Student Care Policy & Procedures Rationale: The policy outlines the
advertisement

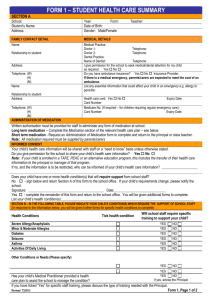
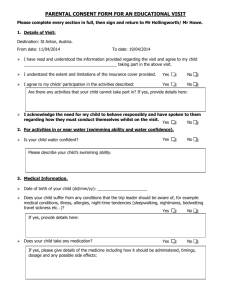
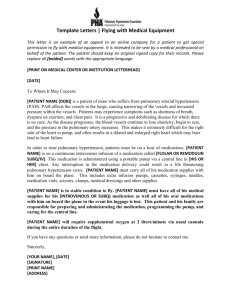
Student Care Policy & Procedures Rationale: The policy outlines the college’s responsibility and procedures in respect of our “responsibility to provide equitable access to education and respond to diverse student needs, including health care needs”. Confidential records of all students with specific health needs are maintained securely in the general office for reference as required. A First Aid Register is also maintained noting ailments and treatment for all presenting students. Section 1: First Aid Policy & Procedures Aim: Administer first aid to children when in need in a competent and timely manner. Communicate children’s health problems to parents when considered necessary. Provide supplies and facilities to cater for the administering of first aid. Maintain a sufficient number of staff members trained with a level 2 first aid certificate. Identify staff as first aid officers, including their level of training and training expiry date Implementation: A sufficient number of staff (including at least 1 administration staff member) to be trained to a level 2 first aid certificate, and with up-to-date CPR qualifications. A Health Centre will be available for use at all times. A comprehensive supply of basic first aid materials will be stored in a locked cupboard in the Health Centre. Supervision of the Health Centre will be provided by an Assistant Principle in the absence of the school nurse. Any children in the Health Centre will be supervised by a staff member at all times. A confidential up-to-date register (secured) located in the Health Centre room will be kept of all injuries or illnesses experienced by children that require first aid. All staff will be provided with basic first aid management skills, including blood spills, and a supply of protective disposable gloves will be available for use by staff. Minor injuries only will be treated by the nominated staff member, while more serious injuries-including those requiring parents to be notified or suspected treatment by a doctor - require a level 2 first aid trained staff member to provide first aid. Any children with injuries involving blood must have the wound covered at all times. No medication including headache tablets will be administered to children without the express written permission of parents or guardians. Parents of all children who receive first aid will receive a completed form indicating the nature of the injury, any treatment given, and the name of the person providing the first aid. For more serious injuries/illnesses, the parents/guardians must be contacted by the administration staff so that professional treatment may be organised. Any injuries to a child’s head, face, neck or back must be reported to parents/guardian. Any student who is collected from school by parents/guardians as a result of an injury, or who is administered treatment by a doctor/hospital or ambulance officer as a result of an injury, or has an injury to the head, face, neck or back, or where a teacher considers the injury to be greater than “minor” will be reported on Department of Education Accident/Injury form LE375, and entered onto CASES. Students may be signed out form the Health Centre. Parents who collect children from school for any reason (other than emergency) must sign the child out of the school in a register maintained in the school office. Students who attend the Health Centre may be signed out form the Health Centre. All teachers have the authority to call an ambulance immediately in an emergency. If the situation and time permit, a teacher may confer with others before deciding on an appropriate course of action. All school camps will have at least one Level 2 first aid trained staff member at all times. A comprehensive first aid kit will accompany all camps, along with a mobile phone. All children attending camps or excursions will have provided a signed medical form providing medical detail and giving teachers permission to contact a doctor or ambulance should instances arise where their child requires treatment. Copies of the signed medical forms to be taken on camps and excursions, as well as kept at school. All children, especially those with a documented asthma management plan, will have access to Ventolin and a spacer at all times. The school nurse is responsible for the purchase and maintenance of first aid supplies, first aid kits, ice packs and the general upkeep of the Health Centre. At the commencement of each year, requests for updated first aid information will be sent home including requests for any asthma, diabetes and anaphylaxis management plans, high priority medical forms, and reminders to parents of the policies and practices used by the school to manage first aid, illnesses and medications throughout the year. General organisational matters relating to first aid will be communicated to staff at the beginning of each year. Revisions of recommended procedures for administering asthma, diabetes and anaphylaxis medication will also be given at that time. It is recommended that all students have personal accident insurance and ambulance cover. The College will call for an ambulance if deemed necessary, but will not be responsible for any cost incurred as a result of the call out. Section 2: Accidents and Incidents Reporting/Register When an accident / incident occur, the following is to be undertaken by staff on hand: 1. First aid action is to be taken as required. Send a reliable student if necessary to the office to seek trained first aid assistance and administration assistance. 2. Seek assistance from nearby staff if necessary. 3. Any serious accident or incident is to be reported immediately to school administration. 4. All accidents and incidents are to be reported as soon as possible to the college office and required documentation completed. 5. If an ambulance is called, emergency management will be notified. The college will not be responsible for the cost of the ambulance NOTES: All accidents and incidents involving injury are also to be entered online in the injury management system on CASES21 Incidents to staff may also be notifiable under WorkSafe. All incidents involving staff must be reported to administration. Section 3: Assessment and First Aid Treatment of an Asthma attack If a student develops signs of what appears to be an asthma attack, appropriate care must be given immediately. Assessing the severity of an asthma attack: Asthma attacks can be: Mild - this may involve coughing, a soft wheeze, minor difficulty in breathing and no difficulty speaking in sentences Moderate - this may involve a persistent cough, loud wheeze, obvious difficulty in breathing and ability to speak only in short sentences Severe - the student is often very distressed and anxious, gasping for breath, unable to speak more than a few words, pale and sweaty and may have blue lips. All students judged to be having a severe asthma attack require emergency medical assistance. Call an ambulance (dial 000), notify the student’s emergency contact and follow the ‘4 Step Asthma First Aid Plan’ while waiting for the ambulance to arrive. When calling the ambulance state clearly that a student is having ‘breathing difficulties.’ The ambulance service will give priority to a person suffering extreme shortness of breath. Regardless of whether an attack of asthma has been assessed as mild, moderate or severe, Asthma First Aid (as detailed below) must commence immediately. The danger in any asthma situation is delay. Delay may increase the severity of the attack and ultimately risk the student’s life. Asthma First Aid If the student has an Asthma Action Plan, follow the first aid procedure immediately. If no, Asthma Action Plan is available in the steps outlined below should be taken immediately. The 4 Step Asthma First Aid Plan (displayed in the Health Centre): Step 1: Sit the student down in as quiet an atmosphere as possible. Breathing is easier sitting rather than lying down. Be calm and reassuring. Do not leave the student alone. Step 2: Without delay give 4 separate puffs of a blue reliever medication (Airomir, Asmol, Epaq or Ventolin). The medication is best given one puff at a time via a spacer device. If a spacer device is not available, simply use the puffer on its own. Ask the person to take 4 breaths from the spacer after each puff of medication. Step 3: Wait 4 minutes. If there is little or no improvement repeat steps 2 and 3. Step 4: If there is still little or no improvement; call an ambulance immediately (dial 000). State clearly that a student is having ‘breathing difficulties.’ Continuously repeat steps 2 and 3 while waiting for the ambulance. Section 4: Assessment and First Aid Treatment of Anaphylaxis/Anaphylaxis Management Policy & Procedures What is anaphylaxis? Anaphylaxis is a severe, rapidly progressive allergic reaction that is potentially life threatening. Although allergic reactions are common in children, severe life threatening allergic reactions are uncommon and deaths are rare. However, deaths have occurred and anaphylaxis is therefore regarded as a medical emergency that requires a rapid response. Signs and symptoms The symptoms of a mild to moderate allergic reaction can include: • Swelling of the lips, face and eyes • Hives or welts • Abdominal pain and/or vomiting. Symptoms of anaphylaxis (a severe allergic reaction) can include: • Difficulty breathing or noisy breathing • Swelling of the tongue • Swelling/tightness in the throat • Difficulty talking and/or a hoarse voice • Wheezing or persistent coughing • Loss of consciousness and/or collapse • Young children may appear pale and floppy. Symptoms usually develop within 10 minutes to one hour of exposure to an allergen but can appear within a few minutes. The role and responsibilities of the first aider This principal’s nominee has overall responsibility for implementing strategies and processes for ensuring a safe and supporting environment for students at risk of anaphylaxis. The principal’s nominee will: Actively seek information to identify students with severe life threatening allergies at enrolment. Conduct a risk assessment of the potential for accidental exposure to allergens while the student is in the care of the school. Request that parents provide an ASCIA (Australasian Society of Clinical Immunology and Allergy) Action Plan that has been signed by the student’s medical practitioner and has an up to date photograph of the student Ensure that parents provide the student’s EpiPen® and that it is not out of date. This will be stored in the Health Centre. Ensure that staff obtains training in how to recognise and respond to an anaphylactic reaction, including administering an EpiPen®. Develop a communication plan to raise student, staff and parent awareness about severe allergies and the school’s policies. Provide information to all staff so that they are aware of students who are at risk of anaphylaxis, the student’s allergies, the school’s management strategies and first aid procedures. Ensure that there are procedures in place for informing casual relief teachers of students at risk of anaphylaxis and the steps required for prevention and emergency response. Ensure that any external canteen provider can demonstrate satisfactory training in the area of anaphylaxis and its implications on food handling practices. Allocate time, such as during staff meetings, to discuss, practice and review the school’s management strategies for students at risk of anaphylaxis. Practice using the trainer EpiPen® regularly. Encourage ongoing communication between parents/carers and staff about the current status of the student’s allergies, the school’s policies and their implementation. Review the student’s Anaphylaxis Management Plan annually or if the student’s circumstances change, in consultation with parents. (706) Schools can purchase and use adrenaline injectors for general use in the event of an emergency where no other devices are available, and a student is having a first-time reaction without a medical diagnosis of anaphylaxis. Individual Anaphylaxis Management Plans: Every student who has been diagnosed as at risk of anaphylaxis will have an individual Anaphylaxis Management Plan. The student’s Anaphylaxis Management Plan will clearly set out: The type of allergy or allergies. The student’s emergency contact details. practical strategies to minimise the risk of exposure to allergens for in-school and out of class settings, including: » during classroom activities » in canteens or during lunch or snack times » before and after school, in the yard and during breaks » for special events such as incursions, sport days or class parties » for excursions and camps. the name of the person/s responsible for implementing the strategies. information on where the EpiPen® will be stored. The Anaphylaxis Management Plan will also include an individual ASCIA Action Plan, which sets out the emergency procedures to be taken in the event of an allergic reaction. (ASCIA, the Australasian Society of Clinical Immunology and Allergy, is the peak body of immunologists and allergists in Australia). Section 5: Head Lice Head lice (pediculosis) are tiny insects that live on the human scalp where they feed and breed. While head lice do not carry or transmit disease, they are the most common cause of head itch and scratching which may lead to infection and swollen lymph glands. Therefore, they need to be eradicated. Anyone can catch head lice. Head lice cannot fly, hop or jump. They spread from person to person by head to head contact, and by the sharing of personal items such as combs, brushes and head gear such as hats. Implementation: While teachers and other staff members may believe that a child is infested with head lice, they are not permitted or qualified to search a child’s hair, inspect for head lice, or diagnose a case of head lice. Parents/guardians permission will be obtained before a child’s hair is inspected for head lice. Teachers or staff members suspecting that a child has head lice are to report their concerns to the college nurse who will carry out the necessary inspections. Upon positive identification of head lice, the nurse will ensure that the parents/guardians of any infected child are contacted as soon as possible and informed that their child is to be excluded from attending school in accordance with the Health (Infectious Diseases) Regulations 2001 until the child has been treated. The nurse will ensure all parents/guardians of children in the same class as the infected child will be informed so they can monitor their own child/children. Parent/guardian assistance from home is imperative to keep head lice to a minimum. The nurse will also provide parents/guardians of infected children with information about head lice treatment and prevention On the child’s return to school, the classroom teacher should then send the child to the nurse, who will check the child’s head to ensure the treatment has been successful The nurse will ensure that information relating to the prevention and eradication of head lice appears throughout the year in the college newsletter, particularly at times of heavy outbreaks. If permission is NOT given by the parents/guardians and the child is suspected of having head lice, the matter will be referred to the relevant assistant principal or principal and the parents/guardians will be phoned to collect child. Section 6: Sun Policy Australia has the highest incidence of skin cancer in the world, with two out of three Australians developing some form of skin cancer during their lifetime. Over-exposure to the sun during childhood and adolescence is known to be a major cause of skin cancer. Implementation: All students will be encouraged to wear hats during terms 1 and 4 whenever they are outside. Staff are also encouraged to wear hats when outside. Students will be encouraged to wear a broad-spectrum water resistant sunscreen (SPF30+). Sunscreen will be provided for sport and excursions. However students will be encouraged to provide their own sunscreen whilst at school. Students and staff members are encouraged to wear sunglasses for outdoor use. Whenever possible, outside activities on hot days should be scheduled before 11.00am. Adequate shade structures for students will be provided—particularly over eating areas and leisure locations. Temporary shade structures are to be erected at events such as swimming or athletics. The school newsletter and school assemblies will be used to highlight and reinforce the sun policy. The policy will be published in the student handbook. The school will work in conjunction with the maintenance team to ensure adequate shade is provided. Section 7: Administration of Medication/Distribution of medication procedures The college has an administration of medication procedure which outlines the school’s processes and protocols regarding the management of prescribed and non-prescribed medication to students at this school. All medications, including prescription as well as non-prescription medication, including analgesics, such as paracetamol and aspirin and other medications which can be purchased over the counter without a prescription, are to be administered by school personnel following the processes and protocols set out in the medication management procedures of the school. In order to ensure that the interests of staff, students and parents/guardians/approved persons are not compromised, medication will only be administered with explicit written permission from parent/guardian/approved person, or in the case of an emergency, with permission of a medical practitioner. When administering prescription medication on behalf of parent/Guardian, the written advice received must be supported by specific written instructions on the original medication bottle or container, such as that on the pharmacists label noting the name of the student, dosage and time to be administered. Analgesics can mask signs and symptoms of serious illness or injury and will not, therefore, be administered by the school, as a standard first aid strategy. Therefore analgesics such as aspirin and paracetamol will not be stored in the school’s first aid kit. The principal nominee administering medication needs to ensure that: the right child; has the right medication; and the right dose; by the right route (for example, oral or inhaled); at the right time; and that they write down what they have observed permission to administer medication has been received from the child’s parents/guardians/approved persons or a medical practitioner. The principal nominee will inform teachers of those students in their charge who require medication to be administered at the school. The teachers may be required to release students at prescribed times so they may receive their medications from the principal or nominee. The School register will be completed by the person administering the taking of medication. The school in consultation with parents/guardians and the student’s medical/health practitioner will consider the age and circumstances by which the student could be permitted to self-administer their medication. Ideally, medication to be selfadministered by the student should be stored by the school. However, where immediate access is required by the student, such as in the case of asthma, anaphylaxis, or diabetes, medication must be stored in an easily accessible location. NOTE: It is at the Principals’ discretion to agree for the student to carry and manage his/her own medication. Student Information: Parents and/or guardians are required to keep the school informed of current medical contact details concerning students and any current medical conditions and appropriate medical history. Every student who has a medical condition or illness has an individual management plan that is attached to the student’s records. This management plan is provided by the student’s parents/guardians and contains details of: The usual medical treatment needed by the student at school or on school activities The medical treatment and action needed if the student’s condition deteriorates The name, address and telephone numbers for an emergency contact and the student’s doctor Administration of prescribed Oral Medication: Parents/guardians are required to inform the principal in writing of any prescribed medication that students need to take in school hours. Where medication is required in spontaneous situations, detailed administration instructions should be provided, for example in the case of asthma attacks. Medication Administration Permission Forms are available from the Administration Office and should be completed and signed by the parent/guardian. Certain students are capable of taking their own medication (usually tablets) while other students will need assistance from teachers. This information will be recorded on the individual student’s management plan. Where medication for more than one day is supplied, it is to be locked in the storage cupboard in the school administration office. Section 8: First Aid Kit Contents Consistent with the Department’s First Aid Policy and Procedures the school will maintain a First Aid Kit that includes the following items: an up-to-date first aid book – examples include: First aid: Responding to Emergencies, Australian Red Cross o Australian First Aid, St John Ambulance Australia (current edition) o Staying Alive, St John Ambulance Australia, (current edition) wound cleaning equipment o gauze swabs: 100 of 7.5 cm x 7.5 cm divided into small individual packets of five o sterile saline ampoules: 12 x 15 ml and 12 x 30 ml o disposable towels for cleaning dirt from skin surrounding a wound wound dressing equipment o sterile, non-adhesive dressings, individually packed: eight 5 cm x 5 cm, four 7.5 m x 7.5 m, four 10 cm x 10 cm for larger wounds o combine pads: twelve 10 cm x 10 cm for bleeding wounds o non-allergenic plain adhesive strips, without antiseptic on the dressing, for smaller cuts and grazes o steri-strips for holding deep cuts together in preparation for stitching o non-allergenic paper type tape, width 2.5 cm–5 cm, for attaching dressings o conforming bandages for attaching dressings in the absence of tape or in the case of extremely sensitive skin o six sterile eye pads, individually packed bandages o four triangular bandages, for slings, pads for bleeding or attaching dressings, splints, etc. o conforming bandages: two of 2.5 cm, two of 5 cm, six of 7.5 cm and two of 10 cm – these may be used to hold dressings in place or for support in the case of soft tissue injuries lotions and ointments o Cuts and abrasions should be cleaned initially under running water followed by deeper and more serious wounds being cleaned with sterile saline prior to dressing. Antiseptics are not recommended o any sun screen, with a sun protection factor of approximately 15+ o single use sterile saline ampoules for the irrigation of eyes o creams and lotions, other than those in aqueous or gel form, are not recommended in the first aid treatment of wounds or burns o Asthma equipment (which should be in all major portable kits, camping kits, sports kits, etc.) o blue reliever puffer (e.g. Ventolin) that is in date o spacer device o alcohol wipes Other equipment includes: single use gloves – these are essential for all kits and should be available for teachers to carry with them, particularly while on yard duty blood spill kits vomit spill kits one medicine measure for use with prescribed medications disposable cups one pair of scissors (medium size) disposable splinter probes and a sharps container for waste disposable tweezers one teaspoon disposable hand towels pen-like torch, to measure eye-pupil reaction two gel packs, kept in the refrigerator, for sprains, strains and bruises or disposable ice packs for portable kits adhesive sanitary pads, as a backup for personal supplies flexible ‘sam’ splints for fractured limbs (in case of ambulance delay) additional 7.5 m conforming bandages and safety pins to attach splints blanket and sheet, including a thermal accident blanket for portable kits germicidal soap and nail brush for hand-cleaning only one box of paper tissues paper towel for wiping up blood spills in conjunction with blood spill kit single use plastic rubbish bags that can be sealed, for used swabs and a separate waste disposal bin suitable for taking biohazard waste (note: Biohazard waste should be burnt and there are several companies that will handle bulk biohazard waste) Ice cream containers or emesis bags for vomit. Links to this policy: http://www.education.vic.gov.au/school/principals/spag/governance/pages/recordin g.aspx http://www.education.vic.gov.au/school/principals/spag/health/Pages/supportplanning.as px http://www.education.vic.gov.au/school/principals/spag/health/pages/healthcarenee ds.aspx http://www.education.vic.gov.au/school/principals/spag/health/Pages/studenthealth. aspx http://www.education.vic.gov.au/school/principals/spag/health/pages/firstaid.aspx http://www.education.vic.gov.au/school/principals/spag/health/pages/anaphylaxis.as px http://www.education.vic.gov.au/school/principals/spag/management/pages/medical. aspx http://www.education.vic.gov.au/school/principals/spag/health/pages/medication.as px http://www.education.vic.gov.au/school/principals/spag/health/Pages/caresupport.as px DEECD Medication Policy DEECD Anaphylaxis Policy DEECD Health Support Planning Policy Asthma Society Webpage In use at the college are: Medical authority form – for students who require medication whilst at school Anaphylaxis management plan Diabetes management plan Epilepsy management plan Head lice notification form Asthma management plan Emergency Numbers: Poisons Information Service Ambulance 13 11 26 000 Date Implemented August 2014 Author S.Davenport Approved By School Council Responsible for Review Assistant Principal Review Date August 2017