Paramedic Law & Ethics: Chapter Review
advertisement
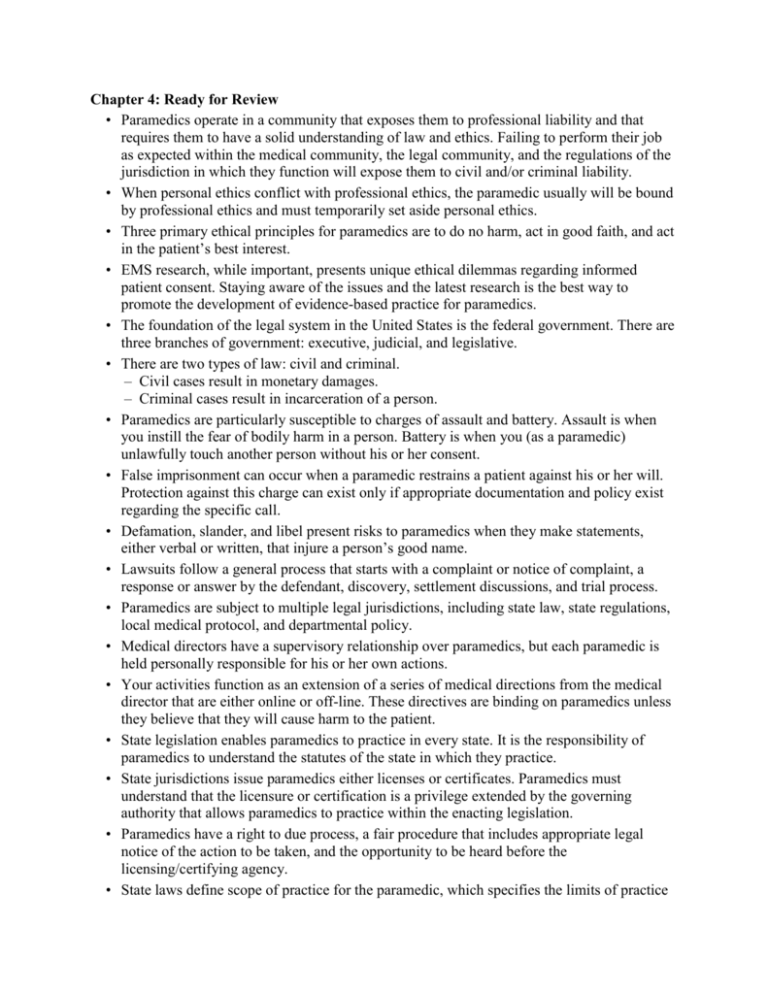
Chapter 4: Ready for Review • Paramedics operate in a community that exposes them to professional liability and that requires them to have a solid understanding of law and ethics. Failing to perform their job as expected within the medical community, the legal community, and the regulations of the jurisdiction in which they function will expose them to civil and/or criminal liability. • When personal ethics conflict with professional ethics, the paramedic usually will be bound by professional ethics and must temporarily set aside personal ethics. • Three primary ethical principles for paramedics are to do no harm, act in good faith, and act in the patient’s best interest. • EMS research, while important, presents unique ethical dilemmas regarding informed patient consent. Staying aware of the issues and the latest research is the best way to promote the development of evidence-based practice for paramedics. • The foundation of the legal system in the United States is the federal government. There are three branches of government: executive, judicial, and legislative. • There are two types of law: civil and criminal. – Civil cases result in monetary damages. – Criminal cases result in incarceration of a person. • Paramedics are particularly susceptible to charges of assault and battery. Assault is when you instill the fear of bodily harm in a person. Battery is when you (as a paramedic) unlawfully touch another person without his or her consent. • False imprisonment can occur when a paramedic restrains a patient against his or her will. Protection against this charge can exist only if appropriate documentation and policy exist regarding the specific call. • Defamation, slander, and libel present risks to paramedics when they make statements, either verbal or written, that injure a person’s good name. • Lawsuits follow a general process that starts with a complaint or notice of complaint, a response or answer by the defendant, discovery, settlement discussions, and trial process. • Paramedics are subject to multiple legal jurisdictions, including state law, state regulations, local medical protocol, and departmental policy. • Medical directors have a supervisory relationship over paramedics, but each paramedic is held personally responsible for his or her own actions. • Your activities function as an extension of a series of medical directions from the medical director that are either online or off-line. These directives are binding on paramedics unless they believe that they will cause harm to the patient. • State legislation enables paramedics to practice in every state. It is the responsibility of paramedics to understand the statutes of the state in which they practice. • State jurisdictions issue paramedics either licenses or certificates. Paramedics must understand that the licensure or certification is a privilege extended by the governing authority that allows paramedics to practice within the enacting legislation. • Paramedics have a right to due process, a fair procedure that includes appropriate legal notice of the action to be taken, and the opportunity to be heard before the licensing/certifying agency. • State laws define scope of practice for the paramedic, which specifies the limits of practice • • • • • • • • • • • • • • • • allowed under the Medical Practice Act. HIPAA was enacted to protect patient information from unlawful and unnecessary dissemination. EMTALA is another federal law designed to prevent hospital emergency departments from turning patients away for any reason, including the ability to pay for care. Emergency vehicle operations must be performed in a manner that protects the public from further injury. No call can justify driving in a manner that endangers the public. Transportation to a certain medical facility should be determined by taking into account the patient’s preference and the medical needs of the patient. Crime scenes present the intersection between EMS and law enforcement. Paramedics have an obligation to assist the law enforcement community in preservation of evidence and documentation of scenes or actions that may later be introduced on behalf of a criminal prosecution. Paramedics can be held legally responsible when they fail to report cases such as suspected abuse, domestic violence, gunshot/stab wounds, childbirth outside a medical facility, rape, infectious diseases, or animal bites. Suspected homicides, suicides, prison inmate deaths, and other violent or unexpected deaths should immediately be reported to local law enforcement personnel in order to allow a coroner or medical examiner to examine the body. All patients of sound mind have the legal right under the US Constitution to privacy, consent, and refusal. Paramedics cannot infringe on these inalienable rights unless they believe that patients are not of sound mind and pose a detriment to themselves or others. Patient refusals pose a large potential legal liability to paramedics. The only protection against a civil suit over a refusal will be the documentation at the time of the incident. – A refusal signature without narrative and evidence of a physical assessment is worthless. You must obtain informed consent from patients prior to any medical process, including examination. You must get expressed consent—action demonstrating permission to provide care—from patients before initiating treatment. Implied consent is said to exist when patients are unable to answer for themselves and paramedics deem that treatment is required. Determining the decision-making capacity of a patient can be tricky, but tools such as pulse oximetry and blood glucose measurements can provide factual documentation of patient awareness and ability to make clear decisions regarding his or her medical care. In any questionable circumstance, thorough documentation and consultation with medical control will provide the best protection against lawsuits. Minors pose challenges that local jurisdictions must address before a call occurs. In general, if the patient is a minor, the minor has neither the right to consent to care nor the right to refuse it, although exceptions for emancipated minors exist. Violent patients may be restrained using physical or chemical means if they are a danger to themselves or others. Always follow local medical and law enforcement protocols when addressing the needs of violent or potentially violent patients. Allocation of resources and triage challenges can present serious ethical dilemmas to • • • • • • • • • • • • paramedics. In such circumstances, well-established protocols and professional ethics should take precedence over any personal feelings or ethics of the paramedic. Negligence occurs only when the following four processes have occurred: – Duty to act. The paramedic must have had a duty to act. – Breach of duty. The paramedic did not fulfill that duty. – Proximate cause. The paramedic’s breach of duty caused the plaintiff’s injury. – Injury resulted. An injury occurred as a result of the above. Negligence can be categorized as acts of commission (malfeasance and misfeasance) or acts of omission (nonfeasance). As the highest level of prehospital care providers, paramedics must ensure that they do not abandon their patients. Abandonment can occur anytime paramedics turn over their patients inappropriately or to a level of care lesser than themselves. Documentation is the only methodology to prevent the appearance of abandonment. Patients have the right to determine their own care. Paramedics must understand their legal limitations based on any advance directives issued by the patient. Do not resuscitate (DNR) orders are a specific form of advance directive that generally define the care a patient wants when lifesaving procedures are required. A DNR order is not a “do-not-care-for-the-patient” order. Patients often decide on medical care and treatment issues prior to an emergency. Paramedics need to be familiar with DNR orders, living wills, health care powers of attorney, surrogate decisions, and organ donations. Futile resuscitation efforts, which you may encounter, need to be addressed and considered prior to an emergency event. Weighing various ethical issues prior to their occurrence can help prevent and reduce suffering in your patient population. You may provide care when off duty and in most jurisdictions be protected under the Good Samaritan laws. Paramedics must remember that they are only protected if they perform within their training and education and if they do not receive any compensation. You can be protected under certain governmental immunity clauses. These protections may not be valid if the paramedics have committed negligence or if the paramedics are deemed to be personally liable. Two common legal defenses are the statute of limitations (time in which to file a lawsuit) and contributory negligence, when a plaintiff has contributed to the negative outcome by committing an act or failing to disclose relevant information to medical practitioners. Several federal and state laws affect the relationship between the paramedic and his or her employer. These laws promote a healthier, safer workplace by addressing topics such as discrimination, sexual harassment, family leave, and occupational safety regulations.