AktinPaperBCRT - University of Aberdeen
advertisement
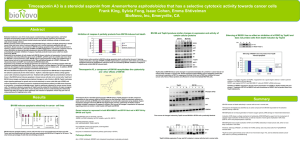
Early changes in [18F] FDG incorporation by breast cancer cells treated with trastuzumab in normoxic conditions: Role of the Akt-pathway, glucose transport and HIF-1α Ian N Fleming, Alexandra Andriu, Tim A D Smith* Division of Applied Medicine, School of Medicine and Dentistry, University of Aberdeen, Foresterhill, Aberdeen AB24 2TN UK *Corresponding author: Dr Tim A D Smith Biomedical Physics Building School of Medicine and Dentistry University of Aberdeen Foresterhill Aberdeen AB24 2TN United Kingdom +44 1224 553208 +44 1224 552514 t.smith@abdn.ac.uk Running title: Trastuzumab and [18F]FDG incorporation Word count 4986 Funding: University of Aberdeen and Friends of Anchor 1 Abstract Purpose: HER-2 overexpression doesn’t guarantee response to HER2-targeting drugs such as trastuzumab, which is cardiotoxic and expensive, so early detection of response status is crucial. Factors influencing [18F]FDG incorporation in the timeframe of cell signalling down-regulation subsequent to trastuzumab treatment are investigated to provide a better understanding of the relationship between growth response and modulation of [18F]FDG incorporation. Methods: HER-2-overexpressing breast tumour cell lines, MDA-MB-453, SKBr3 and BT474 and MDAMB-468 (HER2 non-over-expressor) treated with trastuzumab (4h) and probed for AKT, pAKT, ERK1/2, pERK1/2 and HIF-1α to determine early signalling pathway inhibitory effects of trastuzumab. Cells incubated with trastuzumab and/or PI3K inhibitor LY294002 and ERK1/2 inhibitor U0126 and glucose transport and [18F]FDG incorporation measured. Results: Cell lines expressed AKT, pAKT, ERK1/2 and pEKR1/2 but not HIF-1α. Trastuzumab treatment decreased pAkt but not pERK1/2 levels. Trastuzumab did not further inhibit AkT when maximally inhibited with LY294002. Treatment with LY294002 and trastuzumab for 4h (and 72h with trastuzumab) decreased [18F]FDG incorporation in BT474 and MDA-MB-453 but not SKBr3 cells. LY294002 inhibited glucose transport by each cell line but glucose transport rate was 10 fold higher by SKBr3 cells than BT474 and MDA-MB-453 cells. Akt–induced uptake of [18F]FDG was found to be HIF-1α independent in breast cancer cell lines. Conclusion: AKT inhibition level and tumour cell glucose transport rate can influence whether or not PI3K inhibitors affect [18F]FDG incorporation which may account for the variation in preclinical and clinical findings associated with [18F]FDG-PET in response to trastuzumab and other HER-2 targeting drugs. Key words: [18F]FDG; glucose transport; PI3/AKT; trastuzumab 2 Introduction Breast cancer, the most common cancer in women, is the primary cause of death amongst women in the United States(1). However the development of targeted biological therapies that down-regulate growth factor pathways are improving breast cancer prognosis for many women, particularly drugs like trastuzumab that target the human epithelial growth factor receptor (HER) family. Intracellular signalling pathways are frequently up-regulated in cancer. Many well-established anticancer drugs block signalling via a particular pathway. However due to cross talk and feedback mechanisms inhibition of one signalling pathway can be compensated by up-regulation of another. The Phosphatidylinositol 3 kinase(PI3K)/protein kinase B (AKT) pathway, which is associated with growth, proliferation and survival(2), is one of the most commonly upregulated signalling pathways in breast cancer. Signalling in the PI3K/AKT pathway is activated by PI3K catalysed conversion of phosphatidylinositoI-4, 5-bisphosphate (PIP2) to phosphatidylinositol-3’, 4’, 5’- trisphosphate (PIP3). AKT activity is tightly controlled by the phosphatase, PTEN which converts PIP3 back to PIP2. Overactivation of PI3K/AKT signalling in cancer is a consequence of activating mutations of PI3K or AKT, deactivation of PTEN or overexpression of tyrosine kinase receptors which are upstream of PI3K/AKT(3). The HER family includes the EGFR (or HER1), and the target of trastuzumab, HER2 as well as HER3 and HER4. Ligand binding with HER1, 3 or 4 (HER2 is constitutively activated) permits interaction with another ligand-activated receptor member of the HER family forming homo- or hetero-dimers facilitating activation of intracellular tyrosine kinase domains. Activated dimers possess binding sites for components of the mitogen-activated protein kinase (ERK) and AKT signalling pathway e.g. PI3K, binding to which induces signalling through the PI3K/AKT pathway. Thus HER3 has several PI3K binding sites and when it forms dimers with HER2 is a strong activator of PI3K(4). HER2overexpressing tumours consequently exhibit increased activity of downstream AKT. 3 Between 15 and 25% of primary invasive breast cancers over-express HER2 which is indicative for treatment with the recombinant humanized monoclonal antibody trastuzumab. Whilst clinical benefit of trastuzumab to many patients with HER2-positive breast cancer is well established, less than 50%(5) receiving trastuzumab as monotherapy respond and even when administered in the adjuvant setting 15% of patients still relapse(6). Trastuzumab is expensive and cardiotoxic(7) so early detection of non-responders is a crucial requirement in oncology. Positron emission tomography (PET) imaging with the glucose analogue, 2-[18F]fluoro-2-deoxy-Dglucose ([18F]FDG-PET) facilitates primary and metastatic cancer detection and therapy response detection. Tumour response is generally associated with decreased uptake of [18F]FDG determined by serial PET scanning although metabolic flare(8) can influence incorporation in some cases. [18F]FDG-PET has demonstrated some utility for assessing response to therapy for a range of targeted anti-cancer agents. Currently there are no specific PET tracers available to quantitate AKT activity but a number of recent studies suggest that [18F]FDG-PET may be a useful modality for detecting response to drugs targeting the AKT pathway(9,10). However rates of glucose utilisation don’t necessarily correspond with activation levels of AKT(11) and response to HER-2-targeting drugs including trastuzumab which functions partly by inhibiting the AKT pathway have not consistently been shown to result in decreased [18F]FDG incorporation(12,13). A number of factors confound the relationship between level of signalling pathway activation and downstream events, factors that include compensatory up-regulation of parallel signalling pathways e.g. inhibition of ERK increases AKT activity(14). Further the PI3K-AKT signalling pathway influences cell growth through anabolic processes that control glucose metabolism via Hypoxia Inducible Factor 1α (HIF-1α) dependent and HIF1-independent mechanisms which may impact on how inhibition of AKT relates to [18F]FDG incorporation. The purpose of this study is to investigate the relative importance of AKT and ERK signalling inhibition in response to trastuzumab in cells growing under normoxic conditions, the role that the 4 trastuzumab-induced inhibition of the pathways plays in inducing early changes in glucose transport and [18F]FDG incorporation and the involvement of HIF-1α in this process. Three cell lines BT474, MDA-MB-453 and SKBr3 which we have previously shown to be sensitive to trastuzumab (15) were employed. To demonstrate the relative insensitivity of these processes to trastuzumab in cells that do not overexpress HER2, MDA-MB-468, was also used. Materials and Chemicals [18F]FDG was synthesised by the University of Aberdeen’s PET facility. LY294002 and U0126 were from Cambridge Biosciences (UK). Trastuzumab (Roche) was purchased from the Pharmacy at Aberdeen Royal Infirmary and used at a concentration of 5μg/ml which is above that at which the growth inhibitory drug effect reaches a plateau(15). All other chemicals were from Sigma-Aldrich (Poole UK) unless otherwise stated. Cell culture All cells were cultured in Dulbecco’s Modified Eagle Medium (Gibco, Life Technologies Ltd, Paisley UK) supplemented with penicillin (100units/ml) and streptomycin (100µg/ml) and 10% fetal bovine serum (Gibco). BT474, SKBr3 and MDA-MB-453 cell lines were purchased from the American Type Cell Collection. BT474 and MDA-MB-453 cells exhibit mutations in their PIK3CA genes whilst SKBr3 cells have wild-type PIK3CA(16). Cytotoxicity assay (3-(4,5 dimethylythiazol-2-yl)-2,5-diphenyl tetrazolium bromide(MTT)) To determine cell sensitivity to PI3K inhibitor LY294002 and ERK1/2 inhibitor U0126 cells were seeded (5000 cells/well in 100μl) in 96 well plates and exposed to 0.5-50µM concentrations +/trastuzumab (5μg/ml) for 72h at 37oC. Medium then aspirated and 0.2ml of MTT (10%) in medium added per well then left at 37oC for 4h then the MTT aspirated. DMSO (0.2ml) was added to each 5 well to dissolve the formazin crystals and absorbance read at 570nm using a scanning multi-well spectrophotometer (Dynatech MR 5000, Dynatech Laboratories, Chantilly, VA, USA ) after 30s agitation. The readings were analysed using Ascent software. [18F]FDG incorporation To measure [18F]FDG incorporation by cells after different treatments 25cm2 tissue culture flasks were seeded with MDA-MB-453, BT474, MDA-MB-468 or SKBr3 cells (0.5 x 106 cells per flask) in 5ml of medium and allowed to incubate for 3 days at 37oC. One ml of medium containing [18F]FDG (37KBq/ml) was administered to each flask. Incubation was continued for 20min after which the medium was removed from the flasks and the cells washed 5X with PBS (5ml). The cells were then detached by addition of 0.5ml of trypsin (0.05%)/EDTA (0.2%) recovered into microfuge tubes and incorporated [18F]FDG measured using a well counter with a Nuclear Instruments (Oakland UK) interface until >1000 counts accumulated. Cells were then centrifuged at 200g for 5min and the cells suspended in 100μl of NaOH (1M) and left overnight at 37oC. After neutralisation with 100μl of HCL (1M) a protein assay was carried out on the dissolved tissue. The [18F]FDG incorporation was then normalised by dividing by the protein value. [3H]-o-methylglucose (OMG) uptake assay(15) O-methylglucose is transported by glucose transporters but not metabolised. Its initial rate of uptake is a measure of glucose transport. Flasks (25cm2) were seeded with cells and treated in quadruplicate as described for [18F]FDG incorporation experiments. Media was removed from cells and the assay started by adding 1ml of DMEM containing [3H]-OMG (37KBq/ml) at 37oC. After exposure of the cells to [3H]-OMG for 5s or 10s, 5ml of ice-cold PBS containing (200µM) phloretin was immediately added to the flasks and decanted. Three further rapid washes were carried out, prior to cell detachment by trypsinisation and transfer to scintillation vials containing 5ml of Ultima Gold scintillation fluid (Perkin Elmer UK). Cellular [3H] uptake was determined on a Packard (UK) Tri- 6 Carb 2100TR scintillation counter. Radioactive counts were normalised to protein content determined on the cell suspension. Western blot MDA-MB-453, BT474, MDA-MB-468 and SKBr3 cells were seeded at 0.5 x 106 cells/60mm plate and grown for 3 days. Cells were exposed to LY294002 (50µM), trastuzumab (5µg/ml) or LY294002 (50µM) + Trastuzumab (5μg/ml) for 4h. Western blots were performed as described previously(17). Antibodies were sourced from cell signalling (AKT, phospho Ser473 AKT, phospho Thr308 AKT, p44/42 ERK1/2, phospho Thr202/Tyr204 p44/42 ERK1/2), Insight Biotechnology (HER2/neu), DAKO (phosphor-HER2) Becton Dickinson (HIF1α) and Millipore (glut-1). W. blotting was carried out 2 or 3 times in each case and representative blots are shown. Protein assay Protein concentrations determined using the Bicinchoninic acid kit (Sigma-Aldrich UK) according to the manufacturer’s instructions. Absorbance at 562nm were measured on a Helios γ (Thompson Spectronic) UV/Vis spectrophotometer. Statistics Significant differences between means were determined using the Student t-test. All experiments were carried out at least 3 times. Results HER2 expression in the breast cancer cell lines was checked by western blotting. The results (Fig 1A) demonstrated high levels of HER2 expression in BT474 and SKBr3 and medium levels in MDA-MB453 cells and no detectable expression in MDA-MB-468 cells. This agrees with the literature(18), confirming our cell lines have expected expression profiles. The phosphor-HER2 level in MDA-MB453 cells was lower than in BT474 and SKBr3 cells reflecting the lower level of HER-2 in MDA-MB-453 7 cells. Trastuzumab treatment decreased phosphor-HER-2 expression in these three cells lines. Western blotting confirmed all three experimental cell lines contained AKT, pAKT, ERK1/2 and pERK1/2 (Fig 1B and C). AKT and pAKT protein levels were lower in SkBr3 cells compared with the other cell lines, but there was little difference in the intercellular ERK1/2 and pERK1/2 levels. Trastuzumab treatment had no detectable effect on ERK 1/2 phosphorylation (Fig 1B), but modestly decreased pAKT levels in all three HER-2 overexpressing cell lines (Fig 1C) but not in HER-2 negative MDA-MB-468 cells (results not shown). Treatment of cells with LY294002 inhibited their growth (Fig 2). Trastuzumab (5μg/ml) alone (initial point on each curve i.e. where LY294002 concentration is 0) inhibited the growth of each cell line by 30-40%. In combination with trastuzumab (5μg/ml), the growth inhibitory effect of LY294002 at concentrations of up to 5μM, was increased compared with LY294002 alone. However the additive effect is not apparent at higher concentrations of LY294002. MDA-MB-468 cells did not show any decrease in cell number after treatment with trastuzumab (5ug/ml) (results not shown). To further investigate the relationship between PI3K/AKT and trastuzumab cells were treated with a high dose (50μM) of the PI3K inhibitor LY294002. Inhibition of AKT reached a plateau with treatment of doses of LY294002 between 20 and 50μM (results not shown). PI3K inhibitor treatment greatly decreased pAKT (Fig 3A) in each cell line, but did not completely eliminate AKT phosphorylation of Thr308, presumably because phosphorylation is also maintained by other inputs(19). Similar results obtained when Ser473 phosphorylation was studied (data not shown). Combination of LY294002 (50μM) with trastuzumab did not further decrease pAKT levels suggesting that trastuzumab inhibition of pAKT is a consequence of its action via PI3K. Figure 3B shows the incorporation of [18F]FDG by SKBr3, BT474 and MDA-MB453 cells after treatment with trastuzumab (5μg/ml), LY294002 (50μM) or the two combined. Treatment with 5µg/ml trastuzumab or with 50µM LY204002 for 4h significantly decreased [18F]FDG incorporation by BT474 and MDA-MB-453 cells but not SKBr3 cells. Combined treatment of LY294002 with 8 trastuzumab did not further decrease [18F]FDG incorporation by MDA-MB-453 or BT474 cells beyond that of LY294002 indicating that trastuzumab inhibition of [18F]FDG incorporation was via the PI3K/AKT signalling pathway. [18F]FDG incorporation by MDA-MB-453 and BT474 cells treated with LY294002 (1-50μM) was found to decrease in a dose-dependent manner (Fig 3C). In contrast no decrease in [18F]FDG incorporation by SKBr3 cells was observed. FDG incorporation by MDA-MB-468 cells was not significantly decreased by treatment for 4 h with trastuzumab (51088 ± 3844 cpm/mg protein) compared with controls (50735 ± 4230 cpm/mg protein). [18]FDG incorporation was also determined in each HER-2 overexpressing cell line after 72h incubation with trastuzumab. As was the case after 4h incubation with trastuzumab, treatment for 72h with this drug significantly decreased [18F]FDG incorporation by BT474 (62% (±5.8) of control p<0.001) and MDA-MB-453 (77% (±5.7) of control p<01) cells but not SKBr3 (98% (±14) % of control not significant) cells. It is well documented that ERK inhibition can cause upregulation of AKT phosphorylation(14). Each cell line was treated for 4h with the well characterised ERK 1/2 inhibitor U0126(20). As expected, U0126 treatment eliminated all detectable pERK 1/2 in SKBr3 and BT474 cells (Fig 4). Strong pERK downregulation was also observed in MDA-MB-453 cells (Fig 4); some residual pERK was observed in MDA-MB-453 cells, probably due to the very high basal pERK levels. U0126 treatment caused a clear increase in pAKT and an upregulation of total ERK protein levels (Fig 4). U0126 was also found to inhibit the growth rate of MDA-MB-453, SKBr3 and BT474 cells (data not shown). [18F]FDG incorporation was significantly increased in MDA-MB-453 and BT474 cells but not by SKBr3 cells (Fig 4C). HIF1α levels were undetectable in both the control and U0126-treated cells. Glut-1 protein expression was not affected by any of the 4h treatments (figure 3). However glucose transport is also controlled by several post-translational mechanisms so glucose transport was examined at the functional level. The relative levels of glucose transport and the effect of AKT inhibition on glucose transport was determined in each cell line by measuring the rate of uptake of 9 [3H]O-methyl-glucose for the first 5s after addition to the media. To be considered to be a measure of glucose transport it the uptake of OMG mustn’t reach equilibrium during the measurement period so uptake was also measured at 10s for BT474 cells and was significantly (t=4.95, p<0.01) higher than at 5s (we have previously shown this to be the case for SKBr3, MDA-MB-453 and MDA-MB-468 cells(15). Figure 5A shows that whilst the rate of glucose transport is similar for BT474 and MDAMB-453 cells, for SKBr3 cells the rate is much greater. Treatment with LY294002 (50µM) significantly) decreased glucose transport by each cell line corresponding with decreased [18F]FDG incorporation by MDA-MB-453 and BT474 cells. Trastuzumab significantly decreased glucose transport by MDA-MB-453 cells corresponding with decreased [18F]FDG incorporation (figure 5B). Trastuzumab-treatment of BT474 and SKBr3 cells induced small but significant decreases in glucose transport. Glucose transport ([3H]-OMG) was similar in MDA-MB-468 cells treated with trastuzumab for 4h (691 ± 27 cpm/5s/mg protein) compared with untreated cells (731 ± 87 cpm/5s/mg protein). Discussion: The AKT signalling pathway is associated with increases in hexokinase 2 activity, glucose transport and lactic acid production(11,21,22) and constitutive up-regulation of AKT alone has been suggested to account for the switch to aerobic glycolysis exhibited by tumour cells(23). Studies have shown that treatment of cancer cells with the HER-2 targeting antibody trastuzumab for 24h(24) or 72h(25) specifically decrease AKT but not ERK activation. A 4h drug treatment time is considered an appropriate incubation period for drugs to target intracellular pathways(26). Therefore, in this study a 4h drug treatment was employed to determine the early cell signalling associated effects of trastuzumab on glucose transport and [18F]FDG incorporation, rather than the onset of growth inhibitory and cell death associated events exhibited at later time points. In common with studies using longer (25) incubation time decreases in pAKT levels, but not pEKR1/2, was observed after a 4h treatment of HER-2-overexpressing breast cancer cells with trastuzumab. 10 Chan et al(27)demonstrated that knockdown of Skp2, which regulates AKT ubiquitination, crucial in determining the membrane localisation and hence activity of AKT, increases the sensitivity of cancer cells to trastuzumab, an effect countered by introduction of constitutively active AKT. They (27) also showed that AKT activation is a controlling pathway for glucose transporter expression. In this study, glucose transport was significantly decreased by treatment with LY294002 in each cell line. The modest decrease in pAkt induced by trastuzumab suggests that trastuzumab is a relatively poor inhibitor of AKT phosphorylation as previously observed (24). In contrast, the PI3K inhibitor LY294002 eliminated almost all detectable pAKT. Correspondingly glucose transport was significantly inhibited by 50 μM LY294002 but the effect of trastuzumab on glucose transport was less apparent. Although glucose transport (at the functional level) was decreased in SKBr3 cells by both trastuzumab and LY294002, treatment, neither agent decreased [18F]FDG incorporation in this cell line. Even a long exposure (72h) of SKBr3 cells to trastuzumab did not cause a decrease in [18F]FDG incorporation which was evident in both BT474 and MDA-MB-453 cells suggesting that it’s not a short term phenomenon. Palaskas et al (28) showed that PTEN knockdown in SKBr3 cells, which results in high levels of AKT activity, did not significantly influence [18F]FDG incorporation. Here we found that glucose transport was very high in this cell line and unlikely to be rate limiting. Glucose transporter expression is an important factor that influences FDG incorporation. Cells in which AKT is constitutively up-regulated or growth factor stimulated exhibit enhanced membrane glucose transporter expression (29,30). Growth factor withdrawal results in a rapid decrease in cell surface glucose transporter expression (29,30) (within hours). Therefore [18F]FDG incorporation may be unaffected by AKT inhibition in cancer cells, such as SKBr3 cells in which glucose transport is very high. Although some studies suggest that decreased [18F]FDG incorporation predicts response of breast tumours(31) and xenografts (32,33) derived from breast cancer cells, to anti-HER2 treatments, the 11 results from a xenograft study (12) demonstrated that treatment with trastuzumab did not induce detectable changes in [18F]FDG incorporation. In the present study glucose transport was found to be decreased by treatment with trastuzumab in each cell line but only by about 10% in BT474 cells corresponding with a small decrease in [18F]FDG incorporation. LY294002 induced greater inhibition of glucose transport, and in BT474 and MDA-MB-453 cells, of [18F]FDG incorporation than did trastuzumab. Davies et al (34) showed that treatment of BT474 cells with the PI3K inhibitor AZD5363 inhibited growth of xenografts derived from BT474 cells and decreased FDG incorporation after 4h treatment. In some cells in normoxic conditions HIF-1α is involved in the enhanced glycolysis in tumour cells due to its activation by intracellular signalling pathways including PI3K/AKT(35,36) Inhibition of PI3K/AKT in some tumour types including thyroid(37) and prostate cancer(38) can result in HIF1α downregulation and this can act as a mediator of the downstream effects of AKT de-activation(38,39). However, the role of HIF1α in controlling tumour cell glucose utilisation as a function of AKT activation in normoxia is tumour type-dependent. Studies using leukaemic(23) and human bladder cancer cells(40) have shown that up-regulation of AKT does not necessarily result in up-regulation of HIF1α expression or of HIF1α target genes including that of GLUT1. In the three breast cancer cell lines in the present study, which was carried out under normoxic conditions, the downstream effects of AKT inhibition on glucose transport and [18F]FDG incorporation did not appear to be routed through HIF1α. HIF1α protein expression was undetectable in all three cell lines and administration of YC1 to MDA-MB-453 cells at a dose that strongly down regulates HIF1α levels(17) had no effect on [18F]FDG incorporation (results not shown). Treatment of cells with the ERK1/2 inhibitor U0126 increased AKT activation and [18F]FDG incorporation but did not increase HIF1α expression. ERK inhibitors are being explored for the treatment of a variety of ras-activated cancer types. 12 Compensatory changes in AKT activation during treatment with ERK inhibitors have been observed(14). We found that inhibition of ERK with U0126 which was growth inhibitory in each cell line actually increased [18F]FDG incorporation in two cell lines due to an increase in pAKT levels. Inhibition of ERK increases AKT activity and [18F]FDG incorporation and is a potential source of metabolic flare associated with some anti-cancer treatment. The findings of the present study suggest that inhibition of AKT in normoxic cells can result in early changes in [18F]FDG incorporation and that this is independent of HIF-1α. However a number of factors are involved which include the decrease in pAKT levels below a threshold level at least in some cancers before glucose transport is appreciably affected and that glucose transport may need to be a rate limiting factor in [18F]FDG incorporation in that cell line. This may account for the variation in preclinical and clinical findings associated with [18F]FDG-PET in response to trastuzumab and other HER-2 targeting drugs(12,13,32-34). Disclosure The authors declare no conflicts of interest. The work was funding by the University of Aberdeen and Friends of Anchor. We thank Dr Iain Brown, University of Aberdeen, for the generous gift of the anti -pHER2 antibody. References 1) www.cancer.org/cancer/breastcancer/overviewguide/breast-cancer-overview-key-statistics 2) Wong KK, Engelman JA, Cantley LC. (2010) Targeting the PI3K signalling pathway in cancer. Curr Opin Genet Dev 20:87–90. 13 3) Stemke-Hale K, Gonzalez-Angulo AM, Lluch A et al. (2008) An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res.68:6084-6091. 4) Schulze WX, Deng L, Mann M. (2005) Phosphotyrosine interactome of the ErbB-receptor kinase family. Mol. Systems Biol. 1 Article Number: 2005.0008 5) Smith BL, Chin D, Maltzman W, Crosby K, Hortobagyi GN and Bacus SS. (2004) The efficacy of Herceptin therapies is influenced by the expression of other erbB receptors, their ligands and the activation of downstream signalling proteins. Br. J. Cancer 91:1190–1194 6) Nahta R. Esteva FJ. (2006) HER2 therapy - Molecular mechanisms of trastuzumab resistance. Breast Cancer Res. 8: Article Number: 215 7) Slamon DJ, Leyland-Jones B, Shak S et al.(2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N. Eng. J. Med. 344: 783-792 8) Evangelista L, Rubello D, Saladini G. (2012)Can FDG PET/CT monitor the response to hormonal therapy in breast cancer patients? Eur. J. Nucl. Med.Mol. Imag. 39: 446-449 9) Maynard J, Ricketts SA, Gendrin C, Dudley P, Davies BR. (2013) 2-Deoxy-2-[18F]fluoro-D-glucose Positron Emission Tomography Demonstrates Target Inhibition with the Potential to Predict AntiTumour Activity Following Treatment with the AKT Inhibitor AZD5363. Mol. Imag. Biol. 15: 476-485 10) Kelly CJ, Hussien K, Muschel RJ. (2012) 3D tumour spheroids as a model to assess the suitability of [18F]FDG-PET as an early indicator of response to PI3K inhibition. Nucl. Med. Biol. 39: 986-992 11) Robey IF, Stephen RM, Brown KS, Baggett BK, Gatenby RA, Gillies RJ.(2008) Regulation of the Warburg effect in early-passage breast cancer cells. Neoplasia 10: 745-756. 12) Shah C, Miller TW, Wyatt SK et al.(2009) Imaging Biomarkers Predict Response toAnti-HER2 (ErbB2) Therapy in Preclinical Models of Breast Cancer. Clin. Cancer Res. 15:4712-4719 14 13) Janjigian YY, Viola-Villegas N, Holland JP et al. (2013) Monitoring Afatinib Treatment in HER2Positive Gastric Cancer with F-18-FDG and Zr-89-Trastuzumab PET. J.Nucl.Med. 54: 936-943 14) Flores LG, Yeh HH, Soghomonyan S et al. (2013) Monitoring Therapy with MEK Inhibitor U0126 in a Novel Wilms Tumor Model in Wt1 Knockout Igf2 Transgenic Mice Using F-18-FDG PET with DualContrast Enhanced CT and MRI: Early Metabolic Response Without Inhibition of Tumor Growth. Mol. Imag. Biol. 15: 175-185 15) Cheyne RW, Trembleau L, McLaughlin AC, Smith TAD. (2011) Changes in 2-Fluoro-2-deoxy-Dglucose incorporation, hexokinase activity and lactate production by breast cancer cells responding to treatment with the anti-HER-2 antibody trastuzumab. Nucl. Med. Biol. 38:339-346 16) Hollestelle A, Elstrodt F, Nagel JH, Kallemeijn WW, Schutte M (2007): Phosphatidylinositol-3-OH kinase or RAS pathway mutations in human breast cancer cell lines. Mol Cancer Res. 5:195-201 17) Smith TAD, Zanda M, Fleming IN. (2013) Hypoxia stimulates 18F-Fluorodeoxyglucose uptake in breast cancer cells via hypoxia induced factors-1 and AMP-activated protein kinase. Nucl. Med. Biol. 40:858-864 18) Rusnak DW, Alligood KJ, Mullin RJ et al. (2007) Assessment of epidermal growth factor receptor (EGFR, ErbB1) and HER2 (ErbB2) proteins expression levels and response to lapatinab (Tykerb, GW572016) in an expanded panel of human normal and tumour cell lines. Cell. Prolif. 40:580-594 19) Powis G, Ihle N, Kirkpatrick DL.(2006) Practicalities of Drugging the Phosphatidylinositol-3Kinase/Akt Cell Survival Signaling Pathway. Clin Cancer Res. 12:2964-66 20) Davies SP, Reddy H, Caivano M, Cohen P. (2000) Specificity and mechanism of action of some commonly used protein kinase inhibitors. Biochem. J. 351: 95-105 15 21) Lambert CM, Roy M, Robitaille GA, Richard DE, Bonnet S.(2010) HIF-1 inhibition decreases systemic vascular remodelling diseases by promoting apoptosis through a hexokinase 2-dependent mechanism. 88:196-204. 22) Fan YJ, Dickman KG, Zong WX. (2010) Akt and c-Myc Differentially Activate Cellular Metabolic Programs and Prime Cells to Bioenergetic Inhibition. J. Biol. Chem. 285: 7324-7333. 23) Elstrom RL, Bauer DE, Buzzai M et al. (2004) Akt stimulates aerobic glycolysis in cancer cells. Cancer Res. 64:3892-3899. 24) Garrett JT, Sutton CR, Kuba MG, Cook RS, Arteaga CL.(2013) Dual Blockade of HER2 in HER2Overexpressing Tumor Cells Does Not Completely Eliminate HER3 Function. Clin Cancer Res. 19: 610619 25) Normanno N, Campiglio M, De Luca A et al. (2002) Cooperative inhibitory effect of ZD1839 (Iressa) in combination with trastuzumab (Herceptin) on human breast cancer cell growth. Ann. Oncol. 13: 65-72 26) Nguyen QD, Perumal M, Waldman TA, Aboagye EO. (2011) Glucose Metabolism Measured by [F18]Fluorodeoxyglucose Positron Emission Tomography Is Independent of PTEN/AKT Status in Human Colon Carcinoma Cells. Translational Oncol. 4 : 231-238 27) Chan CH, Li CF, Yang WL et al. (2012) The Skp2-SCF E3 Ligase Regulates Akt Ubiquitination, Glycolysis, Herceptin Sensitivity, and Tumorigenesis. Cell 149: 1098-1111 28) Palaskas N, Larson SM, Schultz N et al.(2011) F-18-Fluorodeoxy-glucose Positron Emission Tomography Marks MYC-Overexpressing Human Basal-Like Breast Cancers. Cancer Res. 71: 51645174 16 29) Rathmell JC, Fox CJ, Plas DR, Hammerman PS, Cinalli RM, Thompson CB.(2003) Akt-directed glucose metabolism can prevent Bax conformation change and promote growth factor-independent survival. Mol. Cell. Biol. 23: 7315-7328 30) Wieman HL, Wofford JA, Rathmell JC (2007) Cytokine stimulation promotes glucose uptake via phosphatidylinositol-3 kinase/Akt regulation of Glut1 activity and trafficking. Mol. Biol. Cell. 18 : 1437-1446 31) Kawada K, Murakami K, Sato T et al. (2007). Prospective study of positron emission tomography for evaluation of the activity of lapatinib, a dual inhibitor of the ErbB1 and ErbB2 tyrosine kinases, in patients with advanced tumors. Jpn. J. Clin. Oncol. 37:44-48 32) McLarty K, Fasih A, Scollard DA et al (2009). F-18-FDG Small-Animal PET/CT Differentiates Trastuzumab-Responsive from Unresponsive Human Breast Cancer Xenografts in Athymic Mice. J. Nucl. Med. 50;1848-1856 33) Smith TAD, Appleyard MVCL, Sharp S, Fleming IN, Murray K, Thompson AM.(2013) Response to trastuzumab by HER2 expressing breast tumour xenografts is accompanied by decreased Hexokinase II, glut1 and [F-18]-FDG incorporation and changes in P-31-NMR-detectable phosphomonoesters. Cancer Chemotherapy Pharmacol. 71: 473-480 34) Davies BR, Greenwood H, Dudley P et al. (2012) Preclinical Pharmacology of AZD5363, an Inhibitor of AKT: Pharmacodynamics, Antitumor Activity, and Correlation of Monotherapy Activity with Genetic Background. Mol. Cancer Ther. 11: 873-887 35) Zundel W, Schindler C, Haas-Kogan et. al.(2000) Loss of PTED facilitates HIF-1-mediated gene expression. Genes Dev. 14:391-6 36) Zhong H, Chiles K, Feldser D et al.(2000) Modulation of hypoxia inducible factor-1 alpha expression by the epidermal growth factor/phosphatidylinositol-3-kinase/PTEN/FRAP pathway in 17 human prostate cancer cells; implications for tumor angiogenesis and therapeutics. Cancer Res. 60:1541-5 37) Burrows N, Babur M, Resch J et al. (2011) GDC-0941 Inhibits Metastatic Characteristics of Thyroid Carcinomas by Targeting both the Phosphoinositide-3 Kinase (PI3K) and Hypoxia-Inducible Factor-1 alpha (HIF-1 alpha) Pathways. J. Clin. Endocrinol. Metab. 96: E1934-E1943 38) Majumder PK, Febbo PG, Bikoff R, et al. (2004) mTOR inhibition reverses Akt-dependent prostate intraepithelial neoplasia through regulation of apoptotic and HIF-1-dependent pathways. Nat Med. 10:594–601 39) Bhaskar PT, Nogueira V, Patra KC, Jeon SM, Park Y, Robey RB, Hay N.(2009) mTORC1 Hyperactivity Inhibits Serum Deprivation-Induced Apoptosis via Increased Hexokinase II and GLUT1 Expression, Sustained Mcl-1 Expression, and Glycogen Synthase Kinase 3 beta Inhibition. Mol. Cell. Biol. 29: 5136-5147 40) Jones A, Fujiyama C, Blanche C et al. (2001) Relationship of vascular endothelial growth factor production to expression and regulation of hypoxia-inducible factor -1α and hypoxia-inducuble factor-2 α in human bladder tumors and cell line. Clin. Cancer Res. 7:1263-72 18 19 Figure 1) A) HER2 pTyr1248-HER2 1 2 3 4 5 6 7 8 B) C) Figure 1) (A) HER-2 and phosphor-HER-2 expression inSkBr3 (lanes 1 & 2), BT474 (lanes 3 &4), MDA453 (lanes 5 & 6) and MDA468 (lanes 7 & 8) cell lysates analysed by western blotting (The phosph-HER-2 blot was exposed for 20s (left of line) and 120s (right of line)). B) ERK1/2 and pERK1/2 expression in cell lysates prepared from SkBr3 (lanes 1-4), MDA-MB-453 (lanes 5 & 6), and BT474 cell lysates (lanes 7 & 8). Cells were treated with DMSO (lanes 1, 3, 5 & 7) trastuzumab (5μg/ml) for 4h (lanes 4, 6 & 8), or U0126 (20μM for 4h) (lane 2) and probed with antibodies to ERK 1/2, pERK1/2. (C) AKT and pAKT expression in SkBr3 (lanes 1 & 2), BT474 (lanes 3 & 4), and MDA453 cell lysates (lanes 5-7). Cells were treated with DMSO (lanes 1, 3 & 5), Trastuzumab (5μg/ml) (lanes 2, 4 & 6) or LY294002 (50μM) (lane 7) 20 Cell growth (% control) 120 SKBr3 100 ** 80 ** 60 ** 40 20 0 0 10 20 30 40 50 60 Ly294002 dose (μM) Cell growth (% control) 120 MDA-MB-453 100 ** 80 60 ** 40 * 20 0 0 10 20 30 40 50 60 Ly294002 dose (μM) Cell growth (% control) 120 100 BT474 ** 80 ** * 60 * 40 20 0 0 10 20 30 40 50 60 Ly294002 dose (μM) Figure 2: Sensitivity of MDA-MB-453 (A), SKBr3 (B) and BT474 (C) cells to the PI3K inhibitor, LY294002 with (squares) and without 5μg/ml Trastuzumab (triangles). Cells were exposed to 1, 2, 5, 10, 25 and 50µM concentrations of LY294002 in 96 well plates for 3 days then treated with MTT for 4h and the absorbance at 570nm read in a multi-well spectrophotometer. There were significant differences (*p<0.05, **p<0.001) in cell growth rate between cells treated with LY294002 alone or with trastuzumab (5μg/ml) at concentrations of up to 5μM Ly294002 for SKBr3 and up to 10μM LY204002 for the MDA-MB-453 and BT474 cells. The effect of Trastuzumab alone is also shown (first point on each trastuzumab curve (LY294002 concentration = 0). 21 A) MDA453 BT474 SkBr3 pThr308 AKT AKT glut1 Actin 1 B) 2 3 4 1 2 3 4 1 2 3 4 FDG incorporation (% control) 120 ** 100 ** 80 60 40 ** ** ** ** 20 0 Control FDG incorporation (% control) C) -50 Trastuzumab ** 140 Ly Trast+Ly ** 120 100 80 MDA453 60 SKBr3 40 BT474 20 0 0 50 100 150 LY294002 concentration (μM) Figure 3) (A) Protein lysates prepared from MDA-MB-453, SKBr3 and BT474 cells control (lane 1) trastuzumab (5μg/ml) for 4h (lane 2), LY294002 (50μM) for 4h (lane 3) or trastuzumab and LY294002 (lane 4) were probed with antibodies to PKB, pPKB and actin (B) [18F]FDG incorporation by MDA-MB453 (black columns), SKBr3 cells (white columns) and BT474 (grey columns) in untreated controls, Cells treated with trastuzumab (1µM), Ly294002 (50µM) or trastuzumab+ Ly294002 for 4h. (**significant difference from control at 0.01% probability level) C) [18F]FDG incorporation by MDAMB-453 (diamond), SKBr3 (squares) and BT474 (triangles) cells treated for 4h with 0 to 100 µM LY294002. (C) [18F]FDG incorporation by MDA-MB-453, SKBr3 and BT474 cells treated for 4h with LY294002 (0-100μM). 22 A) pThr308 AKT AK T pThr202/Tyr204 ERK 1/2 P42/44 ERK 1/2 HIF 1 1 2 3 4 5 6 7 B) FDG incorporation (% control) 250 200 ** ** 150 100 50 0 MDA-453 SKBr3 BT474 Figure 4) A) SKBr3 (lanes 1 & 2), BT474 (lanes 3 & 4) and MDAMB453 cells (lanes 5 & 6) were control (lanes 1, 3 & 5) or treated with the ERK 1/2 inhibitor U0126 (lanes 2, 4 & 6) for 4h. Lane 7 (+ve HIF1α control is from lysate from MCF7 cells maintained in 1%O2:99%N2 for 4h). Lysates were probed for ERK, pERK, AKT, pAKT and HIF-1α. B) [18F]-FDG incorporation by MDA-453, SKBr3 and BT474 cells after treatment for 4h with the ERK1/2 inhibitor U0126 (20μM) (black columns) (% untreated cells). [18F]-FDG incorporation was increased in U0126-treated MDA-MB-453 (p<0.001) and BT474 cells ( p<0.02) but not by SKBR3 cells. 23 OMG uptake in 5s (% control) A) 40000 35000 30000 25000 20000 15000 10000 5000 0 B) OMG uptake in 5s (% control) 140 120 100 ** * * ** 80 ** ** 60 ** ** 40 ** 20 0 Control Trast Ly LyT Figure 5) Glucose transport (A) in untreated MDA-MB-453, SKBr3 and BT474 cells expressed as cpm/mg protein and (B) relative to untreated controls by MDA-MB-453 (black columns), SKBr3 (white columns) and BT474 (grey columns) cells treated with trastuzumab (5μg/ml), LY294002 (50µM) for 4h or both. (Significantly different from control: at p<0.05 * or p<0.01 **). 24