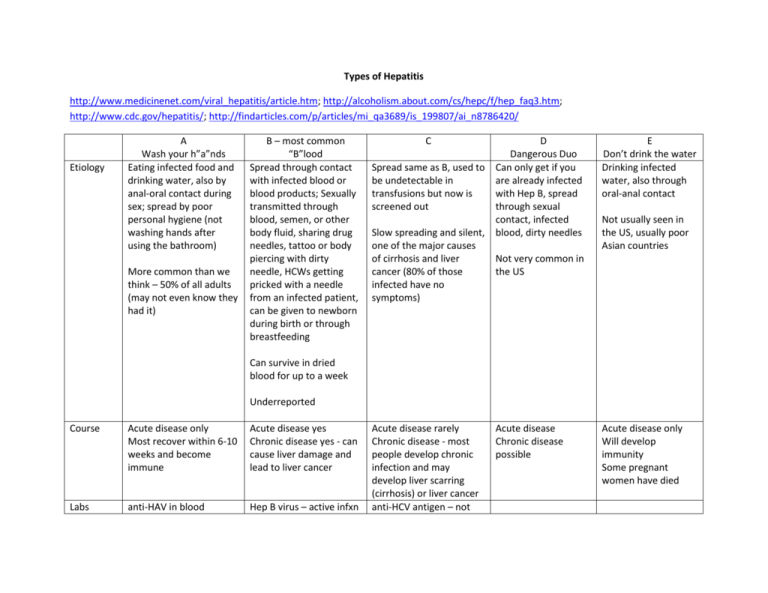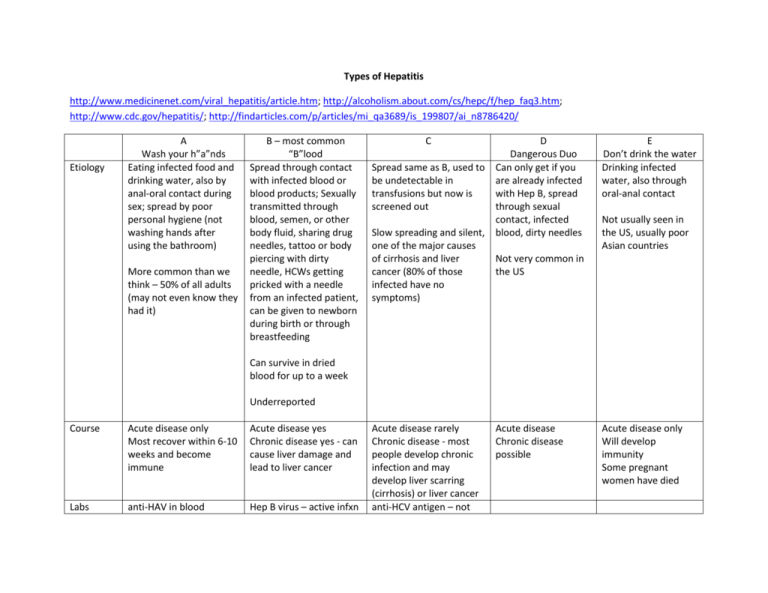
Types of Hepatitis
http://www.medicinenet.com/viral_hepatitis/article.htm; http://alcoholism.about.com/cs/hepc/f/hep_faq3.htm;
http://www.cdc.gov/hepatitis/; http://findarticles.com/p/articles/mi_qa3689/is_199807/ai_n8786420/
Etiology
A
Wash your h”a”nds
Eating infected food and
drinking water, also by
anal-oral contact during
sex; spread by poor
personal hygiene (not
washing hands after
using the bathroom)
More common than we
think – 50% of all adults
(may not even know they
had it)
B – most common
“B”lood
Spread through contact
with infected blood or
blood products; Sexually
transmitted through
blood, semen, or other
body fluid, sharing drug
needles, tattoo or body
piercing with dirty
needle, HCWs getting
pricked with a needle
from an infected patient,
can be given to newborn
during birth or through
breastfeeding
C
D
Dangerous Duo
Spread same as B, used to Can only get if you
be undetectable in
are already infected
transfusions but now is
with Hep B, spread
screened out
through sexual
contact, infected
Slow spreading and silent, blood, dirty needles
one of the major causes
of cirrhosis and liver
Not very common in
cancer (80% of those
the US
infected have no
symptoms)
E
Don’t drink the water
Drinking infected
water, also through
oral-anal contact
Acute disease rarely
Chronic disease - most
people develop chronic
infection and may
develop liver scarring
(cirrhosis) or liver cancer
anti-HCV antigen – not
Acute disease only
Will develop
immunity
Some pregnant
women have died
Not usually seen in
the US, usually poor
Asian countries
Can survive in dried
blood for up to a week
Underreported
Course
Acute disease only
Most recover within 6-10
weeks and become
immune
Acute disease yes
Chronic disease yes - can
cause liver damage and
lead to liver cancer
Labs
anti-HAV in blood
Hep B virus – active infxn
Acute disease
Chronic disease
possible
Prevention Handwashing
2 dose vaccination for all
kids starting at age 1,
travelers to certain
countries, those at risk
Treatment None needed, can get
immune globulin within 2
weeks of contact
Hep B surface antigen –
has active immunity or
current infection
anti-HBC IgM – active
immunity or current
infection
anti-HBs - immune
anti-HBc - past or current
infection
IgM anti-HBc – has been
infected in past 4-6
months
HBeAg - active viral
replication, highly
infectious
HBsAg – active or chronic
hep B
Vaccination for all infants
and adults at risk for HBV
including health care
workers
always accurate
If HBeAg need tx for 4-12
months, if chronic are
also treated for at least
12 months
Use interferon alfa and
antiviral drugs
Interferon alfa-2b,
ribavirin, peginterferon
alfa-2A – combo therapy
No vaccine
No vaccine
No vaccine
Interferon is being
researched
Avoid drinking water
or ice in areas with
bad water quality
Supportive therapy
only
Liver transplantation
Hepatitis G – no vaccine, no treatment, found in Europe, Asia, Australia from tainted injectable drugs, hemodialysis, tattooing or body piercing
Signs & Symptoms including lab values – many don’t know they are infected because they are asymptomatic, flu like symptoms early in the
disease, fever, muscle/joint pain, stomach pain, n/v, fatigue, anorexia, yellowing of skin and eyes, dark urine, light-colored stools, skin rashes
Labs – AST (serum aspartate aminotransferase) and ALT (serum alanine aminotransferase) increase in the prodromal stage of viral hepatitis, ALP
(serum alkaline phosphatase) may increase, serum bilirubin level will be elevated, prothrombin time (PT) will elevate as liver damage increases
(> 3 seconds indicates severe liver damage), WBCs may be elevated
Risk Factors – health care workers, those needing frequent blood transfusions/products, infants born to infected mothers, people with close
contact to infected people, people with many sexual partners, homosexually active males, illegal drug users, those from other countries where
disease is prevalent, prison inmates, Pacific Islanders, Alaskan Natives
Isolation Precautions – Follow standard precautions, don't have to keep most patients with hepatitis in isolation, although patients with hepatitis
A or E and poor hygiene and those who can't cooperate with standard precautions should have a private room. Use contact precautions for
patients with hepatitis A who are diapered or incontinent. Isolation policies vary, depending on the hepatitis type, so check your hospital's
guidelines.
Complications – severe fulminant hepatitis; not knowing you are sick and infecting others; may take weeks/months to recover; liver cancer
Treatment (acute vs chronic) – avoid meds that affect the liver (ie. Tylenol)
Prevention – Change behavior and lifestyle that increase risk, vaccines for some types (don’t work for everyone), ask for testing if you have been
exposed
Hepatitis can also be caused by other viral infections, chemical or drug toxicity, and alcohol abuse; also Hep G, not testable in banked blood, very
mild, rarely even have elevated liver enzymes
Case Study:
New admission
Your patient, 32-year-old Raymond Torres, is admitted with a tentative diagnosis of hepatitis. He's put in a semiprivate room rather than a private one because
he's alert and maintains good hygiene.
During the admission interview, Mr. Torres complains of fatigue, nausea, vomiting, and abdominal discomfort. His vital signs are: pulse, 100; BP, 130/80; and
respirations, 18 (regular). His temperature is 100.4 F (38 degs C), his urine is dark yellow, and the right upper quadrant of his abdomen is distended and
tender. He appears dehydrated and has a dry mouth and poor skin turgor.
Taking his history, you learn that Mr. Torres is a migrant farmworker from Mexico. This makes you first suspect hepatitis A, which is spread enterically in lessdeveloped countries with poor sanitation. That would explain why he has no signs of jaundice, which affects only 10% of patients with hepatitis A.
First, you explain to him the importance of thoroughly washing his hands after he uses the bathroom. Next, as ordered, you start an I.V. infusion of D5W and
0.45% sodium chloride or 0.9% sodium chloride solution at 100 ml/hour following standard precautions. When his vomiting subsides, you start Mr. Torres on a
clear-liquid diet. (Contrary to past practice, disposable dishware and utensils are no longer required for any patients, including those with hepatitis.)
After lab results come back, you find that Mr. Torres has elevated liver function tests and a positive antiHAV IgM antibody. The presence of this antibody
confirms a diagnosis of hepatitis A. (See What Tests Tell You for more on how lab tests are used to make a diagnosis.) Hepatitis A needs to be reported to the
public-health department, as required by law. You'd follow the procedure outlined in your hospital's policy on reportable diseases. Although the Centers for
Disease Control and Prevention reports only hepatitis A, B, and C, your local health department may require reporting of all types of hepatitis.
When Mr. Torres's wife visits, you learn that her husband frequently prepares meals for the family. Because hepatitis A can be spread through contaminated
food, you advise his wife to consult with their physician for testing. You also stress the importance of good hand-washing practices and emphasize that family
members need to wash their hands after visiting or caring for Mr. Torres.
Fortunately, Mrs. Torres and her children test negative for hepatitis A. Although a vaccine is now available to prevent hepatitis A, it has to be given about 1
month prior to possible exposure; the vaccine won't help the family now. However, Mr. Torres's family can be given passive immunity with injections of immune
globulin (formerly called immune serum globulin or gamma globulin). Their physician recommends that each of them receive an injection (0.02 ml/kg
intramuscularly) as a precaution. This injection must be given within 2 weeks of exposure to be effective. It's not effective for hepatitis prophylaxis if 6 weeks
or more have elapsed since exposure.
Treating hepatitis A
Drug therapy isn't indicated for hepatitis A; therapy is supportive only and Mr. Torres will stay less than 24 hours. You tell him and his family that when Mr.
Torres goes home, he should rest, although he can get up to go to the bathroom and take occasional short walks.
You provide a meal plan that's high in carbohydrates and low in fat. Mr. Torres tells you that he doesn't have much appetite, so you suggest small but frequent
meals. You also advise him not to drink alcohol until his physician says he can-most likely in several months, after liver function tests are back to normal.
Finally, you arrange for him to see his physician and receive regular liver function tests-he'll need them for 6 months up to a year.
Patients with any type of hepatitis must be careful with prescription and over-the-counter (OTC) drugs because hepatic dysfunction slows down metabolism.
Medications can damage the liver or reach toxic levels if they're not metabolized properly. In some cases, however, a patient might receive drugs to treat
occasional nausea, pain, or insomnia. Tell the patient to consult the physician or pharmacist before taking any OTC drugs.
Treating hepatitis B
Now, let's look at a patient with hepatitis B. Nancy Williams, 28, is admitted from the emergency department with vomiting, vague abdominal discomfort, dark
urine, anorexia, pruritus, and jaundice. Her vital signs are: pulse, 82; BP 110/60; respirations, 14 (regular). Her temperature is 98.6 degs F (37o C).
During the admission assessment, she tells you that she's the mother of two children and works part-time. Divorced, she's been dating a man for the past 4
months. She tells you that he sometimes uses I.V. drugs.
Ms. Williams's lab tests show the following:
HBsAg-positive
anti-HBs-negative
anti-HBc-positive.
The two positive results indicate that Ms. Williams is in the acute phase of a hepatitis B infection. The lack of anti-HBs shows that her immune system hasn't
produced hepatitis B antibodies.
Her liver function tests are as follows:
Alanine aminotransferase (ALT) is elevated at 1,760 international units/ liter (normal range: 5 to 35 international units/liter). This test is more specific for
hepatitis-induced liver damage than the other tests.
Aspartate aminotransferase is elevated at 1,216 international units/ liter (normal range: 5 to 40 international units/liter).
Lactate dehydrogenase is elevated at 607 international milliunits/ml (normal range: 90 to 200 international milliunits/ml).
Total bilirubin is elevated at 7.1 mg/dl (normal range: 0.1 to 1 mg/dl).
Although individual values are important, following the trends and knowing when the values peak and start to decline gives you the best insight into your
patient's condition.
The physician diagnoses Ms. Williams as having acute hepatitis B. The diagnosis isn't a surprise; sexual partners of I.V. drug users are at risk for hepatitis B
and C. Hepatitis B can be transmitted via blood or during sex, although condoms will help prevent the transmission.
Like all patients with high risk factors for hepatitis B, Ms. Williams should be screened for HIV. Because HIV can be transmitted the same way as hepatitis B,
many patients with one disease also have the other.
After her case has been reported, the public-health department will notify anyone who's had contact with Ms. Williams-through sexual relations or needle
sharing, for example. These people will be offered the hepatitis B vaccine and hepatitis B immune globulin (HBIG).
As for her children, Ms. Williams should be encouraged to follow up with her pediatrician or go to her health department for HBIG and hepatitis B vaccine.
Hepatitis B vaccine is recommended for all newborns and required for school entry in some states.
Explaining the diagnosis You need to make sure Ms. Williams understands her diagnosis. She'll need to learn safer sex practices, such as consistent use of a
condom. If she still has a positive HBsAg test in 6 months, she'll most likely be a carrier, capable of transmitting the infection through shared needles, sexual
relations, or blood transfusions.
If she becomes a carrier, she'll be susceptible to future hepatitis B flare-ups. (Not all carriers have flareups, though.) She'll also have an increased risk of
cirrhosis and liver failure. Carriers may be asymptomatic or have ongoing signs and symptoms of infection (referred to as chronic carriers). All carriers are
capable of transmitting the disease.
Chronic carriers can be treated with recombinant interferon alfa-2b injections. This therapy is administered over a 16-week period. Up to 40% of patients who
receive this therapy go into remission; up to 10% are eventually cured.
A full recovery from hepatitis B is documented with a negative HBsAg test and a positive anti-HBs testas well as normal ALT levels. The presence of anti-HBs
indicates immunity to hepatitis B (which means that the patient is also immune to hepatitis D, the coinfection of hepatitis B).
For now, though, Ms. Williams should concentrate on not spreading the disease. You advise her to make sure any sexual partner uses a condom. Because her
sexual partner is the likely source of Ms. Williams's hepatitis B, the health department will follow up with him and suggest screening him for HIV.
Now that you've explained everything to Ms. Williams and answered her questions, you schedule her for an interview with a caseworker from your hospital's
social services department. You want to make sure she'll receive proper follow-up. Two days after her admission, she's discharged.
Responding to hepatitis C
Dr. John Walsh, 60, is admitted with jaundice, nausea, and vomiting. You learn that he received several units of blood during coronary bypass surgery 6
months ago. His preliminary diagnosis is hepatitis, but the lab tests for hepatitis A and B are negative. Like Ms. Williams, Dr. Walsh has elevated liver enzymes.
His hepatitis C antibodies are positive.
While admitting him, you learn that he's never traveled outside the United States. His physician rules out Epstein-Barr virus and cytomegalovirus.
His physician suspects that Dr. Walsh was infected with hepatitis during one of his transfusions, so most likely, he has hepatitis C. Despite current bloodscreening methods, no lab test is absolute.
A more sensitive lab test for the hepatitis C antibody (anti-HCV) confirms the diagnosis. An interval of 2 to 6 months passes between exposure to hepatitis C
and the development of the antibody in the blood.
No specific therapy is available for hepatitis C, so treatment is supportive. Like the previous two patients, Dr. Walsh needs to be prepared properly for
discharge.
We know hepatitis C can be spread through blood; whether it's transmitted in other ways is controversial. Because sexual transmission may be possible, some
experts recommend barrier protection during sexual intercourse. Before advising Dr. Walsh, you'd talk with his physician or an infectious-disease expert about
discharge instructions.
Make sure that Dr. Walsh is aware that he could develop chronic hepatitis (with ongoing signs and symptoms) or cirrhosis. Recombinant interferon alfa-2b
injections, the same therapy used with chronic hepatitis B carriers, can also be given to hepatitis C carriers. Administered in low doses for 6 months, the
therapy has been shown to improve hepatic function in about half of the chronic hepatitis C carriers who receive it.
For now, though, Dr. Walsh isn't a candidate for this therapy. Three days after admission, his symptoms are brought under control and he's discharged.
Special considerations for hepatitis D and E
Hepatitis D occurs only when the patient already has hepatitis B, either during the acute phase or as a chronic carrier. It's endemic in Italy, the Middle East,
Africa, and South America. When it strikes, the patient will experience acute hepatitis symptoms. Hepatitis D typically leads to death.
The only widely used test for this disease is for the antibody (antiHDV), which indicates past exposure to the virus. As with other forms of hepatitis, treatment
is supportive. Recombinant interferon alfa-2b injections have been successful in forcing the virus into remission, with relapses occurring after therapy ends.
Studies continue with other drugs.
Hepatitis E resembles hepatitis A in that it's transmitted enterically and doesn't result in chronic hepatitis. It has been associated with epidemics in developing
countries. It usually isn't fatal. Not yet a reportable disease, it's diagnosed by ruling out all other forms of viral hepatitis.
As for hepatitis G, to date, the virus has been isolated in the lab only. Infection is usually benign.
Patient teaching: Crucial to recovery
No matter what type of hepatitis your patient has, effective patient teaching is crucial to his recovery. Before he's discharged, you should:
assess his understanding of the disease and the recovery process (see Comparing Different Types of Viral Hepatitis for vital patient-teaching information)
tell him to rest between periods of activity; his energy level won't return to normal for up to 6 months explain the potential effects of nonprescription drugs on
his liver; tell him to check with his physician before taking any drug
instruct him to drink more fluids and eat foods with fiber to encourage normal bowel function
make sure he knows that he can never donate blood again because of the risk that he'd spread his disease emphasize the importance of keeping his physician
and lab appointments for follow-up care tell him to avoid drinking alcoholic beverages for 6 to 12 months, or longer if indicated make sure that he understands
that immunity to one type of hepatitis doesn't guarantee immunity to other types
explain, if possible, how long he'll be infectious. With hepatitis A, the infectious period usually ends a week after symptoms subside. (The local health
department will make a specific recommendation.) With hepatitis B, the patient can transmit infection for as long as tests show he has the antigen in his blood
(usually 20 weeks for patients who don't become chronic carriers). The infectious period for hepatitis C is the same as for B; the periods for D, E, and G aren't
known.
Highest level of care
Once you've covered all these points with your patient, you'll know you've given him the information he needs to manage his recovery. And if you've followed
the other precautions we've discussed-including infection control techniques-you'll have done everything possible to prevent hepatitis from spreading. I
SELECTED REFERENCES
DiBisceglie, A.: "Hepatitis G Virus Infection: A Work in Progress," Annals of Internal Medicine. 125(9): 772-773, November 1996.
Niederau, C., et al.: "Long-Term Follow-up of HBeAg-Positive Patients Treated with Interferon Alfa for Chronic Hepatitis B," The New England Journal of
Medicine. 334(22):1422-1427, May 30, 1996.
Tong M., et al.: "Clinical Outcomes after TransfusionAssociated Hepatitis C," The New England Journal of Medicine. 332(22):1463-1466, June 1, 1995.
SELECTED WEB SITES
American Liver Foundation
sadieo.ucsf.edu/alf/alffinal/ homepagealf.html
CDC Hepatitis Branch
www.cdc.gov/ncidod/diseases/ hepatitis/hepatitis.htm
Hepatitis B Foundation
www2.hepb.org/hepb/home.html
HepNet, the Hepatitis Information Network
www.hepnet.com/index.html
BY JAMES F. MARX, RN, CIC, MS
Infection Control and Epidemiology Consultant
Broad Street Solutions
San Diego, Calif.
Copyright Springhouse Corporation Jul 1998
Provided by ProQuest Information and Learning Company. All rights Reserved