Transplant Immunology - Jess - PBL-J-2015
advertisement

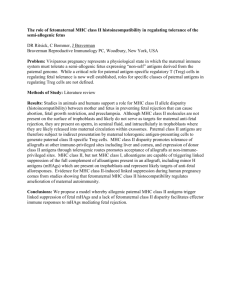
TRANSPLANT IMMUNOLOGY Contents INDICATE, BY REFERENCE TO THE GENETIC MAPPING OF THE HUMAN HLA SYSTEM, THE PROBABILITY OF FINDING HLA IDENTICAL SIBLINGS VERSUS PARENTS AND UNRELATED INDIVIDUALS ........................................... 1 TYPES OF TRANSPLANTATION ................................................................................................................................... 2 UNDERSTAND THE BASIC GENETICS OF TRANSPLANTATION REJECTION, INCLUDING ROLE OF THE MAJOR HISTOCOMPATIBILITY COMPLEX (MHC) GENES AND PROTEINS ............................................................................... 2 UNDERSTAND THE BASIC IMMUNOLOGICAL MECHANISMS OF TISSUE REJECTION.................................................... 3 OUTLINE THE METHODS OF REJECTION PREVENTION ................................................................................................ 3 DISCUSS ASPECTS OF CLINICAL TRANSPLANTATION ................................................................................................. 4 REFERENCES.............................................................................................................................................................. 4 INDICATE, BY REFERENCE TO THE GENETIC MAPPING OF THE HUMAN HLA SYSTEM, THE PROBABILITY OF FINDING HLA IDENTICAL SIBLINGS VERSUS PARENTS AND UNRELATED INDIVIDUALS The MHC gene complex is located on chromosome 6 It is divided into 3 classes MHC Class I ~ A, B, C (E, F, G) MHC Class II ~ DP, DQ, DR (DM, DO) MHC Class III ~ Complement components and some cytokines For MHC Class I There are a HUGE number of antigens possible, thus likelihood of unrelated match is very small In addition, laws of transplantation are similar to those of blood groups: Jess Q – Week 14 – Astro Boy Page 1 Donor A B B AxB Recipient A A AXB B Outcome Accepted Rejected (recipient has antigens for B) Accepted (donor recognises B antigens = no antigens) Rejected (recipient has antigens for A) TYPES OF TRANSPLANTATION UNDERSTAND THE BASIC GENETICS OF TRANSPLANTATION REJECTION, INCLUDING ROLE OF THE MAJOR HISTOCOMPATIBILITY COMPLEX (MHC) GENES AND PROTEINS MHC molecules are membrane proteins on Antigen Presenting Cells that display peptide antigens for recognition by T lymphocytes. MHC was discovered as the genetic locus that is the principal determinant of acceptance or rejection of tissue grafts exchanged between individuals. I.e.: individuals that are identical at their MHC locus (identical twins) will accept grafts from one another, and individuals that differ at their MHC loci will reject such grafts. In all species, the MHC locus contains two sets of highly polymorphic genes (many different allele are present among the different individuals in the population), called class I and class II MHC genes. These genes encode the class I and class II MHC molecules that display peptides to T cells. Jess Q – Week 14 – Astro Boy Page 2 The antigens of allografts (the transplant of an organ or tissue from one individual to another of the same species with a different genotype) that serve as the principal targets of rejection are proteins encoded in the MHC. UNDERSTAND THE BASIC IMMUNOLOGICAL MECHANISMS OF TISSUE REJECTION Three main mechanisms of tissue rejection (N.B: lecture notes add accelerated as a rejection type between hyperacutre and acute, however the text books that I sourced did not include this) 1. - Hyperacute rejection Occurs within minutes of transplantation Is characterised by thrombosis of graft vessel and ischemic necrosis of the graft Cause = preformed anti-donor antibodies and complement Preformed antibodies react with alloantigens (an antigen present in allelic forms encoded at the same gene locus in different individuals of the same species) on the vascular endothelium of the graft, activate complement, and trigger rapid intravascular thrombosis and necrosis of the vessel wall 2. - Acute rejection Occurs within days or weeks after transplantation Is the principal cause of early graft failure Cause = primary activation of T cells CD8+ T lymphocytes reactive with alloantigents on graft endothelial cells and parenchymal cells cause damage to these cell types. Alloreactive (pertaining to the immune response in reaction to a transplanted) antibodies also may contribute to vascular injury. 3. - Chronic rejection An idle for of graft damage that occurs over months or years, leading to progressive loss of graft function Cause = unknown – multiple hypothesis T cells reactive with graft alloantigens may produce cytokines that induce proliferation of endothelial cells and intimal smooth muscle cells, leading to luminal occlusion OUTLINE THE METHODS OF REJECTION PREVENTION Matching Tissue Type - Serological - Cellular - Genetic - PCR-SSP (Sequence Specific Primers) – most commonly used procedure - ABO compatibility - Negative lymphocytic cross-match (class II to reduce rejection) Immunosuppression - Through the use of drugs (the lecture from the example was that azathioprine stopped the division of all immune cells, but also had effects on the gut and RBC; Cyclosporine inhibits the interaction between thelper and cytotoxic cells by inhibiting Il2 Jess Q – Week 14 – Astro Boy Page 3 Immunomodulation - Specific immunosuppression (through the use of antibodies) Autologous transplantation - i.e: skin graft from one section of body to another Tissue Engineering DISCUSS ASPECTS OF CLINICAL TRANSPLANTATION Many aspects to consider!!! Source – living donor or cadaveric Tissue match Type of immunosuppression regime required – eg: Full solid organ immunosuppression regime for kidney, not required for autologous grafts How long has organ been out of donor body? Prognosis Size of organ Best notes are in the lecture slides REFERENCES Lecture “Transplant Immunology” Abbas, A., & Litchtman, A. (2011). Basic Immunology (3rd Edition). Philadelphia: Saunders Elsevier. Jess Q – Week 14 – Astro Boy Page 4