neonatal fever
advertisement

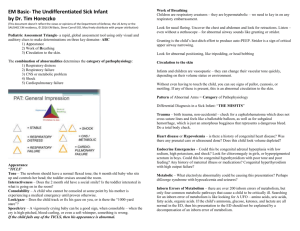
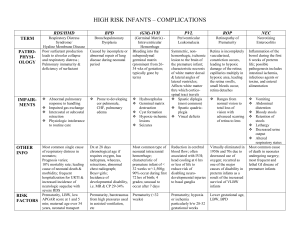
NORMAL NEWBORN • Perinatal period: 28th wk AOG upto 7th day after birth • Neonatal period: 1st 28 days after birth – Very early: birth to <24 hrs – Early: birth to <7 days – Late: 7 days to <28 days • Infancy: 1st year after birth • Mortality is highest during the 1st 24 hr after birth. • Neonatal mortality accounts for 2/3 of all infant deaths (deaths < 1yr of age). Major Causes of Perinatal and Neonatal Mortality FETAL • Placental insufficiency • Intrauterine infection • Severe congenital malformations (anomalies) • Umbilical cord accident • Abruptio placentae • Hydrops fetalis PRETERM • Severe immaturity • Respiratory distress syndrome • Intraventricular hemorrhage • Congenital anomalies • Infection • Necrotizing enterocolitis • Bronchopulmonary dysplasia FULL TERM • Congenital anomalies • Birth asphyxia • Trauma • Infection • Meconium aspiration pneumonia • Persistent pulmonary hypertension Ten Leading Causes of Infant Mortality in the Philippines (DOH, 2009) 1. Bacterial sepsis of newborn 2. Pneumonia 3. Respiratory distress of newborn 4. Disorders related to short gestation and low birthweight, not elsewhere classified 5. Congenital malformations of the heart 6. Congenital pneumonia 7. Neonatal aspiration syndrome 8. Diarhea and gastroenteritis of presumed infectious origin 9. Other congenital malformations 10. Intrauterine hypoxia and birth asphyxia Physical Examination of the Newborn • Requires patience, gentleness and procedural flexibility • Ideally done 2-3x prior to discharge: Immediately after birth Within 24 hours of birth – Prior to discharge, preferably in the presence of the mother • Vital signs – Monitored every 30 mins after birth for 2 hrs or until stable – HR (N 120-160 bpm), vagal slowing may be noted (upto 80 bpm in postdated infants, reassuring if w/ good acceleration on stimulation) – RR (N 30-60 breaths/min), short pauses(5-10secs) considered normal – Apnea: cessation of breathing >20 secs or any duration if accompanied by cyanosis and bradycardia – Pulse oximetry- to screen for PDAdependent CHD – Blood pressure- not routine, SBP gradient bet upper and lower ext >10mmHg suspect CoA – Temp N 36.4-37⁰C (axillary) • Anthropometrics – Head circumference(occipitofrontal circumference):N 35cm in term infants – Weight: SGA- BW<10th percentile Symmetric SGA Asymmetric SGA Onset: early in Onset: late in gestation gestation Brain size corresponds No or minimal with body size effects on fetal brain growth Causes: smoking/drugs, small Causes: maternal size, uteroplacental chromosomal insufficiency with anomaly, TORCH, chronic fetal hypoxia metabolic d/o – AGA- BW between 10th-90th percentile – LGA- BW >90th percentile,↑risk for perinatal asphyxia, RDS, hypogly – Length • General appearance – Physical activity (active and passive tone, posturing) – Ankle or jaw myoclonus/ jitteriness: common in newborns, usually during active mov’t – Vs. convulsive twitching: abnormal, during quiet state – Edema: generalized (prematurity, hypoproteinemia sec to severe erythroblastosis fetalis, nonimmune hydrops, congenital nephrosis, Hurler syndrome) vs. localized (silver nitrate irritation of the eyelid, lymphatic malformation, Turner syndrome) • Skin – Signs of vasomotor instability: purple lividity while crying, acrocyanosis (harmless), mottling (may be assoc w/ serious illness/ transient fluctuation in skin temp) – Harlequin color change: Extraordinary division of the body (pale- red) from forehead to pubis; transient, harmless, speculated pathogenesis: temporary imbalance in tone of cutaneous BVs sec to hypothalamic immaturity, must not be confused with harlequin fetus-severe and uncommon form of ichthyosis manifesting with large plate-like scales and fissures Salmon Patch (Nevus Simplex) – – – Port Wine Stain small, pale pink, ill macular, sharply defined, vascular circumscribed, macules pink to purple, larger usually symmetric unilateral glabella, eyelids, upper lip, and nuchal head and neck area represent mature represent localized dilated dermal vascular ectasia capillaries persist for months, permanent most eventually fade – Cyanosis: high hgb content + thin skin; becomes pale with blanching(unlike ecchymosis) also used in demonstrating icterus – Pallor (Hct<42%): anemia, asphyxia, shock, edema, postterm – Plethora (Hct>65%): polycythemia – Preterm: gelatinous and translucent skin, lanugo – Post-term: peeling, parchment-like (ichtyosis congenita) – Sebaceous hyperplasia: minute, profuse, yellow-white papules representing hyperplastic sebaceous glands; forehead, nose, upper lip, and cheeks;diminish gradually and disappear within the first few weeks – Cutis marmorata: evanescent, lacy, reticulated red/blue vascular pattern over most of the body surface at low temp; represents an accentuated physiologic vasomotor response that disappears with increasing age – Mongolian spots: slate-blue, welldemarcated pigmented areas among blacks, native Americans&Asians, tend to disappear within the 1st year – Milia: tiny sebaceous retention cysts, whitish, pinhead-sized, chin, nose, forehead and cheeks, disappear w/in a few wks – Erythema toxicum: benign,1-3 days after birth, lasts upto 1st wk, eosinophils, face, trunk, extremities – Miliaria crystallina: noninflammatory, pinpoint clear vesicles, profuse eruption over large areas, brawny desquamation upon healing Pustular melanosis: benign, neutrophils, present at birth, lasts 2-3 days, chin, neck, back, extremities, palms or soles Amniotic bands: may be due to amniotic membrane rupture or vascular compromise w/ fibrous band formation Vernix: spontaneously shed w/in 2-3 days • Skull Molding (esp. if normal firstborn cephalic delivery)- temporary skull asymmetry; rpt HC after a few days Cranial synostosis: hard nonmovable ridge over the suture Anterior fontanel:diamond-shaped, 46cm at birth,usually closes at 9-18mos Persistently large anterior fontanels (N= 20±10mm): can be secondary to achondroplasia, Apert syndrome, cleidocranial dysostosis, congenital rubella sydrome, HCP, IUGR, osteogenesis imperfecta, prematurity, Trisomy 13, 18, 21, Vit D deficiency Persistently small fontanels: microcephaly, craniosynostosis, congenital hypothyroidism, wormian bones (intersutural bone formation) Posterior fontanel may be closed at irth or admits tip of finger till 2-4 mos 3rd fontanel: trisomy 21, preterm Craniotabes: soft areas in parietal bones at the vertex near the sagittal suture; common in preterms exposed to uterine compression, resolve in wks Aplasia cutis congenita: atrophic or alopecic scalp, sporadic or AD, assoc w/ Trisomy 13, chromosome 4 deletion, or Johanson-Blizzard syndrome Caput succedaneum: diffuse, ±ecchymosis, soft tissue swelling from the vertex delivery, occipital/parietal, crosses suture lines, resolves in 1-2 days Cephalohematoma: more tense, no discoloration, subperiosteal bleeding assoc w/ instrumented vaginal birth, parietal,do not cross suture lines, may not be visible at birth(slow process), resolves in 2wks to 3mos, may contribute to jaundice Subgaleal hemorrhage: very loose, soft swelling, bleeding under the aponeurosis of occipitofrontalis muscle, assoc w/ vacuum extractions, linear skull fracture, suture diastasis and/or rupture of the emissary vein, nape to forehead, closely monitor for poss extensive bleeding in large potential space, resolves in 2-3 wks • Face Moebius syndrome: symmetric facial palsy sec to absence or hypoplasia of CNVII nucleus • Eyes Often spontaneously open when held up and tipped gently Retinal hemorrhages: common w/ vacuum-assisted deliveries, resolve by 2-4 wks Pupillary reflex: begins 28-30 wks AOG Congenital glaucoma: cornea>1cm in term infant, photophobia, tearing Leukokoria: tumor, chorioretinitis, retinopathy of prematurity, or a persistent hyperplastic primary vitreous • Mouth Precocious dentition- normally shed before eruption of deciduous teeth, assoc w/ Ellis-van Creveld, HallermanStreiff and other syndromes Cleft palate- excessively high arch, bifid uvula Epstein pearls- accumulation of epith cells on hard palate, retention cystsaccumulation of epith cells on gums, ankyloglossia- tongue-tied, short frenulum, sucking callus- labial tubercle which disappears when suckling ceases • Ears/Nose Preauricular sinus, pits, skin tags Alar flaring: dec in airway resistance Choanal atresia: assessed by free passage of NGT through both nares • Neck SCM lesions: hematoma (traumatic) or fibrosis (fixed posistioning in utero) Congenital torticollis: head turned toward, face turned away from affected side, may cause plagiocephaly, facial asymmetry, and hemihypoplasia if untreated Redundant skin/webbing in a female: intrauterine lymphedema, Turner Syndrome Thyroglossal and branchial arch sinus tracts MC neck masses in the NB are vascular malformations, abnormal lymphatic tissue, teratomas, cystic hydromas and dermoid cysts • Lungs Breathing is entirely diaphragmatic Grunting: self-generated PEEP, sign of potentially serious cardiopulmonary distress/sepsis. if benign resolves bet 30-60min after birth Intercostal retractions: compensation for chest wall stabilization Lung shounds are more bronchial than vesicular due to better transmission of large airway sounds across a thin chest • Heart Palpate PMI and auscultation to determine heart location SVT: >220 beats/min Systolic murmurs may be heard transiently in normal NB as ductus arteriosus is closing (flow murmurs) or w/ mild pulmonary branch stenosis Diastolic murmurs should always be considered abnormal Suspect CHD in (1)persistent murmurs, (2)O2sat < 96% after 24 hrs, (3) failed hyperoxia test- arterial PO2<100 after giving 100% inspired O2 w/o clear-cut lung dse, or consider structural heart dse w/ complete intracardiac mixing if pO2 bet 100-250 • Abdomen/ Genitalia Liver usually palpable 2cm below rib margin; Spleen palpable at tip of costal margin Rectal gas should be present by 24 hrs of age Diastasis recti:separation of rectus abdominis into R and L sides Omphalocele:midline, intestines covered w/ peritoneum, assoc w/ Beckwith-Wiedemann, conjoined twins, trisomy 18, meningomyelocele, and imperforate anus vs. gastroschisis: lateral, uncovered Unusual masses: usually renal in origin Cystic: hydronephrosis, multicysticdysplastic kidneys, adrenal hemorrhage, hydrometrocolpos (sec to imperforate hymen), intestinal duplication, and choledochal, ovarian, omental, or pancreatic cysts Solid: neuroblastoma, congenital mesoblastic nephroma, hepatoblastoma, and teratoma Renal vein thrombosis: solid flank mass, hematuria, HTN, thrombocytopenia, assoc w/ polycythemia, dehydration, maternal DM, asphyxia, sepsis, nephrosis, hypercoagulable state Omphalitis: acute periumbilical inflamm, may cause portal HTN Single umbilical artery: occult renal anomaly Severe hypospdias/epispadias: suspect adrenogenital syndrome Stretched penile length <2.5cm is abnormal and requires evaluation Hydrocele: transilluminating scrotal mass, collection of peritoneal fluid due to patency of processus vaginalis in fetal life, monitored to ensure resolution by the 1st yr of life If the testis has not descended by 4 mo, it will remain undescended. Voiding w/in 1st 24 hrs, passage of meconium w/in 48 hrs (does not rule out imperforate anus) • Extremities Crepitus or “step-off” deformity: consider clavicular fracture (most common fracture in NB)or nerve injury Polydactyly; syndactyly; simian crease; talipes equinovarus (clubfoot)foot turned inward and downward, sole directed medially; metatarsus varus- adduction of forefoot, usually corrects spontaneously Barlow maneuver: assesses the potential for dislocation of a nondisplaced hip; performed with the patient's knees and hips flexed, with the thigh in adduction, the examiner applies a posteriorly directed force. Positive Barlow maneuver Ortolani maneuver: causes reduction of dislocation Positive Ortolani maneuver Hip clicks: high-pitched, usually originate in the ligamentum teres or occasionally in the fascia lata or psoas tendon, do not indicate a significant hip abnormality (vs “hip clunks” of hip dislocation). Midline sacral dimpling: common finding, need no further eval unless high-risk for spinal dysraphism (deep, larger than 0.5cm, located > 2.5cm from anal verge, assoc with other cutaneous markers) Fetal neuromuscular disease: assoc w/ breech, polyhydramnios, failure to breathe, pulmonary hypoplasia, dislocated hips, undescended testes, thin ribs, and clubfoot Neurologic examination • Level of alertness-evaluate in both sleep and wakeful states • Cranial nerve exam is largely by observation CN I:rarely tested, functional by 57mos CN II:visual fixation on human face, (+)glare, pupillary response, tracking, optic disc is light pink/pale gray CN III,IV,VI: Doll’s eye maneuver to check for conjugate eye movt, may be disconjugate at birth; ptosis (CN III), pupillary reactivity seen in neonates >32wks AOG CN V: facial sensation w/ rooting reflex, corneal reflex, grimace/ change in CR or RR w/ tactile stimulation V1-3 CN VII: check facial symmetry at rest and upon movt(e.g. crying) CN VIII gross hearing, blink/startle w/ noise CN IX,X,XII: intact if with good sucking (CN V,VII,XII), swallowing (CN IX,X), gag reflex (CN IX,X),tongue movt (XII) CN XI: flexion and rotation of head • Motor Exam: posture- normal term NB have a flexor attitude, preterms lie in extension; tone- tested via traction response(pulling from supine to prone position) if hypotonic, will show severe head lag, strength-check symmetry of spontaneous mov’t • Deep Tendon Reflexes: use index or middle fingers; unsustained ankle clonus(upto 10 beats) is normal • Primitive Reflexes: Moro: carrying baby by his back and “dropping” onto hand causes extension followed by flexion of upper limbs, present from birth-5mos Grasp: stroking ulnar side of the palm causes hand grasp, applying pressure on ball of the foot causes toe grasp, present from birth to 6mos(palmar) or 9-10mos(plantar) Rooting/Sucking: stroking angle of mouth causes sucking, birth to 3 mos Tonic neck: turning head sidewise will cause “fencing posture” towards direction of head, birth (welldeveloped at 1 month) upto 5-6 mos • Sensory Exam: gross response to stroking, withdrawal, crying, grimace Neonatal Resuscitation Pearls • Primary apnea: no spontaneous respiration at birth but rapidly responds to tactile stimulation • Secondary apnea: no spontaneous respiration despite 2 attempts at tactile APGAR Scoring Heart rate 0 Absent 1 Below 100 2 Over 100 Respiratory effort Absent Slow, irregular Good, crying Muscle tone Limp Active motion Response to catheter in nostril (tested after oropharynx is clear) Color No response Some flexion of extremities Grimace Body pink, extremities blue Completely pink Blue, pale Cough or sneeze stimulation • ET size: <1 kg= 2.5 uncuffed 1-2 kg= 3 uncuffed 2-4 kg= 3.5 uncuffed • ET depth: Wt(kg)+6; for nasal intubation, add 2cm • Epinephrine: for asystole or severe bradycardia 1:10,000 0.1mg/ml Dose: 0.01-0.03mg/kg IV 0.03-0.1mg/kg IT • Naloxone: for narcotic depression Dose: 0.1-0.2mg/kg APGAR Scoring • 0-3 requires immediate resuscitation • not designed to predict neurologic outcome • Low Apgar scores (0-3 at 5 mins) and umbilical artery blood pH predict neonatal death • False Positive [(-) acidosis but ↓APGAR]: Prematurity Analgesics, narcotics, sedatives MgSO4 Acute cerebral/SC trauma Precipitous delivery Congenital myopathy/neuropathy Lung anomaly/ airway obstruction Pneumonia/sepsis Hemorrhage-hypovolemia • False Negative [(+) acidosis but normal APGAR]: Maternal acidosis High fetal catecholamines Full term Thermoregulation • Body surface is 3x that of an adult • Rate of heat loss is 4x that of an adult; occurs via convection, conduction and radiation, evaporation • Mechanism of heat production inc metabolic rate and O2 consumption release of norepi oxidation of brown fatnonshivering thermogenesis inc muscular activity hence hypoxemic, hypoglycemic and sedated NB will not be able to thermoregulate effectively • Skin-to-skin contact is the optimal method of thermoregulation Other delivery room initial care • Silver nitrate (1%), erythromycin (0.5%) or tetracycline (1%) ophthalmic ointments to protect against gonococcal ophthalmia neonatorum • 1mg of water-soluble phytonadione (Vit K1) IM to prevent hemorrhagic dse of the NB • Hep B vaccine for >2kg • Newborn screening: CH, galactosemia, CAH, G6PD deficiency, PKU, maple syrup urine disease • Hearing screen Nursery Care • Criteria for early discharge (<48 hrs): uncomplicated antepartum, intrapartum, postpartum courses, vaginal delivery, singleton, completed 37wks, AGA, RR<60, CR 100-160, axillary temp 36.5-37.4C, normal PE, urination and stool x 1, at least 2 uneventful, successful feedings, (-)jaundice w/in 24 hrs, good parental educability and ability, normal labs/screening, no social risks • If discharged <48 hrs after delivery, follow up examination of the NB must be made within 48 hrs of discharge Breastfeeding • Baby-Friendly Hospital Initiative (WHO/UNICEF, `989) 10 steps to successful breasfeeding: 1. Have a written breast-feeding policy that is routinely communicated to all health care staff. 2. Train all health care staff in the skills necessary to implement this policy. 3. Inform all pregnant women about the benefits and management of breastfeeding. 4. Help mothers initiate breast-feeding within a half hour of birth. 5. Show mothers how to breast-feed and how to maintain lactation even if they should be separated from their infants. 6. Give newborn infants no food or drink other than breast milk unless medically indicated. 7. Practice rooming-in (allow mothers and infants to remain together) 24 hr a day. 8. Encourage breast-feeding on demand. 9. Give no artificial teats or pacifiers to breast-feeding infants. 10. Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic. • Drugs and breastfeeding Less likely to affect neonate: weak acids, composed of large molecules, plasma bound, poorly absorbed Contraindicated: anti-neoplastics, drugs of abuse, bromocriptine, chloramphenicol, clozapine, methimazole Avoid/give w/ caution: alcohol, amiodarone, ASA, atropine, Bblockers, ciprofloxacin, phenobarbital NEONATAL FEVER • Definition of neonatal fever: rectal temperature of 38ºC (100.4ºF) • Causes: Environmental (e.g. overbundling) unbundle and retake temp after 15-30 mins. If rpt temp is normal in a healthy-appearing infant w/o antipyretic, the infant may be considered afebrile Dehydration Rochester Criteria for Identifying Febrile Infants at Low Risk for Serious Bacterial Infection Infant appears generally well Infant has been previously healthy: Born at term (≥37 weeks of gestation) No perinatal antimicrobial therapy No treatment for unexplained hyperbilirubinemia No previous antimicrobial therapy No previous hospitalization No chronic or underlying illness Not hospitalized longer than mother White blood cell count of 5-15,000 per mm3 Absolute band cell count of ≤1,500 per mm3 Ten or fewer white blood cells per high-power field on microscopic examination of urine Five or fewer white blood cells per high-power field on microscopic examination of stool in infant with diarrhea Vaccine reaction • If these are ruled out, serious infection (pneumonia, bacteremia, meningitis, viral infection esp HSV or enteroviruses) can be considered, although such infections often occur w/o fever, and may even present w/ hypothermia (rectal temp <36ºC) • Neonates who have a fever and do not appear ill have a 7% risk of having a serious bacterial infection • Toxic appearing infants: defined as a clinical picture consistent w/ the sepsis syndrome (e.g. lethargy, signs of poor perfusion or marked hypoventilation, hyperventilation or cyanosis) • Mainly at risk for late-onset neonatal bacterial diseases (group B streptococci, Escherichia coli, and Listeria monocytogenes) and perinatally acquired herpes simplex virus (HSV) • Diagnostics: CBC, UA, BCS, UCS, CSF CS/GS glucose and protein levels, HSV and enterovirus polymerase chain reaction should be considered, ±stool culture and CXR • Under most circumstances, all febrile infants < 28 days of age, including those in the lowrisk group,should have a sepsis evaluation and be hospitalized for parenteral antimicrobial therapy (e.g. Ampicillin+ Gentamicin) pending culture results. • Acyclovir if HSV infection is suspected(CSF pleocytosis or known maternal history of genital HSV) • Alternative management (for low-risk infants <28 days): complete sepsis evaluation, hospitalization, careful observation w/o parenteral antimicrobial therapy pending culture results. References: • http://www.doh.gov.ph/kp/statistics/infant_deaths.html • Nelson’s 19th ed • Manual of Neonatal Care 7th ed by Cloherty et al • Guide for History Taking, Physical Examination and Diagnosis of Pediatric Patients 2nd ed UST Dept of Pediatrics • Baraff LJ, Bass JW, Fleisher GR, Klein JO, McCracken GH, Powell KR, et al. Practice guideline for the management of infants and children 0 to 36 months of age with fever without source. Pediatrics. 1993;92:1–12. • Luszczak, M. 2001. Evaluation and Management of Infants and Young Children with Fever. Am Fam Physician. 64(7):1219-1227.