Local Anesthesia (2)
advertisement

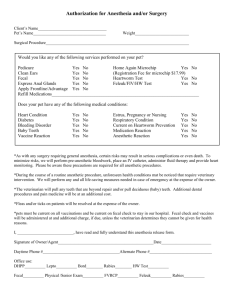
1 Florida Heart CPR* Local Anesthesia 2 hours INTRODUCTION Local anesthesia with sedation offers anesthesia personnel and the surgeon great flexibility in tailoring the degree of anesthesia to the needs of the patient. Procedures that once required patients to stay overnight in the hospital now are performed safely in office and outpatient surgical suites. The introduction of new anesthetic applications enables patients to undergo lengthy and complex procedures as outpatients and then promptly and safely be discharged home. The choice and route of anesthesia administration is paramount to the patient's overall surgical experience. If the patient upon discharge is alert, has minimal pain, and has no nausea or vomiting, then their surgical experience is a positive one (Stoelting, 1989). PREOPERATIVE SELECTION The 3 modalities of administering anesthetic agents include local anesthesia, monitored anesthesia care (MAC), and general anesthesia via an endotracheal tube or laryngeal mask. Appropriate patient selection begins with a meticulous medical and surgical history and physical examination. Once the patient has been cleared for anesthesia, the surgeon must determine if the proposed surgery can be performed effectively under MAC or if general anesthesia is necessary. Another critical factor contributing to the choice of anesthetic modalities to be employed is the patient's attitude and affect. Some patients want to be "asleep" for the duration of the surgery, fearing any pain or the chance of hearing what actually is being performed during surgery. Other patients have trepidation toward general anesthesia and "having a tube stuck down the throat." If the intravenous (IV) sedation is not going to be deep and the patient is particularly anxious and not cooperative, this combination may prove meddlesome during prolonged surgical procedures. The patient may become restless, requiring more anesthetic agents for a deeper level of sedation than planned. A resultant decrease in respiratory drive and possible compromise of patient safety may occur during the procedure. MONITORED ANESTHESIA CARE MAC combines IV sedation with local anesthetic infiltration or nerve blocks. Procedures such as otoplasty, facelift, blepharoplasty, or liposuction are examples of surgeries routinely performed under MAC. Patients given monitored anesthesia rather than general anesthesia experience fewer incidences of nausea and vomiting and typically can be discharged home safely and quickly. The primary disadvantage of MAC Florida Heart CPR* Local Anesthesia 2 is the lack of airway control and the threat of aspiration or obstruction. To minimize these risks, the anesthesia personnel must titrate the medications carefully to maintain spontaneous respirations while maintaining an anesthetic depth, allowing the patient to remain comfortable. Careful selection and administration of medications is essential in producing the desired and optimal intraoperative anesthetic effect and postoperative outcomes. LOCAL ANESTHESIA Local anesthesia encompasses infiltration of the operative site, tumescent techniques, and nerve blocks. A nerve block can be labeled minor if one nerve is affected or major if more than one nerve or conduction in a nerve plexus is impeded. Local anesthetic agents are usually of the amino amides class and include such agents as lidocaine, bupivacaine, prilocaine, mepivacaine, and etidocaine. The potency, onset of action, and duration of these agents varies. Depending on the area to be anesthetized, varying techniques can be implemented. For incisional sites, a local anesthetic such as 1% lidocaine with EPI is ideal for direct injection into the incisional site with rapid onset of the anesthetic effect. For procedures in which flaps are to be elevated, as in a facelift or coronal forehead lift, the incision site is anesthetized as previously mentioned, and the flap area can be infiltrated with a diluted anesthetic such as 0.5% lidocaine with EPI. For the local anesthetic, 1% lidocaine often is used with 1:200,000 or 1:100,000 EPI. The latter prolongs the anesthetic effect of lidocaine as a result of its vasoconstrictive properties. If more prolonged anesthesia is desired, lidocaine can be mixed with bupivacaine, providing the rapid but shorter lasting anesthesia effect of the former coupled with the slower but prolonged anesthetic effect of the latter. In tumescent techniques, vastly larger amounts of anesthetic are used, albeit in dilute concentrations. Adipose tissue is suffused via an infusion cannula in the subcutaneous space, with large volumes of diluted lidocaine (0.05-0.1%) and a diluted concentration of EPI (1:1,000,000) for both anesthetic and hemostatic effects. The safety of this technique lies in the fact that the anesthetic concentration is extremely small, allowing large amounts of solution to be used without reaching toxic levels. For example a mixture of 500 mL of normal saline with 50 mL of 2% lidocaine will result in a concentration of lidocaine of less than 0.2%. In addition, a tissue plane is created that aids in later dissection. Complications Complications of local anesthetic agents can manifest as a localized reaction or systemic adverse effects. The most common cause of such sequelae is secondary to Florida Heart CPR* Local Anesthesia 3 accidental intravascular infiltration but systemic conditions also may increase the risk of these untoward effects. Cardiovascular disease, hepatic and renal dysfunction, acidbase abnormalities, and hypoxia can amplify the possibility of anesthetic toxicity. In addition, the very old, very young, and gravid females may respond aberrantly to these agents. Localized untoward effects include prolonged or permanent paresthesias, anesthesia, and motor weakness. In addition, local vasoconstriction has been reported with resultant necrosis. Systemic adverse effects can result in angina pectoris, shortness of breath, dysrhythmias, and cardiovascular collapse. Bupivacaine in particular has been associated with decreased cardiac output and hypotension. Disorientation, auditory and visual hallucinations, and decreased responsiveness, including coma, are possible effects of CNS toxicity. Respiratory and cardiovascular collapse and seizures also may emanate from CNS-induced toxicity. Rash and other manifestations of allergic reactions (including anaphylaxis) can result from local anesthetic agents. The amino amides are much less likely to cause immune reactions because of their lack of para-aminobenzoic acid (PABA), as compared to the amino esters, which are derivatives of PABA. Some amino amides do contain methylparaben, a structural similar compound to PABA, which may account for the resultant stimulatory immune effect of the amino amides. Methemoglobinemia can result in respiratory drive irregularity, cyanosis, and graying of the skin. Prilocaine mainly has been linked to this toxic effect as a result of its metabolite acting as an oxidizing agent of hemoglobin. Remain cognizant of the possibility of local anesthetic reaction to successfully manage these untoward effects. If suspected, the injection should be terminated, the patient’s airway should be assessed for patency, and supplemental oxygen should be administered. Vital signs and pulse oximetry should be checked. If the patient is desaturating, an airway should be secured through basic life support protocols. If this proves unsuccessful, intubation and advanced cardiac life support protocols are indicated. If hypotension or dysrhythmias occur, IV fluids, vasopressors, and antiarrhythmic drugs should be employed. Management of CNS toxicity is directed toward control of respiratory drive and halting seizure activity. Benzodiazepines and succinylcholine are the drugs of choice to abort seizure activity and decrease neuromuscular sequelae to facilitate airway control, respectively. MONITORED ANESTHESIA CARE - TECHNIQUE Florida Heart CPR* Local Anesthesia 4 IV sedation may begin after IV access is secured, cardiopulmonary monitors are applied, and oxygen is given via nasal cannulae. Midazolam (Versed), a short acting, water-soluble benzodiazepine, is administered in 1mg bolus doses for its amnestic and anxiolytic properties. Midazolam, with a 2-hour half-life, has limited cardiovascular effects, allows for expeditious recovery, and has no postoperative sequelae such as nausea and vomiting. Fentanyl, a rapidly acting narcotic analgesic, can be administered in boluses of 25- to 50-mcg increments for analgesia with little sedative effect. As with all narcotic agents, respiratory function can be depressed, and the patient may experience nausea and emesis. A 10- to 20-mg bolus of ketamine, which produces dissociated anesthesia, can facilitate tolerance to injection of local anesthetic agents. Serious cardiovascular adverse effects and seizures have been reported along with psychotic reactions and nightmares. Propofol (Diprivan) is a rapidly acting sedative and hypnotic agent. Propofol has excellent effects with quick patient recovery. Given in 0.5-1 mg/kg injections that are infused slowly prior to the injection of local anesthesia, propofol maintains respiratory drive and allows the patient to tolerate the local anesthetic injections. A propofol infusion, with a starting dose of as low as 25 mcg/kg/min throughout the procedure, can provide smooth and constant anesthesia with the option of "deepening" the patient at stimulating moments by administering boluses of 50 mcg of fentanyl, 10 mg of ketamine, or 10 mg/kg of propofol. Near the end of surgery, the propofol infusion must be titrated to “lighten” the patient and must be turned off approximately 5 minutes prior to the end of the procedure. At this time, the patient should be awake and following commands appropriately. Upon transfer to the recovery room, IV fentanyl (25-50 mcg) or Demerol (12.5-25 mg) may be given for postoperative pain or shivering. Postoperatively, patients who have undergone MAC must be monitored for cardiorespiratory function, bleeding, nausea, and pain. The rapidity of patient recuperation depends on the length and type of procedure and on the type of sedation employed. Another factor may be the overall patient tolerance to anesthetic agents and the ability to metabolize these chemicals for excretion from the body. Concomitant use of other pharmaceutical agents and body habitus can affect the rate of anesthetic metabolism and overall tolerance to these agents. For example, a patient who weighs 80 kg should receive a maximum dose of 550 mg of lidocaine with epinephrine. If using 2% lidocaine, then the patient should not receive more than 225 mL of this agent. The maximum doses of all anesthetic agents should be committed to memory, allowing for the calculations as shown above. In addition, medications such as the aminoglycosides, succinylcholine, and compounds that reduce liver functions may increase the toxicity of local anesthetic agents. Florida Heart CPR* Local Anesthesia 5 The patient should be questioned concerning problems with anesthesia in the past. Using local anesthetics sparingly or avoiding certain compounds helps the clinician to avoid toxic adverse effects. ALTERNATIVES Although MAC is a safe method for providing anesthesia, general anesthesia is preferred for lengthy or complex procedures. General anesthesia provides amnesia, analgesia, and muscle relaxation. In addition, the patient’s airway is secured with an endotracheal tube or laryngeal mask, and the risk of aspiration or obstruction is minimized. The primary disadvantage of general anesthesia is the increased incidence of nausea and vomiting and the somnolence of patients postoperatively. However, in properly selected patients, local anesthesia with MAC is a safe and effective method of providing anesthesia for operative procedures. REFERENCES Badrinath S, Avramov MN, Shadrick M, et al: The use of a ketamine-propofol combination during monitored anesthesia care. Anesth Analg 2000 Apr; 90(4): 858-62. Biswas S, Bhatnagar M, Rhatigan M, et al: Low-dose midazolam infusion for oculoplastic surgery under local anesthesia. Eye 1999 Aug; 13 ( Pt 4): 537-40. Hogan Q: Local anesthetic toxicity: an update. Reg Anesth 1996 Nov-Dec; 21(6 Suppl): 43-50. Katzen LB: Anesthesia, anelgesia, and amnesia. In: Cosmetic Oculoplastic Surgery, Eyelid, Forehead, and Facial Techniques. 3rd ed. 1999: 67-74. Kendell J, Wildsmith JA, Gray IG: Costing anaesthetic practice. An economic comparison of regional and general anaesthesia for varicose vein and inguinal hernia surgery. Anaesthesia 2000 Nov; 55(11): 1106-13. Nique TA: Introduction: The anesthetic continuum. In: Anesthesia for Facial Plastic Surgery. 1993: 1-3. Stoelting R, Miller R: Basic Anesthesia. 2nd ed. 1989: 417. Thorne AC: Local anesthetics. In: Ashton SM, Beasley RW, Thorne CHM, eds. Grabb and Smith's Plastic Surgery. 5th ed. 1997. Florida Heart CPR* Local Anesthesia 6 Florida Heart CPR* Local Anesthesia Assessment 1. The modalities of administering anesthetic agents include: a. local anesthesia b. monitored anesthesia care (MAC) c. general anesthesia via an endotracheal tube or laryngeal mask d. all of the above 2. This combines IV sedation with local anesthetic infiltration or nerve blocks. a. Local anesthesia b. MAC c. General anesthesia d. All of the above 3. Patients given ______ rather than _______experience fewer incidences of nausea and vomiting and typically can be discharged home safely and quickly. a. Monitored anesthesia / general anesthesia b. General anesthesia / monitored anesthesia c. General anesthesia / MAC d. MAC / general anesthesia 4. Complications of local anesthetic agents can manifest as a localized reaction or systemic adverse effects. a. A localized reaction b. Systemic adverse effects c. Both A and B d. Neither A nor B 5. Systemic adverse effects from complications of local anesthetic agents can result in: a. cardiovascular collapse. b. angina pectoris c. shortness of breath d. all of the above 6. Postoperatively, patients who have undergone MAC must be monitored for pain and: a. Cardiorespiratory function b. Bleeding c. Nausea d. All of the above 7. Although MAC is a safe method for providing anesthesia, general anesthesia is preferred for: Florida Heart CPR* Local Anesthesia 7 a. Lengthy procedures b. Emergency procedures c. Complex procedures d. A and C 8. General anesthesia provides: a. Amnesia b. Analgesia c. Muscle relaxation d. All of the above 9. The primary disadvantage of ______ is the increased incidence of nausea and vomiting and the somnolence of patients postoperatively. a. MAC b. Local anesthesia c. General anesthesia d. All of the above 10. The primary disadvantage of ____ is the lack of airway control and the threat of aspiration or obstruction. a. MAC b. Local anesthesia c. General anesthesia d. All of the above Florida Heart CPR* Local Anesthesia