Respiratory health
advertisement

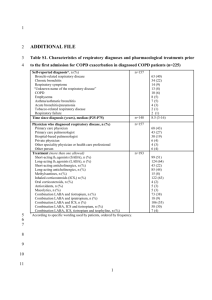
5.10 Respiratory health Respiratory health was assessed at both baseline and follow up. There were some differences between the two studies, however, in regard to the scope of respiratory health data collected and the mode of data collection, which limited our ability to assess change over time on those variables. At follow up a brief list of respiratory symptoms and medical conditions were assessed via self-report questionnaire. The questions included at follow up were pared down or modified from a larger set of respiratory symptom and condition questions administered by a nurse in the baseline study. The baseline study also included lung function testing using a spirometer, which was not included at follow up. The follow up study included an assessment of respiratory health medications dispensed to participants under the PBS or RPBS, which was not included at baseline. 5.10.1 Respiratory symptoms and conditions at follow up The respiratory symptoms and conditions assessed at follow up are shown in Table 1. Gulf War veterans were statistically significantly more likely than the comparison group to report all measured symptoms of wheeze, cough and sputum. The difference between groups was the greatest in magnitude for morning cough, with Gulf War veterans 67% more likely than the comparison group to report this symptom. Whilst statistical significance was not achieved for the differences between groups on the respiratory conditions shown in Table 1, such as measures of doctor diagnosed asthma, chronic bronchitis and emphysema or Chronic Obstructive Pulmonary Disease (COPD), the pattern was such that all point estimates were higher in the Gulf War veteran group. The greatest difference was for COPD, but numbers were very small. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 123 Table 1 Self-reported respiratory symptoms and medical conditions at follow up Gulf War veterans (N=659) Comparison group (N=697) n (%) n (%) RR Adj RR* (95% CI) 182 (26.73) 106 (16.43) 1.63 1.44 (1.15-1.80) Wheeze with breathlessness 96 (55.17) 43 (43.43) 1.27 1.34 (1.02-1.75) Wheeze present but not a cold 134 (77.91) 65 (64.36) 1.21 1.23 (1.03-1.47) Woken by nocturnal cough in last 12 months 201 (29.26) 133 (20.46) 1.43 1.37 (1.11-1.69) Morning cough 127 (18.35) 71 (10.99) 1.67 1.67 (1.26-2.23) Day or night time cough 166 (24.16) 108 (16.64) 1.45 1.36 (1.09-1.70) Symptom-based definition of Chronic bronchitis§ 144 (20.78) 84 (12.90) 1.61 1.51 (1.17-1.96) Morning sputum in Winter 156 (23.01) 99 (15.57) 1.48 1.38 (1.10-1.74) Day or night time sputum in Winter 160 (23.85) 110 (17.32) 1.38 1.31 (1.06-1.63) Sputum most days for 3 months in two successive years 105 (66.04) 52 (47.71) 1.38 1.31 (1.04-1.65) Self-reported asthma 100 (14.41) 80 (12.18) 1.18 1.13 (0.86-1.50) Self-reported doctor confirmed asthma 87 (12.57) 73 (11.18) 1.12 1.09 (0.81-1.47) Asthma attack in last 12 months 33 (33.33) 16 (20.78) 1.60 1.56 (0.89-3.74) Currently taking asthma medication† 42 (42.42) 23 (30.26) 1.40 1.42 (0.91-2.21) Self-reported doctor confirmed Chronic bronchitis 75 (10.84) 69 (10.57) 1.03 1.03 (0.74-1.43) Self-reported doctor confirmed emphysema or COPD‡ 8 (1.15) 4 (0.61) 1.89 2.14 (0.60-7.66) Respiratory symptoms and medical conditions Wheeze in last 12 months * Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks), each estimated as at August 1990, any atopy at baseline and current smoking status (never; former; current smoker) † 5 participants who reported taking asthma medication did not specify which ones they took. ‡ COPD is Chronic Obstructive Pulmonary Disease § Defined as morning, day or night time cough for as much as three months in each of the previous two years Prescribed respiratory health medications recorded on the PBS and RPBS Where participants had provided consent, linked PBS and RPBS data was evaluated to determine the prevalence of participants who had been dispensed a medication for obstructive lung disease, including asthma and COPD, since the baseline study and in the past 12 months. In adults, the majority of inhaled corticosteroids are prescribed in combination with long-acting B-agonists, e.g. Fluticasone/Salmeterol (Seretide) or Budesonide/Eformoterol (Symbicort), and administered through inhalers, or puffers. In the PBS and RPBS it was not possible to distinguish between medications dispensed for asthma from those for other obstructive lung diseases, such as COPD.44 However, for these combination inhalers the dispensed price is greater than or equal to the co-payment for those without a concession card, therefore all prescriptions, regardless of concession card possession, are captured in the database44 and were used to compare use of medications for obstructive airways disease including asthma and COPD in the two study groups. Medications such as Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 124 short-acting beta-agonists, e.g. Ventolin inhalers and about half of the inhaled corticosteroids, cost less than the PBS copayment amount for general patients and do not appear on the PBS or are only subsidised by the PBS when the patient is a concession cardholder. Therefore these medications were not compared. Tiotropium bromide (Spiriva) is a long acting inhaled anticholinergic approved only for use in treatment of COPD and this was also used to compare use of medication for COPD44 in the two study groups. The PBS and/or RPBS data showed that 44 Gulf War veterans (8.2%) and 32 comparison group members (6.5%) had been dispensed a medication listed under the ATC code R03AK for “Adrenergics and other drugs for obstructive airway diseases” or Tiotropium (ATC code R03BB) in the period since the baseline study. In the 12 month period prior to the follow up study only 3.5% of Gulf War veterans and 2.4% of the comparison group had been dispensed one of these medications and this difference between the groups was not significant (RR 1.45, adj RR 1.19, 95% CI 0.59-2.41). 5.10.2 Key findings Respiratory symptoms in relation to wheeze, cough and sputum were all reported significantly more frequently by Gulf War veterans than the comparison group. Self-reported doctor-confirmed respiratory medical conditions including asthma, chronic bronchitis and emphysema or COPD were also reported more frequently by Gulf War veterans, but these differences between groups were not statistically significant. There was no significant difference between the two groups in regard to respiratory medication use in the 12 months prior to follow up, as measured using PBS and RPBS data. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 125