Joshua_Simon_WISER_WITH_AGE_INCREASED_PER
advertisement

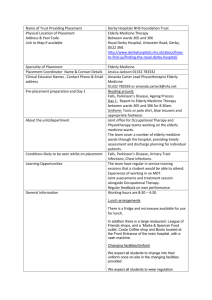
WISER WITH AGE?: INCREASED PER-SURGEON ELDERLY PATIENT VOLUME IS ASSOCIATED WITH LOWER POST-INJURY COMPLICATIONS Joshua Simon DO1,2, Quoc Dang DO1,2, Joe Catino MD2,3, Ivan Puente MD2,3, Fahim Habib MD2,3, Marko Bukur MD2,3 1Larkin Community Hospital, South Miami, FL; 2Delray Medical Center, Delray Beach, FL; 3Broward General Medical Center, Fort Lauderdale, FL OBJECTIVES The elderly population is the fastest growing age group in the United States and traumatic injury continues to be a significant cause of death and disability. Previous studies in trauma patients have suggested improved outcomes with increased per-surgeon volumes in severely injured patients. This effect has not been examined in the elderly trauma population. We hypothesized that increased per-surgeon elderly trauma volume would impact outcomes. METHODS This was a five year registry review of elderly patients admitted to a State Level I trauma center. All fellowship trained trauma surgeons were stratified into Low (LV), Average (AV), and High (HV) Volume Groups according to average elderly patient admission per year. Patients were excluded if they were under 55 years of age, arrived dead on arrival, had non-survivable injuries, or LOS of less than 48 hours. The primary outcomes were in-hospital mortality and post-traumatic complication rate. Stepwise forward logistic regression was used to analyze the effect of surgeon volume on outcomes. RESULTS During the five year study period a total of 2,379 elderly patients were evaluated. Mean admission volume per year was 9.8 ± 5.5, 28.8 ± 6.8, and 62.4 ± 9.1 in the LV, AV and HV Groups, respectively (p<0.001). The median number of years in practice was 17 (IQR 9,21) and not significantly different between the groups, (p=0.883). Patients in the HV group were older (Mean Age HV 77.7 vs AV 73.9 vs LV 73.9, p<0.001), had higher Charlson Scores (4 vs 3 vs 3, p<0.001), more severe head injuries (Head AIS≥3, 49.1% vs 38.1% vs 35%, p<0.001) and higher injury severity (ISS>16, 38.9% vs 30.6% vs 28%, p<0.001) than those admitted by the AV and LV. Need for operative intervention was similar between the 3 groups (8.1% vs 11% vs 7.4%, p=0.091). Overall complications were significantly higher in patients admitted by the LV and AV Groups (21% vs 18.1% vs 15%, p<0.027). Forward logistic regression identified HV to be associated with a lower overall complication rate (HV vs LV AOR 0.57, 95%CI [0.40,0.81], p=0.002, HV vs AV AOR 0.74, [0.57,0.97], p<0.032). Inhospital mortality was not significant between groups (HV 2.9% vs AV 4% vs LV 4.1%, p=0.371). CONCLUSION Our results suggest that overall morbidity of the elderly trauma patient may be impacted by surgeon volume. Further studies identifying the optimal level of surgeon experience should be undertaken. Joshua Simon, DO 2711 Ocean Club Blvd. Apt. 307 Hollywood, FL 33019 Tel: 352.215.3989 E-mail: simon.josh@gmail.com Joshua Simon, DO 2711 Ocean Club Blvd. Apt. 307 Hollywood, FL 33019 Tel: 352.215.3989 E-mail: simon.josh@gmail.com