Sample Medication Policy Template
advertisement

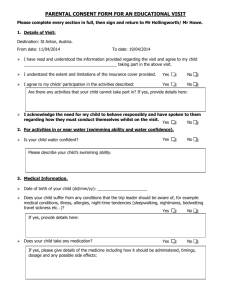
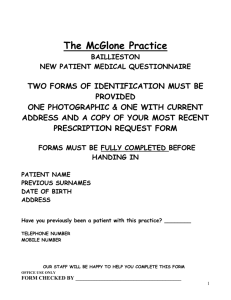
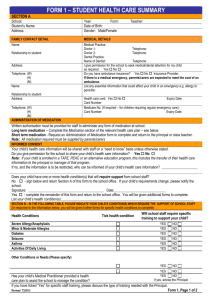
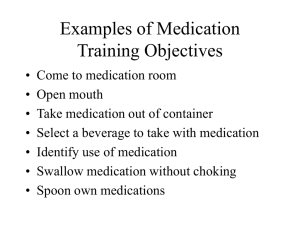
<Service name> Medication Policy Administering medication to a child should be considered a high risk practice. Authority must be obtained from a parent or legal guardian before educators administer any medication (prescribed or non-prescribed). Families place a high level of trust and responsibility on educators when they are administering medication to children, or observing older children self-administer. Services should ensure that their policy and practices regarding medications meet legislative requirements and seek additional medical advice or opinion as needed. It is crucial that educators have some form of professional development training or knowledge of administering medications, in addition to first aid qualifications to ensure that an adverse reaction to medication can be dealt with quickly and responsibly. Services should regularly review policies in collaboration with educators, families, and if appropriate, children; and seek recommendations from recognised authorities. The date the policy is reviewed should be clearly documented on the policy. Policy Number <number> Link to CCQA Principles Family Day Care Quality Assurance (FDCQA) Quality Practices Guide (2004) – Principle 4.3/ Outside School Hours Care Quality Assurance (OSHCQA) Quality Practices Guide (2003) – Principle 6.4 Quality Improvement and Accreditation System (QIAS) Quality Practices Guide (2005) – Principle 5.3 Policy statement <Service name> has a duty of care to ensure that all persons1 are provided with a high level of protection during the hours of the service’s operation. The service’s Medication Policy reflects the following principles: o safe principles and practices to administer medication; o hygiene practices o an acute attention to detail o the maintenance of accurate records o up to date professional development knowledge of administering techniques; o first aid qualifications o licensing and/or legislative requirements o recommended advice and practices from a medical source o open communication between educators, families and children o the accountability of educators when administering medication. An educator will administer medication based on the following principles: o The right child o The right medication o The right dose o The right method o The right date and time For the purpose of this policy, 'persons' include <children, families, educators, carers' family, management, coordination unit staff, ancillary staff (administrative staff, kitchen staff, cleaners, maintenance personnel), students, volunteers, visitors, local community, school community, licensee, sponsor and/or service owner>. 1 Current as at September 2010 Page 1 of 7 These basic principles are the first steps in ensuring that medication is administered safely to any person, and should be documented by the parent or legal guardian before administering medication to a child. Educators should check a medication’s expiry date before administering it to a child. Medication can only be administered when the service’s <medication authorisation form2> has been completed and signed by the child’s parent or legal guardian. In this service, medication is administered to a child by a <educator, manager, coordination unit staff> or in some cases, with parental or guardian consent, medication can be self-administered by a school age child. When medication is being self-administered, children are supervised by educators. The service will endeavour to ensure that educators are witnessed by another person when administering medication to children.3 It is understood by educators, children and families that there is a shared responsibility between the service and other stakeholders that the Medication Policy and procedures are accepted as a high priority. In meeting the service’s duty of care, it is a requirement under the Occupational Health & Safety Act4 that management and educators implement and endorse the service’s Medication Policy and procedures. The service reserves the right to contact a health care professional5 if educators are unsure about administering medication to a child, even if the parent or legal guardian has requested the medication to be administered. Rationale The rationale represents a statement of reasons that detail why the policy and/or procedures have been developed and are important to the service. Please refer to: National Health and Medical Research Council. (2005). Staying healthy in child care: Preventing infectious disease in child care (4th Ed.). Canberra: Author. Strategies and practices These are examples. Services are encouraged to develop and adapt the following strategies and practices as required to meet their individual circumstances and daily best practices. Definition of medication The service has the opportunity to define ‘medication’ in the context of the policy. The term ‘medication’ can be defined either as prescribed or non-prescribed. For the purpose of this policy, ‘prescribed’ medication is: o authorised by a health care professional For the purpose of this policy, ‘medication authorisation form’ is the term used for parents or guardians to grant written consent for a service to administer medication to a child. 3 In family day care schemes and single staff model outside school hours care services, ensuring that a witness can observe another educator administer medication is difficult or not an option. In this situation, services may need to develop practices or strategies that protect educators and reduce the likelihood of a potential incident. 4 There are legislative Acts and regulations for each state and territory that address the issue of Occupational Health and Safety. Services are advised to seek information that is relevant to their jurisdiction. 5 For the purpose of this policy, ‘health care professional’ can include the child’s: medical practitioner (or doctor of medicine), allied health professional, such as a speech therapist, nutritionist or child psychologist. 2 Current as at September 2010 Page 2 of 7 dispensed by a pharmacist with a printed label, which includes the name of the child being prescribed the medication, the medication dosage and expiry date. Medication that does not meet the criteria for prescribed medication, can be considered non-prescribed. This includes over-the-counter medication; medication dispensed by a naturopath/homeopath; or considered complementary or alternative such as vitamins and cultural herbs or remedies. Examples of prescribed medication include antibiotics; Ventolin for asthma; or Ritalin for Attention-Deficit Hyperactivity Disorder. Examples of non-prescribed medication include topical or antifungal creams for nappy rash or eczema; paracetamol; ibuprofen; antihistamine for an allergy; or teething gel. o Handwashing and hygiene practices Services should consider the following reflective questions: o Why do educators or children need to wash their hands before administering medication? o Are there situations when handwashing may not occur before administering medication? For example, school age children may self-administer asthma medication. How can the service encourage children to remember to wash their hands? o Can the service identify when educators may require gloves when administering medication? Maintaining clean and hygienic environments The service can state how some environments need to be hygienically maintained when medication is applied or administered. For example, a baby who has thrush needs to have an antifungal cream applied at each nappy change. Educators will need to follow hygiene practices to ensure that the nappy change mat is safe to use for other children. Services should consider the following reflective questions: o How does the service ensure that hygiene practices are maintained when medication needs to be applied? o How does the service’s hygiene practice change when a child is known to have an infectious illness or condition and medication is required? If so, in what situation and why? o Is there specific equipment required when administering or applying medication which may need to be cleaned? How is this process carried out? Assessing the need for administering medication Services should consider the following reflective questions: o If the medication is non-prescribed, is it appropriate for the child’s signs and symptoms? For example, if the child is coughing and wheezing, how will a paracetamol help the child’s condition if there is no pain or fever observed? Is a decongestant more appropriate? How does the service communicate this respectfully to the child’s family? o If the child is being medicated for an infectious illness or disease, does the child need to continue to be excluded from the service, as per the exclusion guidelines? o How do educators assess a child’s health? o What strategies are in place that support educators when they have decided a child is too ill for care but the family insist that the child should attend care with medication? o Do educators feel comfortable or confident administering the medication? Services can link this section by stating: Please refer to the service’s Illness Policy. Current as at September 2010 Page 3 of 7 Exclusion guidelines The service can state when children can return to the service after an infectious disease or illness, where medication is still being administered. For example, a child can attend care after being diagnosed with impetigo as long as the sores are not weeping and an antibiotic has been administered for more than 24 hours. Services should refer to their relevant state or territory health authority for exclusion guidelines. Services can link this section by stating: Please refer to the service’s Illness Policy. Please refer to the service’s Immunisation and Health Related Exclusion Policy. Assessing the need to administer fever reducing medication Services should consider the implications of administering fever-reducing medication, such as paracetamol, when children are experiencing a high temperature. Services should consult with medical practitioners or hospitalswhen deciding on the practice of administering fever-reducing medications such as paracetamol Authorising the administration of medication This is one of the most important steps in the administration of medication. If the service has not received parental or guardianship authority to administer medication to a child, then it needs to consider the risks of administering medication without consent. It is absolutely crucial at this point to determine a number of important elements, especially for non-prescribed medications, that the service may state in the policy: o Who has recommended the medication? For example, a child’s parent, homeopath or a pharmacist. o Is the medication suitable or recommended for children? o Is the medication appropriate for the child’s age? For example, if the manufacturer’s advice does not recommend for children under two years of age, will the service accept responsibility for administering that medication to a 12 month old (even at the request of the parent)? o Is the medication appropriate for the symptoms or illness? o What happens if the dose is different for weight or age? For example, if a child is heavy for their age, does the service base the dose requirements on the weight of the child or the child’s age? o How does the service respond to a claim “but this is what we always give to her” or “the pharmacist said it was the right dose” when the manufacturer’s recommended dose is not being adhered to? o Has the medication expiry date lapsed? o When was the last dose administered to the child? For example, the time between doses of paracetamol is important. If the parent or guardian requests a time that is not within the manufacturer’s recommendations, what is the action of the service? o Are the recommendations or instructions written in another language? How does the service respond to a family’s request to administer medication that educators are unable to interpret? o Is the child taking a combination of medications? What are the potential risks of administering more than one medication to the same child? Would the service feel more confident with a letter from the child’s health care professional authorising the administration of more than one medication? Medication authorisation form This form may have to comply with state/territory licensing requirements. Services should consider the following reflective questions: o Does the medication authorisation form include the following details: Child’s name who requires the medication Child’s parent or guardian’s name and signature Name of the medication Dose required Current as at September 2010 Page 4 of 7 Method of administration, for example oral, eye, ear, inhaled Time and date of administration Expiry date of the medication Special instructions, such as medication that needs to be administered an hour before a meal or before a child falls asleep Known family history to allergies involving medication. If so, what are the symptoms?6 Storage and disposal of medication The service should state how medication is stored and disposed of, whether in the service or carer’s home. Services should consider the following reflective questions: o Does the service have a lockable cupboard, out of reach from children, where medication can be stored? o How are self-administered medications stored? For example, how does a school age child access their asthma puffer if it is in a locked cupboard? o If medication needs to be refrigerated, is it accessible to children? o How does the service dispose of medication? Is there a pharmacy that can dispose of the medication for the service? o When medication is handed over to the service, does it have the child’s name on it? For non-prescribed medication, is it labelled and in its original packaging? How does the service define ‘original packaging’? o What are the potential risks for the service if it stores medication that is not clearly labelled and does not indicate which child requires it? Administering medication to a child The service should state who is authorised to administer medication in the service. The service should detail a clear step by step procedure that identifies how medication is administered. The procedure should be sourced from either a health care professional or recognised health authority. This ensures that the service is meeting the state/territory legislative requirements and recommended best practice form a heath professional. The importance of a witness The service may decide to state how it ensures that medication being administered is done so safely and with the parent or guardian’s consent by ensuring that there is a witness to medication administration. Family day care carers and single model outside school hours care services, should consider how they ensure that medication is being administered safely and checked for accuracy. Self-administration of medication The service can state, especially for school age children, how it supports the selfadministration of medication. For example, children with asthma or diabetes may have a history at home and at school of self-administering their medication. Services should consider the following reflective questions: o How does the service support and supervise the practice of self-administering medication? o Can children self-administer in a safe and hygienic setting? o How does the service document and communicate to families when children have self-administered medication? o Is there an action plan that assists educators when there is an adverse reaction to the medication? Services should seek advice from a medical practitioner regarding allergies to medications when developing this policy. 6 Current as at September 2010 Page 5 of 7 Documenting the administration of medication Maintaining records Documenting the administration of medication is important so that educators can communicate to families about the child’s health needs. It is important that all medication documentation is stored safely. There may be state or territory licensing regulations that require documentation to be stored for a period of time. Services should state in the policy those requirements. The person administering and the witness, should sign documentation that identifies that they were responsible for administering the medication. Services can link this section by stating: Please refer to the service’s Privacy and Confidentiality Policy. Monitoring after the administration of medication The service can state how it plans to monitor children after the administration of medication. It may be useful to develop a first aid action plan should the child experience an adverse reaction to the medication. Services can link this section by stating: Please refer to the service’s First Aid Policy. Communicating with educators and families Services should consider the following reflective questions: o How does the service communicate to families when children have been administered medication? o How do educators ensure that accurate information is being communicated during a shift change over? Prolonged use of medication Prescribed medication Brief and concise detail of the service’s strategy. Non-prescribed medication Brief and concise detail of the service’s strategy. Experiences Services should consider the following reflective questions: o How can play and learning experiences promote safety and responsibility? For example, a child finds medication in the home and brings it to the service. o How can the service discuss with children about finding an adult and handing the medication to them? o If there is a child who is asthmatic, can educators discuss with children what to do if they observe the child having difficulty breathing? How can educators and children discuss what to do? Is there a recognised plan to help the child assist their peers, such as inform an adult or find the child’s inhaler? o What if a staff/carer has a health need that requires medication and they are alone with children? Excursions Services should consider the following reflective questions: o How does the service ensure that medication can be administered safely and hygienically while on an excursion? o Should a first aid kit be taken on excursions? o What equipment is required while on an excursion to administer medication? o Does the staffing on the excursion include staff with relevant first aid qualifications? o How will the service contact parents/guardians/emergency contact people should there be a medical emergency? Current as at September 2010 Page 6 of 7 o How does the service provide the correct administration requirements for the excursion? Community Services should consider the following reflective questions: o How can the service promote responsible use of medication by using community role models? For example, the service may decide to build links with community organisations, such as a doctor or nurse to visit the service and talk about the safe use of medications. This may be particularly important for children who have ADHD or who see adults use medications consistently in the home. o For services with school age children and operating in areas of high adult drug use, how can the service be proactive in communicating healthy living programs and anti-drug use messages? This may be particularly important if there are high incidences of children seeing used needles in their community. Links to other policies The following are a list of examples: Employment of educators First aid Hygiene and infection control Illness Occupational health and safety Privacy and confidentiality Supporting children’s individual needs Sources National Health and Medical Research Council. (2005). Staying healthy in child care: Preventing infectious disease in child care (4th ed.). Canberra: Author. Further reading Matthews, C. (2004). Healthy children: A guide for child care (2nd ed.). NSW: Elsevier. Oberklaid, F. (2004). Health in early childhood settings. NSW: Pademelon Press. Therapeutic Goods Administration. (2007). Scheduling of medicines and poisons: National Drugs and Poisons Schedule Committee (NDPSC). Retrieved June 28, 2007, from http://www.tga.gov.au/ndpsc/index.htm Useful websites Anaphylaxis Australia – www.allergyfacts.org.au/foodalerts.asp Asthma Foundations Australia – www.asthmaaustralia.org.au Immunise Australia Program – www.immunise.health.gov.au National Health and Medical Research Council – www.nhmrc.gov.au National Prescribing Service – www.nps.org.au Policy created date <date> Policy review date <date> Signatures <signatures> Current as at September 2010 Page 7 of 7