New Directions - Health and Disability Commissioner
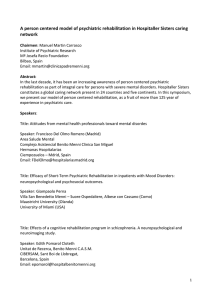
advertisement

New Directions: International Overview of Best Practices in Recovery and Rehabilitation Services for People with Serious Mental Illness - A Discussion Paper Table of contents Acknowledgements I. Introduction Purpose And Context Language About The Centre For Community Change Through Housing And Support, Trinity College Of Vermont II. The Vision and an Image of a Recovery-Oriented Rehabilitation Service System The Vision Image Of A Recovery-Oriented, Integrated Rehabilitation Service System III. Overview of Psychiatric Rehabilitation Definition Of Psychiatric Rehabilitation Core Values Practice Principles Service Outcomes Common Program Models Assertive Community Treatment (P/ACT) Fairweather Lodge Clubhouse or Fountain House Model Psychosocial Rehabilitation Centres Vocational training and support programs Consumer operated programs IV. Recovery Principles in Policy and Practice What Is Recovery? Bases Of Knowledge In Recovery Recovery "Principles" Tools For Recovery Recovery-Oriented Practice In Psychiatric Rehabilitation Programs V. Synopsis of Best Practice Models in Rehabilitation and Recovery-Oriented Services Consumer-operated Programs And Self-help Services Self-help Member-run services Critical elements for success Intensive Case Management Models of intensive case management - Broker Model - Rehabilitation Model - Assertive Community Treatment (P/act) Or The Full Support Model Strengths Model Best Practices in intensive case management Community Support Services (including Supported Housing) Definition of community support services Supported housing Work And Education Support Work preparation, training, and support approaches Vocational outcomes Best practice principles in employment services Family Education and Support Families as support providers and collaborators Families and rehabilitation providers Family-to-family education and support VI. Program Examples Canadian Mental Health Association (CMHA) Canadian Mental Health Association - Timmins, Ontario, Branch Hamilton Program for Schizophrenia, Hamilton, Ontario Journey of Hope - National Alliance for the Mentally Ill, United States Northeast Independent Living Program, Lawrence, Massachusetts Stepping Stone Peer Support Centre, Claremont and Lebanon, New Hampshire Trieste, Italy Village Integrated Service Agency (VISA), Long Beach, California VII. References and Resources VIII. Appendices (NOT available in this online edition) Appendix I Materials List, Centre for Community Change through Housing and Support Appendix II Guiding Principles, Wisconsin Blue Ribbon Commission on Mental Health Appendix III A Position Paper on Recovery and Psychiatric Disability Appendix IV NASMHPD Position Statement on Consumer Contributions to Mental Health Service Delivery Systems Appendix V Teague, Drake and Bond P/ACT Fidelity Scale Appendix VI Best Practices in Housing and Supports for People with Psychiatric Disabilities, National Association of State Mental Health Program Directors Appendix VII NASMHPD Position Statement on Employment of Persons with severe Psychiatric Disabilities Appendix VIII Model Policy on Family Involvement Appendix IX CMHA -- Timmins Branch Program Report for 1995/1996 Acknowledgements Our destiny is to be transformed one by one together. Leonard Roy Frank The development of this paper was sponsored by the New Zealand Mental Health Commission and is intended to inform its initiative to develop a National Blueprint for Mental Health Services which will include a New Zealand-specific rehabilitation and recovery model for adult mental health services. Laurie Curtis, M.A. of the Center for Community Change through Housing and Support of Trinity College of Vermont was contracted to prepare the report by Chris Harris and the Framework Trust, Auckland, New Zealand, on behalf of the Commission. Acknowledgement is given to Fran Silvestry of Monadnock Family Services, Keene, NH; Sue Hallwright, Mental Health Systems Consultant; Derek Wright; and Janet Peters for their review and contributions to the paper as well as to the countless practitioners, researchers, people with serious mental illness, and their family members whose experience, creativity, insight and perseverance help to illuminate and guide our way. I. Introduction In all affairs, it is a wise thing now and then to hang a question mark on the things you have long taken for granted. Bertrand Russell (quoted in Frank, 1995). Purpose and context Mental health services throughout the world are in the midst of unprecedented change. New thinking is emerging about what constitutes "best practice" in mental health services. Community mental health treatment and support services are now the primary locus of care for people with serious mental illness in many areas. Fundamental components of mental health service systems such as methods of designing and delivering services, mechanisms for establishing and funding service priorities, methods of ensuring system accountability, and definitions of staff role, needed competencies, and training approaches, and so forth, are undergoing scrutiny and restructuring. Historic distinctions between clinical treatment services and disability support or rehabilitation services are no longer simple and examples of integrated service systems are becoming more common. In this context, traditional psychiatric hospital services are undergoing a parallel process which is re-shaping their role, services, and position as partners with community treatment and rehabilitation services, disability services, and selfhelp/peer support services in an integrated system. Mental health consumers and their family members are exercising their "voice" and are assuming increasingly vital roles in governance, policy formulation, and service design and delivery which is helping to shape how these changes will occur in our thinking and practice. The New Zealand Mental Health Commission is undertaking to develop a National Blueprint for Mental Health Services to serve as a framework for future service development and funding. The Commission has requested that a New Zealand specific rehabilitation and recovery model for adult mental health be developed for inclusion in the Blueprint. This paper was prepared to provide an overview of some of the international best practices in rehabilitation and recovery to inform this process. It presents some of the guiding principles of rehabilitation and recovery, identifies core "best practices," and describes some of the exemplary programs providing rehabilitation and recovery support services. Three caveats must be noted: 1. The purpose of this paper is to serve as a framework for thinking and discussion. It is beyond its intended scope to provide an exhaustive review of existing models of rehabilitation service or a full inventory of emerging approaches. The choice of programs selected for inclusion in this paper as exemplary is based on the author's experience and exposure to a wide variety of mental health service approaches, the availability of professional literature and descriptive materials about the programs, and their applicability to the New Zealand context. Identifying exemplary programs is like selecting the "best" wine -- there are so many wonderful examples in many different classes and categories, each with a distinctive blend of characteristics, that a definitive "best" is difficult to establish. 2. Because the focus of this paper is primarily on rehabilitation services, other critical core services of a comprehensive mental health service system are not addressed herein. Specifically, crisis response and emergency services, psychopharmacology and other forms of psychiatric treatment, and hospital based care are not discussed, but these components are often critically important to individuals in the process of recovery from mental illness and/or psychiatric disabilities. It is also increasingly important for traditional clinical treatment and disability support services to look at the interface of their services and expand the region of collaborative overlap. For many, using rehabilitation focused skill building models to help individuals to develop coping skills for symptom selfmanagement and self-medication, for proactive crisis planning, and so forth are essential elements in the recovery process. 3. The terminology used in the mental health field is often vague. At present, the field lacks universally accepted definitions for terms such as "case management," "community support services," "supported employment," and so forth. When these terms are defined, they are defined within a local or regional context. Consequently, two different communities may both have "community support services" but literally be offering very different services and operating from different service. This results in considerable confusion for funders and providers, as well as ministers, consumers, carers and others. While every effort is made to be clear about term used in this report, it is very important to read beyond the program names or terms used and to focus on the description of the services provided in order to understand exactly what is being discussed. Language Many terms have been used to denote individuals with personal experience with psychiatric problems, histories, and labels. Client, patient, member, and consumer are in common use, as are ex-patient and survivor. Lately, some people are preferring to use the lengthy term consumer/ex-patient/survivor, or c/s/x for short, in order to emphasize that not all people with psychiatric experiences are consumers of the mental health system. However, not one specific term is fully accepted by the mental health field or by all consumer advocates, and the search continues for respectful language to describe the experience of persons with psychiatric histories which will be generically accepted by all. This paper will use a variety of terms and will specifically reserve the terms "clients" and "members" to distinguish individuals with a specific relationship with a service providing agency. "Person first" language is used throughout the paper and attention is given to balancing gender-based terms. ABOUT THE CENTRE FOR COMMUNITY CHANGE THROUGH HOUSING AND SUPPORT, TRINITY COLLEGE OF VERMONT Established and directed by Dr. Paul J. Carling, the Centre for Community Change is a consultation and training organization which provides system change consultation, information dissemination, organizational development, and workforce development to mental health systems and agencies around the world. With over a decade of experience, the Centre's work combines values of empowerment, community integration, and recovery with planning, program development, and training skills to help design consumer-guided, familysupporting, and outcome-focused systems of care. Key services and products offered by the Centre include: technical assistance in systems change (including hospital downsizing) and services development; rehabilitation and recovery skills training; best practices in case management; "wrap around" services for children, youth, and families; clients at high risk or with high needs; crisis prevention, intervention, and resolution; and supported housing. A list of materials available through the Centre is found in Attachment I The Centre, through Trinity College of Vermont, also offers the Graduate Program in Community Mental Health (PCMH) as an alternative to traditional academic programs. Specializations are available in services for adults with serious mental illness, and children and adolescents with serious emotional disturbances and their families. II. The vision and an image of a recovery-oriented rehabilitation service system The problem that we're facing is that, similar to people with physical or developmental disabilities, the mental health system, and a large part of the general public, believe that we are not capable of living independently, and believe that we must live and work in situations which give us care and treatment for the rest of our lives. That's the myth we have to debunk. Howie the Harp, Advocate (quoted in Carling, 1995) This section offers a vision and an image of a recovery-oriented and integrated mental health system that draws from the best practices outlined in this paper. It articulates a set of ideal outcomes desired by integrated and inclusive mental health services, outlines general recommendations for basic components of a recovery-oriented rehabilitation system, and provides a standard by which to prioritize and to evaluate change efforts. THE VISION Individuals with a psychiatric disability (or serious mental illness) have access to resources that strengthen self-determination and self -sufficiency by promoting health and wellness, improvement and recovery, quality of life and dignity. People live in integrated housing which they have selected from a range of options in their community; work in regular jobs they have chosen; have positive relationships with their families; and have mutual and caring friendships. Self-help and peer support is widely available in all communities through friends, family, co-workers, informal networks of people with shared experiences, and consumer-operated resources and services. Formal mental health services and supports respect and reflect the context of people's economic, cultural and social situations, are based on the latest relevant knowledge and best practice, are consumer guided, and family/carer supporting. Efforts to change negative public attitudes and their resulting behaviours, such as discrimination, are active at local, regional and national levels and involve the collaborative efforts of people with psychiatric disorders, their family members and carers, and professional mental health service providers. Users of services have the resources and authority to hold service providers accountable for the quality of services they receive. They have a central role in developing, governing, delivering, and evaluating services. IMAGE OF A RECOVERY-ORIENTED, INTEGRATED REHABILITATION SERVICE SYSTEM A recovery-oriented, integrated rehabilitation service system will include the following. 1. A shared vision and image of an integrated, recovery-oriented mental health system, grounded in the goals, needs and wants of consumers and family members/carers, which will help to guide the development, funding, and evaluation of all clinical, disability/rehabilitation, and self-help/peer support services. Individual missions of all services demonstrate how the service achieves the over-arching vision. 2. A set of guiding principles developed and adopted by all stakeholders to further guide the operations of the system. These guiding principles should include elements such as those adopted by the Wisconsin Blue Ribbon Commission on Mental Health (1997) (Appendix II). 3. Definition of a set of positive consumer and system outcomes which are reflective of the vision and principles and to which all components of the system will be held accountable, including performance contracts, funding mechanisms and priorities, workforce development, program and service evaluation methodologies, and so forth. The Wisconsin Commission on Mental Health (1997) identified 15 desirable outcomes and grouped them into three categories as follows. The fourth category of outcomes are system outcomes added by the author. A. Energizing Outcomes: Consumer Satisfaction; Empowerment and Selfesteem; Access; Personal Safety; Awareness; and Equal Opportunity. B. Clinical Outcomes: Symptom Relief; Psychological Well-Being; Physical Health. C. Community Living Outcomes: Social Relations and Supports; Meaningful Activities and Occupations; Goal Attainment; Basic Survival and Housing; Freedom from Substance Abuse; Daily Living Skills. D. System Outcomes: Services Availability; Effective Services with Demonstrable Outcomes; Diversity in Service and Support Options; Optimal Hospital and Community Service Utilization; Reasonable Cost Containment; Competent Workforce; Stakeholder Satisfaction. 4. A collaborative network of clinical service providers, disability/rehabilitation service providers, and consumer operated self-help and peer support providers is nurtured. These providers are: •Cross-trained in recovery-oriented principles, tools, and best practices; •Expected to develop and rewarded for implementing collaborative initiatives; •Committed to the importance of consumer and family/carer input and impact on governance and policy decisions; •Which have flexible resources sufficient to individualize and tailor services and supports as needed. 5. A range of self-help, peer support, and consumer-operated services are in place throughout the system. This includes employing mental health consumers as staff and service providers in multiple ways in traditional agencies; funding a range of consumer operated services; and providing necessary supports to ensure the success of these ventures, including but not limited to skill building opportunities, leadership training and mentorship, and on-going technical assistance as needed. Mental health consumers are welcomed as partners in care. 6. Redirect responsibilities for basic social and recreational activities currently handled by many rehabilitation programs to consumer-operated wellness centres and "drop-in" programs. 7. Focus rehabilitation service resources on establishing and supporting a range of meaningful employment, education, and vocational options. These would include agency affiliated co-operatives, independent consumer-run businesses, supported employment and supported education services. 8. Increase the availability of mobile community support services to assist with day-to-day skills training and support activities. Increase the capacity of community support services to access commercially available housing options and to provide support for individuals in a range of accommodation types. For many persons, community support workers may also function as "less intensive" case managers and provide futures planning, relapse prevention, crisis planning, and linkage/referral services integrated into the basic support and service package for the people they serve. 9. Establish Intensive, Strengths Based, Assertive Community Treatment Teams, particularly for individuals identified with intense or complex needs, who have high rates of hospital utilization, and who have concurrent problems with substance abuse, homelessness, legal problems, and so forth. These teams should be available 24 hours/day, 7 days a week and draw on all the best practices for engagement, harm reduction, community network development, and recovery-oriented intervention. 10. Create a range of crisis response options which are partnerships between clinical services and disability services. Such options should include crisis planning and relapse prevention activities, respite options, 24 hour mobile crisis intervention availability, hospital diversion programs and so forth. Both hospitals and community services should share in incentives to reduce unnecessary hospital utilization. 11. Widely train clinical and disability service providers, mental health consumers and consumer-service operators in recovery principles and practices (See Appendix III for a plan developed by the Vermont Department of Mental Health). Promulgate knowledge widely. Specify that the sparking and fuelling of personal movement towards recovery, teaching and supporting use of recovery tools, and coordinated relapse prevention and management activities are the responsibility of ALL members of the mental health community and defies clean categorization as either a clinical, rehabilitation, or self-help service. All traditional and peersupport service providers must encourage and facilitate each individual's ability to self-manage the disorder, its symptoms, and associated disability. 12. Encourage and provide resources for family education and support activities offered both within and external to the traditional system. 13. Address the stigma and devaluation associated with mental disorder within the general population. However, the first level of action must be to confront the stigma and discrimination found within the mental health system itself: language, staff attitudes, organizational structures and policies, centralization and concentration of power, discrimination in hiring, and so forth. III. Overview of Psychiatric Rehabilitation To Rehabilitate: a restoration to effectiveness by training. Concise Oxford Dictionary It must be borne in mind that the tragedy of life doesn't lie in not reaching your goal. The tragedy lies in having no goal to reach. Benjamin E. Meyers DEFINITION OF PSYCHIATRIC REHABILITATION Psychiatric rehabilitation (also known as psychosocial rehabilitation and biopsychosocial rehabilitation) is the process of assisting people to acquire and to use, the internal and external skills, supports, and resources necessary to be successful and satisfied living, learning, and working in the environment(s) of their choice. At its most basic level, psychiatric rehabilitation seeks to help people to determine and prioritize their goals, to identify paths for achieving these goals, and to develop the needed skills and supports to achieve these goals (Anthony, Cohen, Farkas, 1991). Derived from concepts from physical rehabilitation, psychiatric rehabilitation focuses on the disability or impairment resulting from an individual's psychiatric disorder which affects the person's ability to fulfill role expectations. The goal of psychiatric rehabilitation is to help individuals to function "despite" their disability - to compensate for or to eliminate deficits in functioning, interpersonal barriers, and environmental barriers created by the disability, and to restore ability for independent living, socialization, and effective life management. Perceived deficits frequently fall into several categories: daily living skills, social interactions, accommodations, vocational productivity, and problem solving (cognitive processes). Psychiatric rehabilitation services offer 1) skill development, and 2) environmental resource development, in order to help individuals capitalize on their personal strengths, to develop effective coping strategies, and to develop supportive environments so that they may function as independently as possible. Service and support activities are designed to be integrated with the real activities one engages in daily. Rehabilitation services may be offered in a facility setting or "off-site" in the community-at-large or in an individual's home (Hughes, 1994). Rehabilitation services may be offered parallel to, independently of, or integrated with psychopharmacology and other forms of psychiatric treatment. CORE VALUES The following statement of core values was produced by the International Association of Psychosocial Rehabilitation Services (IAPSRS). Core Values Statement The International Association of Psychosocial Rehabilitation Services believes ... A. That all people have the capability to learn and grow. B. That a pluralistic approach to the development and provision of psychosocial models and services will best meet the needs of people who choose to use these services. C. That all people should be treated with respect and dignity. No one should be labelled or discriminated against based upon their disability, dysfunction, illness or disease. D. That the involvement of consumers of service is essential to effective operation, evaluation and governance of mental health services. E. That diversity, racial, ethnic, gender identity, and sexual orientation, should be promoted at all levels of the organization and its member agencies (boards, administration, staff, clients and families). F. That people have the right to direct their own affairs, including services they may receive, related to a mental health disability. G. That programs and practitioners should constantly strive to improve the services which they provide. PRACTICE PRINCIPLES The Centre for Psychiatric Rehabilitation in Boston, Massachusetts, identifies the following principles as basic to the practice of psychiatric rehabilitation and suggests that they operate independently of both the settings in which they are practised and the professional disciplines of those practising them (Anthony, Cohen and Farkas 1991, p. 64). •The primary focus of psychiatric rehabilitation is on improving the competencies of persons with psychiatric disabilities. •The benefits of psychiatric rehabilitation for clients are behavioural improvement in their environments of need. •Psychiatric rehabilitation is eclectic in the use of a variety of techniques. •A central focus of psychiatric rehabilitation is on improving vocational outcomes for persons with psychiatric disabilities. •Hope is an essential ingredient of the rehabilitation process. •The deliberate increase in client dependency can lead to an eventual increase in the client's independent functioning. •The two fundamental interventions of psychiatric rehabilitation are development of client skills and development of environmental supports. •Long term drug treatment is often necessary but rarely sufficient component of a rehabilitation program. SERVICE OUTCOMES Outcomes commonly associated with psychiatric rehabilitation (Dion & Anthony, 1987; Cook and Jonikas, 1996) include the following: •Reduced hospitalization re-admissions, lengths of stay and other measures of hospital utilization; •Positive gains in employment status; •Skill development in cognitive, emotional, social, and physical skills; •Client satisfaction; •Stability in accommodations; •Improvements in perceptions of quality of life. COMMON PROGRAM MODELS There are a variety of ways in which psychiatric rehabilitation services have traditionally been arranged in order to actualize the principles identified above. These are very briefly outlined below and include the more traditional facilitybased programs which may be found in communities and hospitals throughout the world and the more recent emphasis on services and supports which are integrated into the natural rhythms of how people in a community typically live, work, and relax. Recently there has been an increased interest by funders, advocates, and providers in learning which of these models, or elements of the models, are most the effective in delivering the desired outcomes -- and for whom (Cook and Jonikas, 1994). This research does suggest that outcomes are more generalizeable to the "real world" when the training and support is provided in vivo -- in the place and at time of need -- rather than in "specialized" mental health environments (Anthony, Farkas, Cohen, 1991). This emerging research forms the basis for the "best practices" outlined in this paper. •ASSERTIVE COMMUNITY TREATMENT (P/ACT): Integrates the delivery of case management services with in vivo skills training in people's homes, places of work, and neighbourhoods. Variations include intensive case management, continuous care teams, and community support services. (See further discussion in this paper.) •FAIRWEATHER LODGE: Individuals live together in a "lodge" which is run by the residents and support staff. Members of the lodge typically operate a small business together which supplements incomes and provides daily structure (FAIRWEATHER, 1980). •CLUBHOUSE or FOUNTAIN HOUSE MODEL: Site-based programs where members are actively involved in operating the day-to-day business of the club. Program typically operates social/leisure activities as well as pre-vocational skills development and transitional employment services (Beard, Probst, and Malamud, 1982). •PSYCHOSOCIAL REHABILITATION CENTRES: Site-based programs which provide social/leisure and education programs, as well as skill training groups to teach daily living skills, interpersonal skills, conversational skills, and various vocational preparation skills. May include some residential rehabilitation services (Dincin, 1975; Liberman, 1993). •VOCATIONAL TRAINING AND SUPPORT PROGRAMS: Historically, sheltered workshops provided skill assessment and work-focused activities. Current increase in programs offering other vocational services such as career planning, job placement, job clubs for worker support, and integrated work opportunities through industrial enclaves, work crews, supported employment, and consumeroperated businesses. (See further discussion in this paper.) •CONSUMER OPERATED PROGRAMS: Typically facility-based "drop-in" program which emphasizes member controlled and operated peer support, advocacy, psycho educational, and social services. May include peer operated warm-lines, outreach, and case management services. (Further discussion in this paper.) IV. Recovery Principles in Policy and Practice In the process of recovery we make progress and we slide back. We live through the vicissitudes of hope and despair and above all we learn to survive, not just as victims, but as people who can turn reaction into action that is self-directed. Thus we never GET recovered. We are always on the way. Patricia Deegan (in Weisburg, 1995) One of the most prevalent and persistent mistakes we make about individuals with psychiatric disorders is thinking that we have learned well enough what they want and need, and know well enough their deficits and limits in leading satisfying lives. Sue Estroff (in Weisburg, 1995) We must be our own heroes. There is no one coming who can reach out and fix me. We need to do something about it ourselves. Lionel Aldridge (in Weisburg, 1990) WHAT IS RECOVERY? Lefley (1994) notes that there is an artificial distinction between "cure" and "care" in western cultures which influences how clinical and disability services are conceived and delivered. Many treatment and rehabilitation programs for persons with mental disorders provide care, symptom management, and assistance in coping with concurrent disabilities, but these services have frequently given up hope of individuals achieving significant amelioration of the underlying disorder. Additionally, many of these programs chose to "treat" people in compartmentalized programs, outside of the fabric of their community, social, and family lives. Weisburg (1994) suggests that a vision of recovery transcends the arguments about whether severe mental illness is caused by physical and/or psychological, sociological, or spiritual factors. It means growing beyond the experience of having (or being labelled with) a mental illness and developing a new meaning and purpose in one's life. Deegan (1997) describes recovery as, in part, emerging from an individual, rather than being imposed upon an individual. The goal of recovery is to "meet the challenge of the disability and to re-establish a new and valued sense of integrity and purpose within and beyond the limits of the disability. The aspiration is to live, work, and love in a community in which one makes a significant contribution (1988)." Mead (1997) characterizes recovery as role-reclamation and the shift from seeing oneself primarily in as "patient or sick person" to asserting an identity which fully embraces the roles of other persons of similar age, gender, culture, and background: worker, parent, lover, friend, retiree, tenant, home-owner and so forth. She emphasizes the need to move beyond perceptions of disability which can perpetuate self-limitations and learned helplessness. Alcoholics Anonymous (AA), a originator of may concepts which characterize recovery in addictions treatment and self-help/peer support, is clear that recovery requires participatory self-management: an individual must be active participating in making changes his/her about values, beliefs, and a way of living. There is no room for passively waiting to be "cured." AA also makes it clear that this personal commitment to action must be long term, that the recovery process is an ongoing, individual, and non-linear, and that it requires on-going support from people with shared experiences (Brown, 1983). Carling (1995) emphasizes social action as a core element in the recovery process. "Persons in powerless positions must come to an awareness of their own oppression before they can embrace change. They must understand the nature of that oppression, and then chose to assert their power in order to resist the oppression (p.109.)" The rise of consumer advocacy organizations and the peer support movement in many ways is reflective of this view of recovery. Many individuals comment on how important this movement has been to their own recovery both in terms of their own empowerment and because of the inspiration, validation, and guidance they receive from finding other people who have "been there" and are "making it." Copeland (1994) identifies the following as core elements of recovery. •Hope -- belief that change and a better life is not only possible, but attainable. •Personal Responsibility -- not counting on others to solve one's problems or "cure" the disorder, but relying on one's self with help from others. •Self-Advocacy -- re-establishing control over one's personal life, rights, responsibilities. •Education -- learning about the disorder, ones self, what can be done, what is available to help. •Support -- assistance from friends, family, and professional health/mental health care givers. The following definition of recovery in psychiatric disability was developed by participants in recovery skills training program and sums up many of these perspectives (Copeland, Curtis and Palmer, 1996). RECOVERY is a process and an attitude, not a place. It is about regaining what may have been lost: rights, roles, responsibilities, decisions, potential, and support. It is not about symptom elimination, but about what an individual wants in his/her life, how he/she can get it, and how others can help/support the individual to get there. It is about rekindling hope for a productive present and a rewarding future -- and believing that one deserves it! Recovery involves people having a personal vision of the life they want to live, seeing and changing patterns, discovering that symptoms can be managed and doing it, finding new ways and reasons for doing it, and doing more of what works and less of what doesn't. Recovery is about reclaiming the roles of a "healthy" person, rather than living life as a "sick" person. Recovery is about getting there. While there is a plethora of ideas about what constitutes the recovery process, there is no clear-cut consensus at this point. The essence of recovery focuses on the subjective experience each consumer and each person's approach to recovery is unique. It is therefore important to understand how each individual chooses to define his/her experience with psychiatric symptoms and the meaning he or she gives to this experience in their life (Hatfield, 1994). The complexity and personal richness of recovery will be lost if left to professionals to define in isolation from consumers (Mowbray and Moxley, 1997). BASES OF KNOWLEDGE IN RECOVERY Curtis (1997) characterizes recovery as drawing from, but simultaneously transcending, at least three bases of knowledge: medical/clinical "treatment," psychiatric rehabilitation/skill focused coping; and self-help and peer support. (Note: some advocates may add additional points to this model such as spirituality.) Medical/Clinical treatment While each of these three components are important, rarely is any one of these components in isolation of the others, sufficient to kindle and/or foster the recovery process of any individual. Each of these components should be seen as valuable tools to be used by the individual to reach personal growth goals as he/she sees fit. There is some suggestion, however, that consumer service provision/peer support may be an essential feature of any support system devoted to recovery (Mowbray and Moxley, 1997). From the perspective of formal mental health services, self-help and peer support are the "newest kid on the block." While self-help and peer support have been around since the beginning of time, it has only been in the past decade or so that people who experience serious mental illness and their family members have begun to organize into independent groups to share information and provide mutual support. Even more recently, these groups are beginning to receive mental health funding to operate more formal peer-support services. Anecdotal and research evidence suggests that self-help and mutual aid are core supports for persons in recovery and must be considered as equal partners with the better funded, more traditional clinical and rehabilitation services. However, there is legitimate concern that the concept of recovery, with its deep roots in self-help, self-advocacy and empowerment, is being co-opted by professional rehabilitation services and turned into another treatment process or program. RECOVERY "PRINCIPLES" This set of "principles" is derived from the work of a number of c/s/x, professionals, and researchers in an effort to establish an initial understanding of recovery in the context of psychiatric disability (Blanch et al, 1995; Anthony, 1993). •Recovery is an active, ongoing, and individual process. •Recovery is not linear; it entails growth, plateaus, setbacks, side tracks, and fast tracks. •"Recovery" relates not only to the experience of symptoms, but also to the secondary assaults of stigma, discrimination, and abuse. •Hope is the most fundamental factor in recovery. •The presence of people who believe in and stand by the person are required. •Recovery can occur without professional intervention. •The establishment of a sense of control or free will is critical to recovery. •"Remembering your track record" -- learning from observing your own mental and emotional behavior -- is critical for coping. •Self-directed coping strategies are effective and can be learned. •Maintaining or developing connections to valued activities and people is critical to the recovery process. •Connecting with other people on a human level is important. •Recovery is a process of "finding meaning in your experience." TOOLS FOR RECOVERY There is a rich body of knowledge accumulating in the literature and in practical experience about specific tools and strategies which people use to cope on a day-to-day basis with the symptoms of psychiatric disorders. Deegan (1995) has developed Coping with Voices: Self Help Strategies for People who Hear Voices that are Distressing. Based on national surveys in the United States of ways that individuals manage their illness, Copeland (1992;1994; 1996) offers the following as some of the tools of recovery. Copeland and the Center for Community Change have been collaborating to develop training curriculum on the use of these tools for consumers, their family members, and practitioners. •Find other people who've "been there" and learn from them. •Build up-front awareness and understanding of self, patterns, preferences. •Identify triggers and early warning signs. •Self monitoring of patterns, changes. •Explore, identify, implement personal techniques for reducing symptoms. •Create and maintain personal support network. •Develop a lifestyle that enhances wellness. •Find things to do and believe in that are important and meaningful to you. •Attend to crisis prevention/planning/advance directives. RECOVERY-ORIENTED PRACTICE IN PSYCHIATRIC REHABILITATION PROGRAMS Is recovery the same as rehabilitation? No. While rehabilitation services may offer help with learning skills, building resources, creating personal networks, accommodation and vocational support, and developing life goals, rehabilitation services cannot and should not be construed as recovery programs. Those that commit to making significant changes in policy, practice, and power distribution in their services, may at best, become recovery-oriented services. Deegan (1988) conceptualizes recovery as the "lived experience of rehabilitation" and Powell and Knight (1992) similarly characterize recovery as a form of "self-directed rehabilitation." Despite the increasing propensity of rehabilitation programs to reframe their services as "recovery"oriented, the strongest recovery-oriented programs identified to date are those which arise from and are operated by skilled consumer providers. Like traditional programs, these services may have a variety of foci such as peer advocacy, peer support, health and wellness education, community organizing, crisis respite, social recreational activities, and so forth. They are offered both in collaboration with and as alternatives to more traditional services. These programs tend to be more reflective of Deegan's "emerging from rather than imposed upon" principle (1997). Moller and Murphy (1997) outline a program and process for integrating rehabilitation, recovery, and relapse prevention activities in fairly standard rehabilitation programs. Miller's model is based on wellness education, self assessment and monitoring tools, and on-going support to implement the lifestyle changes needed to manage symptoms and symptom triggers. They provide a good example of how clinical and disability oriented services can be blended to create effective recovery-oriented supports and services. Studies on this model indicate decreased inpatient days, cost savings, excellent participant satisfaction, and replicability of results over time within the program. Recovery is not something that is "tacked on" to existing programs as another offering. For a rehabilitation program to become recovery-oriented requires a radical re-alignment of its fundamental beliefs, services and practices, anticipated outcomes, power dynamics, and relationships with the people it serves (Curtis, 1997). The challenge for rehabilitation services is to ruthlessly identify what aspects of our programs helps to spark and to foster the recovery process in individuals and which components do not. It is a question of HOW we go about doing our work as much, if not more, than an analysis of WHAT work should be done. •How do rehabilitation services both help and hinder the recovery process of each individual they serve? •How are the principles outlined above operationalized in day-to-day policy and practice? •How to we restructure our relationships with people so that power is shared equally among professional staff, consumers, and family members? •What do mental health staff need to know in order know how to create relationships and environments which stimulate and foster recovery? The Vermont Department of Mental Health has recently embarked on a course of trying to create a recovery-oriented mental health service system. A position paper outlining their present plan for shifting the system in this direction (Appendix III) provides specific strategies for each of five commonly identified dimensions of recovery: •Hope •Information, knowledge, and skills •Sense of control and personal responsibility •Trusting relationships with health care providers •Self-help and peer support (Vermont Department of Mental Health, 1995). V. Synopsis of Best Practice Models in Rehabilitation and Recovery-Oriented Services Among my many paths I slowly extend myself and resurfacing from years mired in solitary darkness I reach out and discover sunlight illuminating a new world. Sandra Harper (in Weisburg, 1995) Let us try again to connect with each other as two human beings, neither of which has all the answers, both of which have chosen to work together. Laura Mancuso (1995) Best practices can be considered activities and program approaches which are in keeping with the best possible evidence of what works. Empirical studies of the efficacy of different service approaches help to provide a foundation for best practices. But best practices are not always found in the literature. There are a number of unstudied approaches which appear promising and compatible with desired philosophical and/or political principles and goals. Descriptions of best practices may resemble descriptions of ideal service delivery systems rather than reflect the specific realities and constraints of service delivery. Yet, taken together, best practices form a road-map for system change and establish benchmarks by which incremental progress can be measured (Goering, in preparation). Five best practices for rehabilitation services are outlined in this section. 1) Consumer operated programs and self-help services; 2) Intensive Case Management (ICM) which includes Assertive Community Treatment (P/ACT); 3) Community Support Services which includes Supported Housing; 4) Work and Education Support; 5) Family Support and Education. In the following section, specific programs which exemplify these best practices will be described. Some of the best practices presented here been well defined and described in the literature: Intensive Case Management (ICM) which includes Assertive Community Treatment (P/ACT); Community Support Services which includes Supported Housing; and Vocational support approaches. The other two are less well established in the research and typically have a much smaller funding base: Consumer operated programs and self-help services; and Family Support and Education. Consumer-Operated Programs And Self-Help Services SELF-HELP Self-help is based on the premise that people with a commonality such as a shared personal experiences or characteristics, have something to offer each other that cannot be provided by professional service providers. There are growing numbers of consumer-operated programs and self-help services in the United States, Canada, New Zealand, and elsewhere in the world. The recognition and expansion of these groups is due in part to an increasing understanding about their efficacy and utility in the service array, and in part because they tend to be very cost effective for funders. These types of programs often have higher appeal to individuals who are homeless and/or have a dual diagnosis of mental illness and substance abuse disorder than do traditionally operated programs (Segal, Silverman and Temkin, 1995). The mental health self-help movement is comprised of many different types of groups, often embracing divergent philosophies (Chamberlain, 1990). For example, the U.S. National Depressive and Manic Depressive Association promotes an illness model of mental disorder; Recovery, Inc. advocates for selfhelp in conjunction with traditional psychiatric treatment; while the Support Coalition International members view themselves as liberationist. There is empirical support for the establishment of self-help and consumer operated programs. Studies of these programs repeatedly document positive outcomes reported by the persons who use these programs (Chamberlain, Rogers and Ellison, 1996; Segal et al, 1995; Kaufman, 1995; Haas and Mead, 1996). However, these programs sustain primarily because (and only when) their members find them effective as sources of support and assistance in solving personal problems. The activities of consumer operated and self-help services may include: •Mutual support •Advocacy •Cultural activities •Knowledge development and skills training •Public education •Education of professionals •Economic development •Social policy advocacy (Goering, in preparation). Self-help groups are sometimes sponsored by traditional service agencies and there is considerable debate about the appropriateness of professionals facilitating or even being present at group meetings. The inclination of many mental health professionals and consumers is to perpetuate professionally driven groups under the guise of self-help. Agency sponsored self-help groups must be a "hands off" activity for the sponsor. MEMBER-RUN SERVICES There is a growing number of consumer-operated or member-run initiatives which may entail all or most of the staff and leadership being mental health consumers. In these organizations the Board of Directors or other governance group is minimally 51% mental health consumers. There have been some advocacy efforts to have mental health authorities set aside a minimum budget of 1% of their total budget to fund consumer operated initiatives, but this level of support is not wide-spread. New Hampshire has funded a number of consumer run non-profit organizations that provide peer support and wellness activities. The Canadian Province of Ontario has to date funded 36 Consumer/Survivor Development Initiative (CSDI) projects. Six are cooperative businesses, one is a provincial business council which provides support to current and new consumer businesses, and 28 are local organizations which provide a mixture of education, peer support, and other activities which reflect their interests. Self-help groups or member-run services should have the following features (Chamberlain, 1988): •The provide help with needs as defined by members; •Participation is completely voluntary; •Members choose to attend only those activities they wish without being required to attend specified services or activities; •Help is provided by members one to another in mutually supportive fashion; •Overall direction of the organization, including responsibility for financial and policy decisions, is in the hands of the membership; •The responsibility of the organization is to the member and not to relatives or to treatment institutions. It is notable that 17 states in the United States now have Consumer Affairs Directors at the state level and that many managed care organizations are hiring mental health consumers to provide leadership for their consumer-operated initiatives. The United States' National Association of State Mental Health Program Directors (NASMHPD) approved a strong statement of support for consumer contributions to mental health service delivery systems (Appendix IV). Many state mental health authorities are requiring that consumers and family members have a majority of seats on the governance and/or advisory boards of all agencies and organizations under contract to the authority and beginning to identifying practical ways to ensure that participation is valued and impact-full, rather than token (Kanapaux, 1997; Van Tosh, 1994; Vandergang, 1996; Curtis et al. 1991). CRITICAL ELEMENTS FOR SUCCESS Goering's (in preparation) review of the literature in this area suggests that there is sufficient evidence to support the premise that self help should be a funded part of any mental health reform strategy. Key issues in the success of consumer-operated organizations and self-help groups include: •Recruitment and retention of strong, competent leadership requires casting a "wide net" in recruitment, leadership development activities and leadership secession planning. •Availability of professional skill development opportunities in management, group facilitation, accounting, and other core competencies; This may involve hands-on technical assistance, specific training curriculum, mentorship and formal and informal supervision. •Reasonable accommodations and flexibility in performance standards. •Education of the public and mental health professionals about the viability and value of self-help approaches. •Ongoing evaluation of the effectiveness of selfhelp and consumer-operated services which is viable in terms of research design, sufficiency of resources, and applicability to the culture of the organization. •Adequate standards for fiscal accountability of public funds which provide both clear expectations, reasonable amounts of flexibility, and proactive technical assistance where needed. There is increasing literature and curriculum available to help develop leadership, system advocacy, board participation skills, and program management abilities among mental health consumers and family members (Curtis et al. 1991; Valentine and Capponi, 1989; Anderson and Deegan, 1994; Scott, Pomeroy, Pape, 1995; Vandergang, 1996). Many of these initiatives are consumer designed and delivered, but certainly not all. The West Virginia Office of Mental Health, in partnership with the West Virginian Mental Health Consumers Association and the West Virginia Alliance for the Mentally Ill, has established a Leadership Academy for Consumers and Families (Nelson and Edmonds, 1997). In Toronto, Ontario, a Consumer/Survivor Development Initiative, a component of the Canadian Mental Health Association (CSDI) offers leadership information, resources, and support (CSDI, 1993; 1996). Intensive Case Management A variety of models of case management have been developed over the past two decades and during this time they have become a cornerstone of community support services for persons with mental illness (Curtis, 1992; Hodge and Draine, 1993; Rapp, 1996; Soloman, 1992). "Case management" as a term has come under fire because of the negative connotations associated with being labelled a "case" that must be "managed." Alternative terms for persons providing this service include: personal service coordinator; service coordinator; community support worker; care manager, key worker, and so forth. The basic purpose of case management services is to assist an individual to access the services and supports he/she needs, when they are needed, for as long as needed. Service components typically include some or all of the following: client identification; outreach; service assessment; planning; monitoring; linking and referring to services; advocacy for needed services; direct provision of support to the client, their family members, and significant others in home, social, and work environments; assistance in developing personal support networks; crisis planning, prevention, and intervention; teaching and coaching of social and self-management skills. Different models of service provide these components to varying degrees. MODELS OF INTENSIVE CASE MANAGEMENT Four dominant "models" of case management have emerged during this time: the broker model, the strengths model, the P/ACT model (full support model), and the rehabilitation model. There are many similarities among the models and their respective applications in the field, and there are many permutations and hybrids of the models which combine various elements of the models. However, there are some distinctions which are summarized briefly below (Mueser et al., in press). "Intensity" in case management services is usually determined by the number of hours of service provided, the case load size and mix, the severity or complexity of the needs of the individuals served, the range and duration of services provided, and commonly a team-based organizational structure. With exception of the broker model, any of the approaches to case management may be more or less intensive. Dietzen and Bond (1993) found that for people with high service use patterns, intensity in case management services is not linearly related to client outcomes and that there are likely other demographic, clinical, and preference factors than intensity of service delivery which affect outcomes such as hospital utilization. However, their study clearly showed that low frequency of case management contact was not at all effective in reducing hospital use for these persons. •BROKER MODELMODEL -- The primary intervention available to the case manager is linkage and referral of a person to a set of service programs which are prescribed to meet the need of the individual. Broker case managers tend to carry high case loads and have limited interaction with the people they serve outside of basic assessment, planning, referral, and monitoring activities. Expanded broker model programs include more emphasis on assessment and planning, advocacy, and problem solving assistance. A fundamental limitation of this approach is that it expects case managers to connect people with needed clinical services, but not themselves to act as a clinician. This assumes that clinical skills are not needed to perform effective case management and that a provider can always be provided to supply the needed service. While still common, the broker model is somewhat out of favor and current research suggests that "not only does it fail to produce benefits for clients and to reduce hospitalization, but it may have iatrogenic effects" (Rapp, 1996). •REHABILITATION MODELMODEL -- Rehabilitation case management emphasizes the importance of providing case management based on individuals desires and goals, rather than goals defined by the mental health system. It is commonly known as the "choose-get-keep" model. This approach places strong emphasis on developing a rehabilitation diagnosis (as contrasted with a DSM IV psychiatric diagnosis) which is based on an assessment of an individuals skill functioning and environmental resources. Interventions focus on skill development and making adaptations in the individual's environment so that people can live, learn, work, and plan in environments of their choice. •ASSERTIVE COMMUNITY TREATMENT (P/ACT) OR THE FULL SUPPORT MODELCOMMUNITY TREATMENT (P/ACT) OR THE FULL SUPPORT MODELTREATMENT (P/ACT) OR THE FULL SUPPORT MODEL -- The Program in Assertive Community Treatment (PACT), also known as Training in Community Living (TCL) and Assertive Community Treatment (ACT), was designed in the 1970's to be a community based alternative to the psychiatric hospital for people with mental illnesses, and as such, it is the most researched case management model. It has subsequently developed as a specialized package of services designed for the special needs of people with most severe psychiatric difficulties -- usually characterized by a severe and long-term psychosis, co-occurring disorders (e.g. substance abuse), and a pattern of high utilization of services (Mueser et al., in press). P/ACT is delivered by a multidisciplinary team which includes a psychiatrist, a nurse, and at least two case managers. It is further characterized by: •Low case loads (about 1:10); •Case loads which are shared across clinicians rather than individual case loads; •Availability of services 24 hours per day, 7 days a week; •Most services needed by clients served by P/ACT are provided by the team rather then referring them to other providers (e.g. psychopharmacology and other clinical treatment, housing support, crisis intervention, vocational support, and so forth); •Services are predominately provided in the community as opposed to officebased; •Emphasis on practical supports of daily living; •No time limits for length of service (e.g. 18 months or 2 years). The P/ACT has been replicated and has mutated in programs around the world and applications of this model have been adapted to meet the needs of specific client populations, state or local agencies, urban/rural geographical settings and so forth. A common variants of P/ACT are known as Continuous Treatment Teams (CUT) and Intensive Case Management (ICM), both of which may provide elements of P/ACT such as team structured services, low case loads and mobile, flexible supports, but not provide others such as a shared case load or assignment of a psychiatrist to the team. There is considerable debate over exactly what constitutes "fidelity" to the P/ACT model (McGrew et al, 1994; McGrew and Bond, 1995). Teague, Drake and Bond (1995) developed the Dartmouth Assertive Community Treatment Fidelity Scale (Appendix V) to provide a method of assessing the components and range of fidelity to P/ACT. •STRENGTHS MODEL -- The strengths model (also known as the Kansas Model) was developed in response to concerns that other approaches to case management tended to emphasize pathology, limits, and impairments associated psychiatric disability at the expense of negating the personal strengths, resources, gifts, and abilities that an individual can draw upon for achieving personal goals. The model identifies a person's strengths and then actively creates situations (environmental and personal) where success can be achieved and the level or personal strength enhanced In addition, there is very strong emphasis on helping individuals to develop personal networks of support that are outside the formal mental health system -- an area de-emphasized in some of the other models. A high priority is placed on the quality of the relationship between the worker and the person served. The strengths model of intensive case management is grounded on six basic principles (Rapp, 1988): •The focus is on individual strengths, not on deficits or pathology. •The community is viewed as an oasis of resources, not as an obstacle or target for blame. •The helping process is guided by a rigorous standard of consumer selfdetermination. •The relationship between the consumer and case manager is primary and essential. •Community integration is fostered by intensive outreach. •Persons with severe and persistent mental illness possess the inherent capacity to learn, grow, and change. In many ways the strengths model is a philosophical and relational model rather than a structural model. It has been effectively merged, for example, with aspects of P/ACT such as multi-disciplinary staff, focus on high need individuals, provision of services that are not time limited, 24 hour/7 day per week availability, and so forth. The strengths model of case management is typically structured as a team service for case planning, problem-solving and sharing knowledge and support among team members. A mix of one or more team members may provide the direct services. There is emphasis placed on group rather than individual supervision of team members. However, unlike many P/ACT programs, the strengths model typically attends more carefully to the concepts of graduated disengagement of the client and to the replacement of professionally provides support services with alternative non-professional supports from within the community. COMPARISON OF THE MODELS Mueser at al (in press) provides the following analysis of the distinctions between these four models of case management. Features of different case management models Considerable research, training, and evaluation of these approaches has contributed knowledge about what elements of these various models are critical and essential to achieve the desired outcomes (Rapp, 1996; Muser et al., in press; Bond, McGrew and Fekete, 1995). Full support approaches such as P/ACT and some variants of the strengths model do consistently have lower hospital inpatient days with some studies also showing increased periods of community tenure between hospitalizations, and reduced number of admissions (Goering, in preparation). In studies comparing the models, outcome measures suggest that P/ACT and its subsequent adaptions have slightly elevated benefits over other models in terms of increased engagement in treatment, decreased attrition, and decreased hospital use. On other measures (e.g. housing stability, symptomatology, quality of life, family burden, vocational function, client satisfaction, socialization, and substance abuse) P/ACT outcomes were equivocal to other approaches. The strengths model provided similar outcomes to ACT, but also showed benefits in some areas where ACT had only mixed results (e.g. social functioning, behavioral symptomatology, client satisfaction and family burden). The rehabilitation model was found to be not effective for non- or less verbal clients (Rapp, 1996). Drake, Teague, and Warren (1990) are among a number of practioners and researchers who are adapting the P/ACT approach to persons with substance abuse disorders. In the New Hampshire Dual Diagnosis program, continuous treatment teams are identified along with stable housing and psychiatric hospital facilities as core treatment components in an integrated service program. He further suggests that treatment and support for persons with co-occurring disorders should occur within the mental health service system (as opposed to health or additions) since people with co-occurring disorders do not fit easily into more traditional programs. Consequently, mental health staff need to have a heightened awareness and expanded skills in order to effectively engage and treat persons with co-occurring disabilities. In all of these models, there is a trend toward including consumers as support workers (case managers, peer support specialists, case management aides, and for forth) on case management teams. The research studies that have been done to evaluate the impact of consumer staff on outcomes suggest clearly that consumer staff as members of teams had no negative impact on team outcomes and, in fact tended to result in enhanced quality of life outcomes for the people served (Felton et al, 1995; Soloman and Draine, 1995; Felton et al., 1995). BEST PRACTICES IN INTENSIVE CASE MANAGEMENT Based on these and other studies certain best practices can be identified as follows. Bond (1994) cautions however that practioners should dispel any single "best" model of case management, particularly for rural areas. "The issues of resource, geography, and culture defy simple formulations" (p. 341). •Intensive community focused case management for an extended period of time is effective in breaking the re-hospitalization cycle and has long lasting stabilizing effects. •Frequency of contact rather than hours of contact makes a difference. Telephone contact may supplement, but not substitute for face to face contact. •The quality of the contact, not just the frequency, along with the philosophical orientation of the case worker (e.g. strengths or recovery orientation) may also be mitigating factors in outcomes. •People who are at high risk for acute exacerbation of psychiatric symptoms or whose level of disability plans them at high risk for restrictive service settings should be served by low case load case management (optimally no more than 10-15 clients per case manager or team member). •Case managers should have the ultimate responsibility for client services (with the exception of prescription of medication). They retain authority even in referral situations. •Clients should be given equal or greater authority than case managers or other professionals in making treatment and life decisions. Community Support Services (including Supported Housing) DEFINITION OF COMMUNITY SUPPORT SERVICES Community support services can generically be defined as an entire array of treatment, living support, crisis prevention and management, and rehabilitation services needed to assist persons with severe, disabling mental illness to function at optimal levels within the community (Stroul, 1988). The lived experience of a mental illness often entails significant barriers to attaining and maintaining the basic elements of a "regular" life: decent housing, satisfying work, mutual caring and intimate relationships, and normal life roles. The barriers may include poverty, discrimination and stigma, disconnection with family and friends, interruptions in natural adult development due to the cyclic nature of the disorder, and sometimes cognitive difficulties. Community Support Services typically focus on practical day-to-day supports which help people to navigate or overcome these barriers and to develop the personal and environmental resources needed to maintain a satisfying life. Carling (1995) redefines community support as essentially the promotion of community integration all arenas of living: home, employment, spiritual, and social./recreational activities. In his approach, community support entails more than professional services focusing on maintain people in the community. "The basic belief of the community integration movement is that all people, including people with disability labels, have a right to full community participation and membership.... This goal will not be achieved primarily through professional services, but rather through peer support and self-help as well as through physical, vocational, and social integration into mainstream community activities, jobs, housing, and relationships with non-disabled persons....[This is not an assertion that] professional services are unimportant, but that to be effective, such services must be controlled by their users" (p. 21-22). What is community support? Whatever it takes to help people lead rich and fulfilling lives as citizens of their communities. As noted earlier, case management programs (particularly full support and intensive case management) are often very involved in providing community supports and services. However, there are also other models of community support service delivery. For example, the support can be provided by supported housing (or vocational) specialists, peer support workers, family and other carers, volunteers, community friendship and mutual aid networks, or mobile rehabilitation workers. Philosophically, these programs draw from the skill building focus of rehabilitation programs, from the strengths and community resource focus of strengths-oriented case management programs, and from the empowerment, self-advocacy, and mutual aid elements of self-help programs. SUPPORTED HOUSING Supported housing (supported accommodation) services typically emphasize personal choice and self-determination, use of regular generic community housing (as opposed to congregate facilities), and the delivery of individualized and flexible supports. Specifically support workers help people to make determinations about housing preferences, to locate and choose suitable housing and to develop personal support plans which relates specifically to needs associated with that living environment (What is it going to take to "make it" here?). Supported housing assistance may include: •Concrete and emotional support during and following the move into housing; •Attention to special needs (such as those of single mothers); •Support and skill training/coaching in an individual's home or community to help individuals meet the day-to-day demands of life in the community (laundry; meals; neighbour, friend and family relations; home maintenance; self care; symptom self-management; finances; and so forth); •Assistance with developing personal rhythms and structure which "fit" the individual, •Assistance with self-medication maintenance; •Support for self-advocacy in negotiations with landlords and other community representatives; •Help in problem solving and decision-making; •Mediation of disputes; •Support for application of recovery skills when, where, and as needed •Crisis prevention and planning; •Other aspects of informal supportive counselling. Supported housing services are not tied to any particular setting, but move with the individual as he/she moves to other living arrangements. While it is anticipated that individuals may require in home support for an ongoing period -either in continuous or episodic fashion -- a challenge to many housing support providers is to maintain an intention-full and rehabilitation/recovery oriented focus so that the tenant's need for professional support will diminish over time. A range of different housing alternatives is available, but there is emphasis on helping people to access commercially available housing in local neighborhoods that is safe, decent and affordable. In communities where there is an insufficient supply of this kind of housing, the agency or program takes a lead in developing partnerships with housing organizations to improve availability of integrated housing to people with psychiatric disabilities. Wherever possible, the consumer holds and is responsible to the lease to the housing, rather than a service agency. Appendix VI provides a compilation of best practices in housing and supports for people with psychiatric disabilities which was developed as part of a technical assistance tool kit on housing for persons with psychiatric disabilities (Hutchings, Emery, and Aronson, 1996). WORK AND EDUCATION SUPPORT A person discharged from a psychiatric hospital has a greater chance of returning to the hospital than of returning to work. We have not been very successful at teaching the skills that will help people be workers, but we have been very successful at teaching people how to be clients! Unfortunately, the skills of the worker are very different from the skills of the client Anthony, 1994 WORK PREPARATION, TRAINING, AND SUPPORT APPROACHES Work is a source of income, productivity, relationships, structure and meaning in one's day, and valorization of the normal adult role as worker. In spite of the many benefits that can accrue from work, mental health service systems have traditionally been hesitant to promote work as a valued component of rehabilitation programs. The Centre for Psychiatric Rehabilitation at Boston University reports that, in the United States, only about 10 - 15 percent of the people with a serious mental illness are working full or part time (Anthony, 1994). The impact of high and sustained unemployment can lead to increased poverty, despair, isolation, perpetuation of helplessness and the personal sense of having nothing of value to offer (Marrone, et al., in press).. There are a number of reasons for high unemployment of persons with psychiatric disabilities which include the following points (Anthony, 1994; Goering, in preparation; Marrone, in press). •Stigma and discrimination from both the community and the mental health service system; •Assumptions that psychiatric symptomatology predicts capacity to work: •People with psychiatric disabilities do not want to work •A mental health service structure which emphasizes not work, but work preparation and moving through a progression of steps to build "readiness" for work •Very real concerns that work will negatively affect one's disability benefits which include medical insurance and some measure of financial security. This is changing, though more slowly than would be desired. The complex relationship between work and disability benefits is under scrutiny in many areas, particularly in the United States. But as importantly, many consumers report that finding satisfactory work or areas for achievement is essential for well being (Campbell and Schraiber, 1989; Sullivan, 1994; Copeland; 1994). There are increasing numbers of programs which are designed to help individuals move more quickly into real jobs and to provide flexible, on-going supports to help individuals to retain their jobs (and to develop careers!). The National Association of State Mental Health Program Directors (NASMHPD) published a position statement on employment of persons with psychiatric disabilities (Appendix VII). In 1992, the National Institute on Disability and Rehabilitation Research (NIDRR) of the United States convened a Consensus Validation Conference on "Strategies to Secure and Maintain Employment for Persons with Long Term Mental Illness." The Conference identified the following service models of employment programs in public and private settings. These models may also include services such as skills assessment, career planning, and employment preparation components (Viccora, Perry and Mancuso, 1994). •TRANSITIONAL EMPLOYMENT PROGRAMS (TEP) -- Commonly associated with Clubhouse models of rehabilitation, this approach involves entry level positions in community settings split into part time positions to be shared by one or more consumers. Typically short-term (about 6 months) rather than permanent. When one consumer has completed the placement, another is cycled into it. Seen as a first step toward competitive, integrated employment. •INDUSTRIAL ENCLAVES -- Established within larger commercial business, enclaves are whole units (mail room, loading dock, janitorial service) taken over by an agency and staffed by consumers. •WORK CREWS -- Many rehabilitation programs have established mobile janitorial, landscaping, painting, clean-up, or catering crews which are staffed entirely by rehabilitation clients and supervised by program staff. Services are sold to community businesses and public agencies. •WORKSHOPS -- Work sites within rehabilitation programs which may sell a set of services on a contract basis to community businesses. Services sold may include office support (envelope stuffing, packaging document shredding), data management (data entry) and so forth. Focus is typically on work adjustment and basic skill development. •SMALL BUSINESSES or COOPERATIVES -- Agencies may establish small businesses to provide consumers with full or part time work opportunities. These business may spin off into completely consumer operated businesses or retain affiliation with the parent mental health agency. The businesses may be located at various sites in the community or be co-located in a sheltered setting. Examples of businesses may include: organic truck gardens, picture framing, restaurants, bookstores, ice cream franchises, janitorial services, thrift shops, production wood shops, prescription optical services, various cottage industries, and so forth. A variant of this model is the Fairweather Lodge in which small groups of consumers both live together in shared accommodation and operate a small business together which benefits the whole unit. While there may be justifiable argument that many of these businesses do not exemplify the principle of integrated employment settings and can become "dead ends" for workers, they can also play a significant role in establishing real work opportunities for people and in enhancing income. •SUPPORTED EMPLOYMENT -- Focuses on assisting clients to get and keep work as regular employees integrated community agencies and businesses. Characterized as a "place and train" approach. Individuals receive flexible and on-going support on-site and/or off-site tailored to the needs of the individual and the job setting. Support may include on-the-job training, on-going monitoring and trouble shooting as well as off-site mentoring, coaching, and career planning. There is increasing use of mental health agencies as supported employment sites for consumer interested in human service work.. •CONSUMER RUN PROGRAMS -- Consumer-run employment programs are emerging which offer peer support, vocational counselling, education and training, and placement services. Similarly, there are increasing numbers of consumer-operated businesses and services which offer employment to other consumers (Allen and Granger, 1997). One of the most striking developments is an increase in consumer-run mental health services which may include wellness and drop-in centres, case management and advocacy services, crisis respite and hostels, accommodation support services, and so forth (Mowbray and Moxley, 1997). VOCATIONAL OUTCOMES Recent efficacy and effectiveness studies of vocational rehabilitation programs for people with psychiatric disabilities indicate that vocational interventions are effective and have been moderately to strongly successful in helping individuals to find and maintain paid jobs. (Cook and Jonikas, 1996; Bond, 1992). This is not true of sheltered workshop programs however, which have been found to be not effective in helping individuals transition to competitive jobs in the community (Goering, in preparation). Bond et al. (1996) further found that supported employment programs were more effective than other forms of vocational rehabilitation in helping individuals to get and keep competitive work outside agency work programs, and to maintain higher wages. Success in community employment continues as long as the individuals continue to receive tailored supports. The studies also found that attending to consumer preferences for work type, style, location, leads to greatly improved job satisfaction and tenure (Bond et al., 1996; Becker et al., 1996; Viccora, Perry and Mancuso, 1994; Matrix Institute, 1997). BEST PRACTICE PRINCIPLES IN EMPLOYMENT SERVICES The 1992 NIDRR Consensus Validation Conference identified the following list of principles for best practices in employment services (Viccora, Perry and Mancuso, 1994). •Consumer choice. Successful programs both value and act on consumer choice, promote and support consumer empowerment by providing people with control over the timing, pace, and intensity of their engagement in vocational rehabilitation, as well as a wide range of choices in work settings and type. Futures planning and career planning help identify personal preferences and directions. •Integrated settings. Real work opportunities should be in as integrated an environment as possible in which workers have maximal opportunities to interact with a variety of co-workers, supervisors, and the general public. •Service linkages. Rehabilitation agencies can promote successful work outcomes by attending not only to work-oriented programs, but to a range of nonwork resources as well -- accommodations, financial assistance, social opportunities and so forth -- that an individual may require for successful employment. •Natural supports. Many programs are drawing on "natural supports" in the consumers life to provide the worker with supports needed to remain employed. Examples of natural supports include: family and carers, friends, co-workers, mentors company employee assistance programs, and so forth. •Rapid placement. Effective programs help people find real jobs in the community quickly, minimizing pre-placement preparation. Use of careful person-site matches, on-the-job-training, and of-the-job support are needed and desired by consumers. •Job accommodations. Job accommodations are adjustments made in the job scope, schedule, setting, structure, or policies which enable a person with disabilities to successfully maintain that job. Job accommodations be provided by the employer or the rehabilitation program and are highly individualized (Granger, Baron and Robinson, 1996). •Continuity of services. "Seamless" services which do not require an individual change counsellor, agency affiliations, or relationships as the person changes are desirable. •Proactive orientation. Rehabilitation programs work proactively encouraging people to view work as an important aspect of their present and future lifestyle. Implementation of futures planning technology to help stimulate hope, a positive vision of the future, and a supportive personal network (Joyce, 1996; Mount, 1990; Lavin and Everett, 1995). In many vocational programs there is an expectation that a worker must be "ready" to move to the next stage of rehabilitation (e.g. training, placement, etc). Frequently people with complex needs are labelled "not job ready." This readiness model has negative ramifications for a person with a psychiatric disability (Marrone, in press). The Institute for Community Inclusion (1995) suggests that: •One cannot reliably predict who will be successful in employment; •Community settings can accommodate a wide range of skills and behaviours; " •People with disabilities do not always generalize skills and behaviours from one setting to another; •Some problem behaviours and skills deficits cannot be improved in segregation. •Real work situations can only be simulated to a limited extent. What appears to be more important that "readiness" is "fit" or creative job matching. Creative job matching entails creating a match among the skills, interests, values, and needs of a person with the demands of a specific job and the values and needs of a particular employer. Paid work is not the only valued activity which provides structure and meaning for people with disabilities. There is increasing attention to helping individuals find ways in which their skills and abilities can contribute in a valued way to a community. This may involve on-going or short-term volunteer work in areas of interest, participation in governance or advisory boards and committees, opportunities for social action, educating others formally or informally through public speaking, presenting about personal experiences to community members and students, mentoring or helping others, and so forth. While these activities usually to not have the economic benefit that are associated with work, they need to be recognized and supported as important elements of recovery for many individuals. EDUCATION SUPPORTS In the past decade, supported education programs have emerged to in response to some of the problems experienced by people in more traditional rehabilitation programs and because of the expressed desires by consumers and family members to pursue advanced education goals (Unger, 1993). As with supported employment and supported housing, supported education takes a rehabilitation approach to helping individuals pursue educational goals. This may entail attaining high school equivalency, beginning or returning to college or other generic technology training program. This model is also seen as a promising avenue to increasing employment rates of people with psychiatric disabilities (Anthony, 1994). The participants of supported education programs tend to differ from other groups of people with severe mental illness in that they are younger, more educated, and less severely symptomatic (Mowbray, Bybee, and Shriner, 1996). Although most of the literature on supported education currently focuses on college settings, there are examples of rehabilitation programs who have collaborated with local boards of education to develop continuing education programs for people with psychiatric disabilities and to provide high school equivalency degree study opportunities within the rehabilitation program. There are also examples of mental health consumers working as supported education mentors which benefits the student and provides employment and gratification for the mentor (Sharac, Yoder and Sullivan, 1997) Supported education may include any or all of the following components (Unger, 1992). •Assistance with education program planning, selection, application, and preparation; •Specialized orientation and pre-college assessment and support planning; •Individualized study programs or special topic courses; •Help with registration and financial aid; •Structured classrooms; •Special matching of housing options and roommates •On-going mentorship and peer support; •Development of accommodation plans and assistance with negotiating accommodations; •Personalized support such as in-class assistance or follow-up debriefing; •Tutoring and remedial skill development in academic and study skills, as well as in time management, communication and social arenas. •Assistance with relapse prevention and crisis management. A five-to-eight year outcome study of the initial project launched at Boston University finds that program participants were able to maintain initial gains identified in employment status, self-esteem, and reduction in hospitalization rates. Participants reported moderate satisfaction with their overall quality of life (Danly, in press). The study results suggest that programs which serve young adults with psychiatric disabilities should consider providing career education assistance to improve the long-term possibility of vocational achievement and personal success. Family Education and Support Families and carers play an important role in the rehabilitation and recovery process of persons with long term mental illness. Historically, considerable research has focused on how family communication styles, interpersonal relationships, and expressed emotion directly "cause" or in some fashion negatively impact on mental illness (Goldstein and Rodnick, 1975). While there has been no support that these factors can "cause" mental illness, there is some acknowledgment that families do have an impact on their family members with mental illness -- as families everywhere impact on their family members. Family relationships are emerging as an important component in recovery (Falloon, et al, 1982; Hyde and Goldman, 1993). The role of family in any individual's life is often culturally determined with some cultures and communities placing more or less emphasis on the importance of an individual separating from the family and "make it on their own." Beyond cultural norms, some families are the primary source of support for their family member with mental illness. Individuals may live with their parents or adult siblings, receive emotional, financial and material assistance from them, and rely on their family for their day-to-day support. Hatfield (1988) states "sometimes families serve in lieu of the professional practioners and the family itself serves as the agent of rehabilitation." Many families themselves are striving to provide needed resources and support and to remedy social deficits. Hatfield also reports that the National Alliance of Mental Ill (AMI) in the United States has found that 60% of the families of persons with mental illness are operating as primary care takers with little respite or professional guidance or support. Family/Carer "Burden" is increasingly identified as an outcome measure and one of the social costs of psychiatric rehabilitation and other mental health services (Wolf, Helminiak, Diamond, 1995). FAMILIES AND REHABILITATION PROVIDERS The provision of education, information and support to family members by mental health professions is increasingly important to consumers, families and rehabilitation workers alike Hanson and Rapp, 1992). While not all families bear the full burden of supporting a member with mental illness, there are few families who are not deeply affected by their family member with serious mental illness -whether that member is closely connected to the family or living more "independently" in other circumstances. While it is clear that the primary role of rehabilitation services is to focus on the needs of the individual consumer, there is also evidence that people do better when their families are knowledgeable about the mental illness, know the resources available, and skilled in ways to support or cope with the individual when needed, and willing to engage in collaborative discussion and planning (Vosler-Hunter, 1990). It is also easier for consumers to navigate or improve relationships with their families when the family is informed and feels supported. Discussions with families of persons with a serious mental illness shows that, in general, families want education, information, and support (Ryglewicz, 1985; Yess, 1988). Specifically, families want: •Professionals to understand and validate their experiences of living with or loving a persons with serious mental illness; •Accurate and timely information about mental illness to that they can understand the experience of their family member; •To understand the service system and how it operates so that they can manoeuvre with in it (and around it); •Concrete and practical advice about strategies for coping with the illness and its impact on their personal and family life; •To know the resources (material, treatment, financial, social, and so forth) available through multiple sources which might assist their family member •To be actively involved as a partner in designing and delivering services for their family member -- particularly when those services directly impinge on the family (e.g. when the individual with mental illness lives at home with a parent or adult sibling as a care-taker): •To participate fully in the design and evaluation of mental health services. Some rehabilitation services are actively integrating family education and support into both their array of services and into their style of delivering services in general. A Model Policy on Family Involvement is included in Appendix VII and evidence of the application of these principles can be found in a number of the Program descriptions included in this paper. FAMILY-TO-FAMILY EDUCATION AND SUPPORT Mueser and Gingerich (1994) have published a comprehensive guide to living with a mental illness designed primarily for family members, but useful to consumers and rehabilitation practitioners as well. It provides information about mental illnesses and the service system, tools for identifying and managing environmental stressors, communication and problem solving approaches, improving family life, and ways to navigate shared household living. As importantly, there has been a surge in family-to-family education and support activities which operate in conjunction with and independently of the formal mental health system (Burland, 1995; Hatfield and Lefley, 1993). Providing funding and support to these initiatives is important to help ensure the long-term viability of a critical assist in the rehabilitation and recovery support system (Goering, in preparation). VI. Program Examples Innovation starts with an idea. What happens to the idea once it is exposed to scrutiny is greatly influenced by the environment surrounding it. If an idea is congruent with the traditions, philosophy, and practice of the environment, it will be nurtured....if on the other hand the idea is contrary to or inconsistent with the traditions of its environment, its rate of growth is slower and its chances of growing strong are reduced. Stein and Test (cited in Weisburg, 1993) This section contains descriptions of a number of programs which exemplify the best practices described above. Some of the programs focus primarily on one or two of the practices, others are broadly inclusive of current and emerging best practices in mental health services. The programs are presented in alphabetical order and are as follows: Canadian Mental Health Association (CMHA) Canadian Mental Health Association, Timmins, Ontario, Branch Hamilton Program for Schizophrenia, Hamilton, Ontario Journey of Hope, NAMI, United States Northeast Independent Living Centre, Lawrence, Massachusetts Stepping Stone Peer Support Centre, Claremont and Lebanon, New Hampshire Trieste, Italy Village Integrated Service Agency, Long Beach, California Canadian Mental Health Association (CMHA) The Canadian Mental Health Association (CMHA) Ontario Division provides the following description of its organization. The Canadian Mental Health Association (CMHA) was founded in 1918 and is one of the oldest voluntary organizations in Canada and the only one to deal with all aspects of mental health and mental illness. It is a national association with approximately 135 branches in communities of all sizes in all provinces and territories, and a division office in each province and territory. A major aim of the CMHA is to advocate improvements in mental health services and to press for changes in social policies that have an impact on individual's mental health. CMHA's grassroots programs help to ensure that people whose mental health is endangered will find the help they need to cope with crises, regain confidence, and return to community, family, and job. CMHA combats mental health problems and emotional disorders through research and information services, sponsored research projects, and workshops, seminars, pamphlets, newsletters, and resource centres. Further, it acts as a social advocate to encourage public action and commitments to strengthen community mental health services, legislation, and policies affecting services. Branches and Divisions are accountable to their own boards of directors, although there are some common standards to which all members of the Association adhere. Branches and divisions have their own (diverse) funding sources. The National Office receives allocations from the Provincial Divisions according to a negotiated formula (Pape, 1997). The central organizing set of standards of the CMHA are outlined in the publication, A New Framework for Support for People With Serious Mental Health Problems (Trainor, Pomery & Pape, 1993). Briefly, these standards are organized into two fundamental percepts with attendant objectives. 1) Develop comprehensive services and supports using the Community Resource Base as a conceptual model. 2) Develop a new understanding of mental illness using the Knowledge Resource Base as a conceptual model. Community Resource Base This schema illustrates that formal services are only one of the important influences that affect the lives of people with mental illness. It manifests a shifting view of mental health services from a "service paradigm" to a "community process paradigm" and highlights the need for partnership across all sectors. To strengthen the community resource base, the following standards are suggested. •Identify new ways of allocating financial resources for mental health. •Identify new ways of distributing power and influence within the mental health system. •Develop and support consumer groups and organizations. •Develop and support family groups and organizations. •Fully involve consumers and families in service design and delivery. •Reinvest institutional dollars in coordinated and effective community services. •Develop services which build access to the basic elements of citizenship such as work, housing, education, and income. •Make generic community services and supports, such as social assistance and public housing, accessible and a part of coordinated service delivery. Knowledge Resource Base Fundamentally, it is our most basic assumptions about the nature of mental illness that defines how we act. The Knowledge Resource Base is made up of the various types of knowledge that people have about mental illness, including medical/clinical (knowledge developed by professional mental health disciplines); social science (social factors such as poverty, homelessness and so forth); experiential (knowledge that comes from "living with it."); and customary/traditional (informal information from family, friends, community, and culture). Standards deriving from this model include: •Develop and document experiential and customary/traditional knowledge •Develop a sustained and conducive dialogue among all the players. Canadian Mental Health Association - Timmins, Ontario, Branch Timmins is a small town in high-rural northern Ontario with a branch of the CMHA located there. The mission of the Timmins Branch of the CMHA is to provide support to people who have been diagnosed with serious mental illness. The program has undergone recent changes and a current program description provinces the following details (Augello, 1997). The Branch offers its members the following services. A more complete description can be found in Appendix IX. •Case management; •Residential program (supported and supervised housing in partnership with the Timmins Housing Authority) •Social/recreational program, with daily activities •Community support program which provides mobile off-site individual support •One-to-one volunteer program •Self-help/education program •A new 24 hour/7 day per week crisis intervention component (in partnership with the Cochrane District Health Council, Timmins and district Hospital, Kap Counselling Centre and Minto Counselling). Program staff work as part of a mental health team with each staff working an eight week rotation in different roles within the different programs. Each staff acquires specialist skills necessary to act as part of the team with specializations including: supportive employment, life skills, mental health education, medications, self-help, and so forth. Services are available in both English and French. Hamilton Program for Schizophrenia, Hamilton, Ontario Hamilton Program for Schizophrenia (HPS), located in Hamilton, Ontario, is a mature community-based psychosocial rehabilitation and treatment program which integrates all best practices identified above. It uses a long-term, intensive case management model which structurally resembles the P/ACT approach, but utilizes individual case loads and the strengths-based, community-oriented focus of Strengths Based case management approach. All case managers are also trained in psychiatric rehabilitation and integrate therapeutic elements of this approach (e.g. goal setting and direct skills teaching) into their practice. One characteristic which distinguishes the HPS is it strong emphasis the program places on involvement of families in the rehabilitation process. Family members are actively encouraged to participate in the program and are incorporated into the treatment team whenever possible. Case management services are provided directly to family members as well as the family member with mental illness -even though the majority of agency clients individuals do not live with their families. When a client joins HPS, his/her family is asked whether they would like to talk with an experienced HPS family to learn more about HPS and to share coping strategies. The program operates a family support program HPS Family Association and all family members of HPS members are invited to join. The Association meets regularly for information sharing and mutual support. The program has identified meeting family needs and family satisfaction as cores element in its program evaluation design. HPS has devised a Family Satisfaction Questionnaire which inquires about general satisfaction as well as satisfaction with specific services such as case management to themselves and their family member. Family burden is assessed using objective measures such as monthly expenditures of time and money by families for their relative with mental illness (Whelton, Pawlick and Cardamone, FIND CITE). Journey of Hope - National Alliance for the Mentally Ill, United States The Journey of Hope is less of a "program" per se, and more of an educational resource often conjointly offered between a mental health service agency and a family advocacy and support group. It provides a good example of how rehabilitation programs can partner with family support groups to provide much needed family education and support services in their communities. Originally designed by the Vermont Alliance for the Mentally Ill (AMI) in 1991, this program is a family-to-family teaching model where AMI member volunteers are trained to work in co-leader pairs to conduct a rigorous 12-week course. The program was launched as a self-help vehicle for family members and carers of people with serious mental illness and uses as trauma model of recovery as its touchstone. It embraces the belief in the inherent strength of families and the importance that empowerment models have in "raising consciousness" by helping people validate their lived experience, by giving them pertinent information to combat the stigma they face as family members of a person with a serious mental illness (Burland, 1995). The program has mushroomed in the past several years and is offered in many areas in the united States and Canada and has been sponsored by various mental health funders and agencies. In 1995, over 800 persons were certified as trainers. More recently some variations of this model are being seen whereby a consumer or professional mental health worker pair with a trained family member to provide the program. Similarly, the program is being used for more than familyto-family education, primarily to educate and sensitize mental health staff to family perspectives and concerns. The Journey of Hope Ten Principles of Support 1. We acknowledge and accept the fact that someone we love has a mental illness. 2. We accept that we have no control over this illness or the individual with the illness. We have control only over our own actions and thoughts. 3. We release all feeling of guilt concerning this mental illness for we are not to blame for the illness or its effects. 4. We understand and acknowledge that the mental illness has had an impact on all of our relationships. 5. We forgive ourselves for the mistakes we have made and we forgive others for wrongs we feel have been committed against us. 6. We choose to be happy and healthy. We choose to return to a healthy focus on ourselves. 7. We keep our expectations for ourselves and for our mentally ill loved one at realistic levels. 8. We believe that we have inner resources which will help us with our own growth and will sustain us through crisis. 9. We acknowledge the strength and value of this support system and we commit ourselves to sustaining it for our benefit and the benefit of other families. 10. We acknowledge that there is a higher power to whom we will turn to nurture and strengthen our ability to release those things we cannot control. Northeast Independent Living Program, Lawrence, Massachusetts The Independent Living movement was spawned by people with physical disabilities as three things: •A national grass roots movement for social justice and civil rights made up of people with disabilities; •A "lived" philosophy developed by people with disabilities struggling to regain control over their lives and the resources that affected their lives; •A national network of support, service and advocacy non-profit centers that are primarily controlled by and staffed by people with disabilities. Although initiated by people with physical disabilities, these centers have evolved to be more "cross-disability" over time and now involve individuals with other disabilities, including those with psychiatric disabilities (Deegan, 1992). The Northeast Independent Living Program (NILP) is one such center. Located in Lawrence, Massachusetts, the NILP was formed in the late 1980's as a center primarily for people with psychiatric disabilities. Not wanting to fall into the trap of forcing people with psychiatric disabilities to fit into the services that were designed by people with physical disabilities, the NILP began as a grass roots organizing effort. A grass-roots community organizer and organizing trainee were hired to provide technical assistance to the NILP and other forming member-controlled groups. A model of completely consumer-run conferences was developed and a series of conferences were sponsored both in the community and in the psychiatric hospitals. These conferences served as tools for developing leadership within the community of people with psychiatric disabilities, for conducting outreach, and for providing a forum for expression, consciousness raising, and role modeling. The hallmarks of the "lived" philosophy of the Independent Living Center movement are identified by DeJong (1979, as cited in Deegan, 1992) are put into action at the NILP: •The problem does not exist in an individual, but exists as barriers in the environment; •People have the right to failure and the dignity of risk; •Consumers must be sovereign and have a major voice in the development of programs they use; •People can become experts in their own self-care and learn to de-medicalize their lives; •Self-help can offer people many things that professional help cannot. As consumers begin to actively define their needs as individuals and as an aggregate, the services of the NILP began to slowly take shape. The NILP did not attempt to rush the development of specific services, nor to become a parallel service delivery system, nor to duplicate existing services. Their services grow out of their emerging sense of what they need in order to regain control over their own lives. These services currently include the following (NILP, undated) : •Lawrence Organizing Voices for Empowerment (LOVE) -- a political action group advocating for change in the mental health system. Examples of the group's activities in May, 1997, included developing Mental Health Consumer/Doctor Guidelines to improve doctor/consumer communications; organized advocacy to support the Massachusetts Mental Health Bill of Rights; technical assistance to the local psychiatric hospital Patient Advisory Committee and to the regional department of mental health's Consumer Advisory Committee; participation with the regional mental health department task force rewriting policies on treatment; attendance at statewide Human Rights Conference.. •Haverhill "Warm Line" peer counselling -- a telephone support network which provides non-crisis support around daily living issues. Counsellor training program is offered for peer counsellor volunteers. •Advocacy for Inpatients -- technical assistance and support to hospitalized patients. Peer counselling and support are offered to people wanting help in how to work with a treatment team and to get what they want and need. •Information and referral -- assistance pertaining to legal, financial, housing and other issues via telephone and face to face contact. •Information exchanges and skills development in self-care, medications and their side effects, and skill building in self-advocacy and how to "work the system," working assertively with psychiatrists and others, how to write a kind of "psychiatric living will" or "health care proxy" (known in the United States as an "advance directive") in which the individual specifies treatment preferences and desired services, supporters, and decision makers should he/she be deemed incompetent to make such personal decisions. •Disability Awareness Training and Technical Assistance -- on-going peer-run skills training and technical assistance to organizations and individuals. •Personal Assistance -- collaboration with a non-profit organization offering inhome support to individuals who, because of their disability, require help with activities of daily living. •Consumer Run And Controlled Conference -- a yearly conference offering opportunities for networking, education, and information sharing. Services are offered free to any consumer/survivor/ex-patient of the mental health system who is over 18 years old.. Stepping Stone Peer Support Centre, Claremont and Lebanon, New Hampshire Stepping Stone Peer Support Centre is a fully consumer operated and member controlled wellness centre which opened in July, 1995 in Claremont, New Hampshire (a small town in a rural area) with a core membership of about 12 persons. In June, 1997, it had a membership of about 200 persons and had established a second drop-in site in another town. The program is an independent non-profit agency which holds a contract with the New Hampshire Department of Mental Health to provide peer support services, and as such, is accountable to the Department for fiscal management and service outcomes (Mead, 1997). The agency is committed to a non-hierarchical, supportive, educational and safe environment for people with emotional/mental challenges, and to the belief that people can and do recover from psychiatric disorders. All decisions, rules, policy, and direction are created by the community and responsibility for all aspects of the Centre is shared equally by all members. The Stepping Stone offers groups and events that emphasize shared leadership, skill development, team activities, holistic models of health. The philosophy of the program is that people who have experiential knowledge about mental health and illness can offer to each other support that differs from traditional mental health services. As people become more and more focused on their abilities, and find themselves supported by their peers through their difficulties, a sense of hope and of personal and relational responsibility develops. The goal is not to pursue life within the framework of disability, but rather to work toward dreams, build reciprocal relationships, and create together a community in which people have a variety of valued and changing roles. The goal is "life beyond disability." (Stepping Stone, undated) One of the primary goals of the Stepping Stone is to support diversity within its the community rather than to fight differences. In this way all members can become an integral part of a model of wellness that promotes self-help, recovery, education, and full participation in the Stepping Stone community as well as larger social environment Stepping Stone is open six days a week and is staffed by a full time consumer director and two part time assistant coordinators who assist with day-to-day operations and programming. Individual are referred to the program by word-ofmouth, as well as by the local mental health agency and psychiatric hospitals. All policy and operations decisions are made by the membership. Management of disruptive members is also handled by membership meetings. The services offered are determined by the membership and members can attend any or all of the activities depending on interest. Currently, components of the program are: IN-HOUSE: •Drop In -- community living room with television, videos, chat and social times. •Peer support groups -- regular support groups run by trained consumer facilitators. •Educational programs on topics relating to self-advocacy, empowerment, and recovery offered by members and invited speakers. For example, a naturopathic doctor presents a monthly information forum and demonstration on how to prepare nutritious meals on a disability budget. •Group activities which may be either education or support focused: A women's group recently raised money to take itself on a retreat; An eco-psychology group took itself on a camping trip to re-connect itself with the environment, adventure, and the spiritual side of nature. Other group activities have included music group, drumming group, group T'ai Chi and mediation practice; a science fiction group; empowerment group, and so forth. •Social Activities -- include art expression (community murals), softball, jewelry making, game day, music appreciation, and so forth. There is a weekly pot-luck dinner, cooking classes with the naturopathic doctor, picnics and barbies. •Recovery and wellness program -- members trained in recovery skills teach and support other members practice recovery skills. Activities include information sessions, personal assistance with crisis planning and symptom tracking, and management strategies. •Program management -- opportunities for day-to-day decision making and problem solving, dispute resolution, program planning, grant writing, grant renewal applications, computer skills development, program evaluation and research activities, and so forth. •Warm line to take non-crisis calls. Operates during the times the program is open. Open to all persons in the local community, not just Stepping Stone members. •One-to-one peer counselling. •Peer counselling training program. Training entails about 12 1-hour training sessions. Once a person is trained they may work on the warm line, facilitate peer support meetings, and so forth. •Collaborative teaming with traditional mental health agency to provide crisis prevention and hospital diversion support. EXTERNAL ACTIVITIES •Fund raising through various means. •Community education through presentations of mental health information to variety of audiences, including classroom students, mental health agency staff, community members, service funders, and so forth. •Advocacy and political action on a variety of concerns related to mental health and mental illness. •Consideration is being given to establishing a consumer-run book store. Recently the Stepping Stone was awarded additional funding to establish a consumer-operated crisis respite program which will be offered to Stepping Stone members and others who have completed a pre-service interview (Mead, 1995). This is the first fully consumer operated crisis program in the New Hampshire and one of the few in the United States. An intensive training program is being developed for persons interested in working in the respite program which is expected to open in September, 1997. Trieste, Italy Up until 1964, the census at Italian mental hospitals continued a slow increase and only during the next few years was there a gradual decrease in residents in the hospitals. Lead by Dr. Franco Basaglia a new progressive group called Democratic Psychiatrists organized and called for more community services and decreases in hospital census. Dr. Basaglia became responsible for the mental health services in Trieste. He successfully closed the institution in the city and began community services for the former residents. Many staff trained in Trieste and then moved to other part of the country to establish similar services. The national government with the example of Trieste, passed Law 180 in 1978. The law was a radical departure in Italy contained several significant provisions with the intent of closing all psychiatric institutions.. The significant provision of the law were: •Within one year of passage no new admissions were allowed in institutional beds; •the end of 1981 no readmissions were allowed; •New institutional facilities were not allowed to be built; •All psychiatric wards would be located in general hospitals and could not be larger than 15 beds. The wards had to be integrated with community mental health centres The ambitiousness of the law was offset by the lack of overall authority within the country. The national government does not have the usual power vested in many countries and relies to some degree on the city state tradition. This has meant that mental health centres were operated within regional and provincial governments. The result is that there is not a consistency regarding how the law was implemented and some areas did not follow the law or its intent. The northern regions, lead by the followers of Dr. Basaglia, have attempted to close the hospitals as he had done in Trieste. Many areas in northern Italian used the Trieste experience and developed their own unique models of care. Trieste is a city of about 350,000 that is on the northern Adriatic border, next to Slovene. It is an urban environment with a mix of cultures, the area having been ruled by a variety of nations prior to the end of WWII. The city has divided its services with many mental health centres and has successful closed its institution more than 15 years ago. From a census over 1,000 it now relies on several small 15 bed acute units within general hospitals. There is one small private unit that is connected to the university. The services within Trieste rely on several principles: •The creation of Community Mental Health Services for every 40-50,000 residents. •Strong emphasis on consumer and family involvement. •Emphasis on small acute units of 15 beds in general hospitals with short lengths of stay, less than 10 days. •Active outreach crisis teams that focus on in home crisis intervention. •Strong family supports and community linkages for users of services. •A wide variety of residential options to divert usage from inpatient hospitals. •Strong psycho social philosophy. •High usage of work cooperatives. The Trieste mental health centres rely on psychiatric leadership although they have organized the centres around interdisciplinary teams. The teams offer a variety of supports to the users. They work under a psycho social set of principles with emphasis on vocational and housing. The system relies on strong crisis in home intervention with at least two staff who work with the users during the crisis. This service is seen by many as a family intervention. The mental health centres have several day programs and in some cases have their own crisis beds within their facilities. One of the unique aspects of the Italian system is the usage of Worker Cooperatives. The cooperatives are linked with the mental health centres and have a variety of levels of independence from the centres. The cooperatives can be broken into two major categories although there is overlap. •Cooperative that are commercial in nature; •Cooperative that provide services to other users. These commercial cooperatives provide a variety or services such as cleaning, and farming to operating coffee bars, restaurants and hair saloons. The number of workers in these cooperatives in Trieste exceed 500. Many cooperatives in other parts of the country also provide services, such as case management and residential care. All of the cooperatives work closely with the mental health centres and other social welfare benefit systems. The Italian model is able to blend both social and health dollars which does offer some flexibility in the supports the users are able to obtain. The system also relies effectively on the sense of community in that often teams cover a specific territory within the centre, thus knowing sections of the city and the people in the various neighbourhoods. The results are the following: •Very low usage of compulsory interventions; •Few users diverted to forensic services; •Large numbers of users who are working in cooperatives; •Strong working relationships between mental health centres and their communities; •Successful consumer movement. Village Integrated Service Agency (VISA), Long Beach, California The Village Integrated Service Agency (VISA) in Long Beach, California (Los Angeles metropolitan area) was begun in 1988 as one of several pilot projects statewide designed to demonstrate that a fragmented lumbering mental health services system could be reorganized into small, integrated service agencies (ISAs) for high cost/high risk individuals with serious mental illnesses. Existing funds were consolidated and made available to be used by the ISAs in flexible ways to meet each individual person's unique needs. Programs are operated by non-profit mental health service agencies under contracts with funding authorities. The Village participates in a rigorous outcome evaluation project which encompasses all of the pilot projects and new ISAs. While all the pilot programs all were developed around the values of integrated services and individualized services and support, the VISA has evolved into a strong culture with the following core principles (Mandella, 1993; Strand, 1993; Ragins, 1993). It's service approach builds upon the work of a number of innovative service orientations, including the P/ACT model of assertive community treatment and the Strength's model of case management. •One stop shopping. Comprehensive and integrated services. The Village is a single supportive place were virtually any kind of support can begin. It serves as a fixed point of responsibility for the people it serves and provides most of the needed services itself, rather than brokering them out. The benefit of such consolidation is the reduce possibility of service gaps, redundant services, inefficiencies fro lack of coordination, and reliance on difficult inter-agency communication, and to maintain order and coherence in a member's personal life and service program. •Member driven personal support. Informal and non-authoritarian relationships between members and staff is central, with members active participants in al aspects of identifying personal goals and support needs. The service focus is on what individual members want and how to help them achieve it, rather than members choosing from a menu of services offered by the program. The term "personal support" is used in leu of "case management" and emphasis is put on seeing the whole person: values, strengths, obstacles, goals, culture, history, dreams, and so forth. •Responsibility for outcome for the WHOLE individual. There is a focus on wellness and health, not just illness or symptoms. This is important to help members see themselves as whole persons and not as "patients." While symptoms are acknowledge and individuals are helped learn how to manage them, they are considered to be only a part of an individuals life -- and not necessarily an obstacle to having friends, holding a job, living in an apartment, having fun. Success and change is measured in terms of quality of life of the members, and staff and members share accountability in achieving specific outcomes. Results are measured in the domains of living situation, employment, social relationships, physical health, education and learning, avoiding trouble with substance abuse and the law. •Intentionally blurred role boundaries. The professional-member relationship is purposefully blurred. The professional is not the sole expert or "provider of care." People get out from behind desks and talk together about whatever is of concern: work problems, religion, sex, dating, friends, and so forth. The Village is one of the programs which pioneered hiring mental health consumers into staff positions. •Partnership in Medication. Psychiatric consultants are available to the members of the Village. As in other aspects of the agency, partnership is foremost, and medication collaboration is a big part of overall rehabilitation. The psychiatrist role is to listen to what members say helps them, educate them about their considerations and medications, prescribe, as much as possible, the medications they wish to take, and then to assess with them collaboratively the results of the in terms of symptom management, assistance in achieving personal goals, and so forth. •Relationship to the REAL community. Member driven models such as the Village are based on the belief that people can progress if provided with appropriate material, social, and emotional supports. While sometimes very difficult, priority is given to helping individuals establish natural support systems, refine it and strengthen it. •Re-installation of family into the critical path of growth. Another area of challenge for many staff is to effectively engage families in the "growth path" of members -and for family members to understand and embrace the values and support concepts of the Village. However, this is acknowledged as an area of critical development within the agency. •Training. Staff and member training has been a foundation for the ongoing development of the Village -- particularly on-going training which reinforces material presented earlier and which provides people an opportunity to practice new skills between training sessions. Programs offered through the Village include •Community Support Teams. The agency is divided into self-managing teams, each with a capitated budget. Teams track costs and adjust expenses as necessary; the role of agency management is to give the teams the tools and information they need, then get out of the way. Each member has a Personal Services Coordinator (PSC) who provides support and assistance with problem solving throughout a long term one-to-one, "hands on" relationship. PSCs assist with coaching daily living skills, assisting with housing and work issues, and other quality of life related issues. The emphasis is on assertive outreach, in vivo care, and highly individualized treatment. Each team has affiliated psychiatrists to oversee the optimal use of psychotropic medications (not to lead the team), a staff person on-call to provide 24 hour crisis assistance. The teams will use brief psychiatric hospitalization when indicated. •Member financial services. The Village Bank offers savings accounts, check cashing, and loan dispersal. The Bank is operated as an agency business which hires members as tellers and data entry operators. Other member financial services are the Supported Money Management financial counselling and skill building service, and the Loan Program which provides emergency loans for food and shelter and personal loans for other items. •Vocational work sites and support services. A range of meaningful paid job options exist, including the Village Bank and •CAFE 456. A work site for members and the hub of social activity at the Village. The cafe participates in the local "Taste of Long Beach" food festivals with other area restaurants. •Village Mini-Mart. A work site which provides a range of items for sale to members. •Data entry and other administrative services for the agency. Personal service coordinators also assist individuals with finding and keeping volunteer or paid full and part time competitive positions in the community. While the Village does not have a designated program for persons with dual diagnosis mental illness and substance abuse disorders, a considerable portion of is members struggle with these issues. Treatment around these issues is integrated into the larger mix of agency services. VII. References and Resources Allen, JB Jr. and Granger, B (1997). Consumer-Run Entrepreneurial Businesses: Issues and Opportunities. In In Mowbray, CT, Moxley, DP, Jasper, CA, Howell, LL (1997). Consumers as Providers in Psychiatric Rehabilitation. Columbia, MD: International Association of Psychosocial Rehabilitation Services (IAPSRS). Anderson, D and Deegan P (1994). Overcoming Barriers to Effective Consumer/Survivor Participation on Boards and Committees. Unpublished manuscript. Anthony, WA (1994). The Vocational Rehabilitation of People with Severe Mental Illness: Issues and Myths. Innovations and Research. 3:2. 17-23. Anthony, WA (1993). Recovery From Mental Illness: The Guiding Vision of the Mental Health Service System in the 1990's. Innovations and Research. 2:3, 1724. Anthony, W, Cohen, M, Farkas, M (1990). Psychiatric Rehabilitation. Boston, MA: Boston University, Centre for Psychiatric Rehabilitation. Augello, T (1997). Personal communication. Beard, JH, Probst, RN, and Malamud, TJ (1982). The Fountain House Model of Psychiatric Rehabilitation. Psychosocial Rehabilitation Journal. 5. 47-54. Becker, DR, Drake, RE, Farabaugh, A, and Bond, GR (1996). Job Preferences of Clients with Severe Psychiatric Disorders participating in Supported Employment Programs. Psychiatric Services, 47:11. 1223-1226. Blanch, A, Fisher, D, Tucker, W, Walsh, D, and J. Chassman (1995). Consumer - Practitioners and Psychiatrists Share Insights About Recovery and Coping. Disability Studies Quarterly, 13:2, 17-20. Blankertz, L, and Robinson, S. (1996). Adding a Vocational Focus to Mental Health Rehabilitation. Psychiatric Services, 47:11. 1216-1223. Bond, GR, McGrew, JH, Fekete, DM (1995). Assertive Outreach for Frequent Users of Psychiatric Hospitals: A Meta-Analysis. The Journal of Mental Health Administration. 22:1, 4-16. Bond, GR (1994). Case Management and Psychosocial Rehabilitation: Can They Be Synergistic? Community Mental Health Journal, 30:4. 341-346. Bond, GR (1992). Vocational Rehabilitation. In Liberman, RP (ed.) (1992). Handbook of Psychiatric Rehabilitation. New York: Macmillan. Bond, GR, Drake, RE, Mueser, TK and Becker, DR (1996). Supported Employment for People with Severe Mental Illness: A Review. Psychiatric Services. In press. Brown, S (1983). Treating the Alcoholic: A Developmental Model of Recovery. New York: John Wiley & Sons. Burland, J (1995). Journey of Hope: A Family to Family Self Help Education Program. In Weisburg, D (ed.) (1995). The Journal: Self Help. Sacramento, CA: California Alliance for the Mentally Ill. 6:3. Campbell, J and Schraiber, R (1989). The Well-Being Project: Mental Health Clients Speak for Themselves. Sacramento, CA: The California Network of Mental Health Clients. Canadian Mental Health Association (CMHA) (1995). Discussion Guide on Mental Health Reform. Toronto, Ontario: Canadian Mental Health Association, National Mental Health Services Work Group. Canadian Mental Health Association, Ontario Division. (1996). A Values-Based Community Support Service System: A Values Clarification Project. Toronto, Ontario: Canadian Mental Health Association, Ontario Division, Mental Health Reform Implementation Subcommittee, Executive Director Network, Values Subcommittee. Canadian Mental Health Association, Ontario Division (1995). Respecting Case Management: Policy Document of the Canadian Mental Health Association, Ontario Division. Toronto, Ontario: Canadian Mental Health Association, Ontario Division, Policy Advisory Committee, Case Management Task Force. Carling, PJ (1995). Return to Community: Building Support Systems for People with Psychiatric Disabilities. New York: The Guildford Press. Centre for Psychiatric Rehabilitation (1997). Community Support Network News: States Helping States: P/ACT and Managed Care. Boston, MA: Boston University, Centre for Psychiatric Rehabilitation. Chamberlain, J, Rogers, S, and Ellison, ML (1996). Self-help programs: A description of their characteristics and members. Psychosocial Rehabilitation Journal. 19:3, 33-42. Chamberlain, J (1988). Concept Paper: Ex-Patient Self-Help Groups. Prepared for the Seventh CSP Learning Community Conference. Unpublished manuscript. Chamberlain, J (1990). The Ex-patient's Movement: Where We've Been and Where We're Going. The Journal of Mind and Behaviour. 1:3. 323-336. Consumer/Survivor Development Initiative (CSDI) (1993). Operational Guidelines: Hands-on Worksheet. Toronto, Ontario: Canadian Mental Health Association, Consumer/Survivor Development Initiative. Consumer/Survivor Development Initiative (CSDI) (1996). Project Descriptions. Toronto, Ontario: Canadian Mental Health Association, Consumer/Survivor Development Initiative. Cook, JA and Jonikas, JA (1996). Research on Community Integration of Persons with Psychiatric Disabilities: Current Knowledge, Future Directions, and Recommended Research Priorities. Chicago, IL: University of Illinois at Chicago, National Research and Training Centre on Psychiatric Disability. Cook, JA and Jonikas, JA (1996). Outcomes of Psychiatric Rehabilitation Service Delivery. New Directions in Mental Health Series. San Francisco: Jossey-Bass Publishers. Copeland, ME (1992). The Depression Workbook: A Guide for Living with Depression and Manic Depression. Oakland, CA: New Harbinger Publications. Copeland, ME (1994). Living Without Depression and Manic Depression: A Workbook for Maintaining Mood Stability. Oakland, CA: New Harbinger Publications. Copeland, ME (1994). Dealing With Depression and Manic Depression for People with Mood Disorders and Those Who Love and Support Them. Innovations and Research. 3:4, 51-58. Copeland, ME, Curtis, LC, Palmer HP (1996) The Recovery Institute: Knowing and Practising Recovery Skills. A Training Workshop. Burlington, VT: Trinity College of Vermont; Centre for Community Change through Housing and Support. Curtis, LC (1997) Integrating Recovery Principles into Policy and Practice: Participant Workbook. Burlington, VT: Trinity College of Vermont, Centre for Community Change through Housing and Support. Curtis, LC (1992). Supported Housing and Case Management. In Community. 2:4, 2-7. Curtis, LC, Montague, W, McCabe, SS, Caron, D, Harp, H (1991). Strategies for Increasing and Supporting Consumer Involvement in Mental Health Policy Development, Planning, Management, and Service Delivery. Burlington, VT: Centre for Community Change through Housing and Support. Danley, KS (in press). Long-Term Outcomes for Participants in a Career Education Program for Young Adults with Psychiatric Disabilities: Final report. Submitted to the National Institute on Disability and Rehabilitation Research (NIDRR). Boston, MA: Boston University, Centre for Psychiatric Rehabilitation. Deegan, PE (1997). Personal communication. Deegan, PE (1997). A Recovery Model for Using Psychiatric Medications. Lawrence, MA: National Empowerment Centre. Deegan, PE (1995). Coping with Voices: Self Help Strategies for People who Hear Voices that are Distressing. Lawrence, MA: National Empowerment Centre. Deegan, PE (1988). Recovery: The Lived Experience of Rehabilitation. Psychosocial Rehabilitation Journal. 11:4. 11-19. Deegan, PE, (1992). The Independent Living Movement and People with Psychiatric Disabilities; Taking Back Control Over Our Own Lives. Psychosocial Rehabilitation Journal, 15:3, 3-19. Dietzen, LL and Bond GR (1993). Relationship Between Case Manager Contact and Outcome for Frequently Hospitalized Psychiatric Clients. Hospital and Community Psychiatry. 44:9. 839-843. Dincin, , J. (1975). Psychiatric Rehabilitation. Hospital and Community Psychiatry. 33. 645-650. Dion G and Anthony, WA (1987). Research in Psychiatric Rehabilitation: A Review of Experimental and Quasi-experimental Studies. Rehabilitation Counselling Bulletin. 30. 117-203. Drake, RE, Teague, GB, Warren, SR (1990). Dual Diagnosis: The New Hampshire Program. Addiction and Recovery. June. 35-39. Ellison, ML, Rogers, ES, Sciarappa, K, Cohen, M, and Foress R. (1995). Characteristics of Mental Health Case Management: Results of a National Study. Journal of Mental Health Administration. 22. 101-112. Fairweather, GW (1980). The Fairweather Lodge: A Twenty-five Year Retrospective. New Directions in Mental Health. San Francisco: Jossey-Bass. Falloon, IRH, Boyd, JL, McGill, CW, Razani, J, Moss, HB, Gilderman, AM (1982). Family Management in the Prevention of Exacerbations of Schizophrenia. New England Journal of Medicine. 306. 1437-1440. Felton, CJ, Stastny, P, Shern, DL, Blanch, A, Donahue, SA, Knight, E, and Brown, C (1995). Consumers as Peer Specialists on Intensive Case Management Teams: Impact on Client Outcomes. Psychiatric Services. 46:10. 1037-1044. Frank, LR (1995). Influencing Minds: A Reader in Quotations. Portland OR: Feral House. Goldstein, MJ and Rodnick, EH. (1975). The Family's contribution to the Etiology of Schizophrenia: Current Status. Schizophrenia Bulletin. 14, 48-63. Goering, P (principle investigator) (in preparation). Review of Best Practices in Mental Health Service Delivery. Prepared for Health Canada and the Advisory Network on Mental Health by Clark Institute of Psychiatry, Health Systems Research Unit. Granger, B, Baron, RC, and Robinson, S (1996). A National Study on Job Accommodations for People with Psychiatric Disabilities: Final Report. Philadelphia, PA: University of Pennsylvania, Matrix Research Institute, Research and Training Centre on Mental Illness and Work. Hanson, JG and Rapp, CA (1992). Families' Perceptions of Community Mental Health Programs for their Relatives with Severe Mental Illness. Community Mental Health Journal, 30:4, 181-197. Harris, C (1995). Employment Options: A Review of Employment Opportunities for People with Long Term Mental Illness. A Churchill Fellowship Report. Auckland, NZ: Framework Trust. Haas L and Mead, S (1996). Peer Support: Review of Program Services. Claremont, NH: Stepping Stone Peer Support Centre, Inc. Hatfield, AB (1988). The Role of the Family in the Rehabilitation Process. National Rehabilitation Association 1988 Switzer Monograph. 82-94. Hatfield, AB and Lefley HP (1993). Surviving Mental Illness: Stress, Coping, and Adaption. New York: Guildford Press. Hodge, M and Draine J (1993). Development of Support through Case Management. In Flexer R and Soloman P (eds.) Psychiatric Rehabilitation in Practice. Boston: Andover Medical Publishers. Hughes, R (1994). In IAPSRS Publications Committee (1994). An Introduction to Psychiatric Rehabilitation. Columbia, MD: IAPSRS. Hutchings, GP, Emery, BD, Aronson, LP (eds). (1996). Housing for Persons with Psychiatric Disabilities: Best Practices for a Changing Environment. Technical Assistance Tool Kit. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD). Hyde, AP and Goldman, CR (1993) Common Family Issues that Interfere with the Treatment and Rehabilitation of People with Schizophrenia. Psychosocial Rehabilitation Journal. 16:4,63-74. Institute for Community Inclusion (1995). Employment Specialist Training Manual. Boston, MA: Institute for Community Inclusion. Joyce, S. (1995). Discovery: Personal Planning with People Who Receive Support. Kitchener, Ontario: Canadian Mental Health Association, Waterloo Regional Branch and The Collective for Community Action. Kanapaux, W (ed.) (1997) Consumer Advocates Continue Building National Presence. Mental Health Weekly. 7:16, 1-2. Kaufman, CL (1995). The Self-help Employment Centre: Some Outcomes From the First Year. Psychosocial Rehabilitation Journal. 18:4, 145-162. Lavin, D and Everett, A (1995). Working on the Dream: A Guide to Career Planning and Job Success. St. Augustine, FL: Training Resource Network. Lefley, HP (1994). Rehabilitation in Mental Illness: Insights From Other Cultures. In IAPSRS Publications Committee (eds.) (1994). An Introduction to Psychiatric Rehabilitation. Columbia, MD: IAPSRS. Mandella, V (1993). Closing in on Putting It Together" In Weisburg, D (ed.) (1993). The Journal: Does Anything Work -- the ISA Experiment. Sacramento, CA: California Alliance for the Mentally Ill. 4:2, 12-14. Mancuso, L (1995). Renaissance of a Mental Health Clinician. Unpublished. Marrone, J, Candolfo, C, Gold, M, Hoff, D (in press). Just Doing It: Helping People with Mental Illness Get Good Jobs. Boston, MA: Institute for Community Inclusion, Centre for Promoting Employment. Matrix Institute (1997). The Facts about Mental Illness and Work: An Informational Brochure. Conference Handout at International Association of Psychosocial Rehabilitation Services (IAPSRS) 1997 Conference in Vancouver, BC. Philadelphia, PA: University of Pennsylvania, Matrix Research Institute, Research and Training Centre on Mental Illness and Work. McGrew, JH and Bond, GR (1995) Critical Ingredients of Assertive Community Treatment: Judgements of the Experts. Journal of Mental Health Administration. 22 113-125. Mead, S (1997). Personal communication. Mead, S (1995). Stepping Stone Peer Support Manual. Claremont, NH: Stepping Stone Peer Support Centre, Inc. Moller, MD and Murphy, MF (1997). The Three R's Rehabilitation Program: A Prevention Approach for the Management of Relapse Symptoms Associated with Psychiatric Diagnosis. Psychiatric Rehabilitation Journal. 20(3). 42-48. Mount, B (1990). Making Futures Happen: A Manual for Facilitators of Personal Futures Planning. St. Paul, MN: Metropolitan Council. Developmental Disabilities Case Management Project. Mowbray, CT and Tan, C (1993). Evaluation of an Innovative Consumer Run Service Model: Drop In Centre. Innovations and Research. 1:2, 19-24. Mowbray CT and Moxley DP (1997). Consumers as Providers: Themes and Success Factors. In Mowbray, CT, Moxley, DP, Jasper, CA, Howell, LL (1997). Consumers as Providers in Psychiatric Rehabilitation. Columbia, MD: International Association of Psychosocial Rehabilitation Services (IAPSRS). Mowbray, CT, Bybee, D and Shriner, W, (1996). Characteristics of Participants in a Supported Education Program for Adults with Psychiatric Disabilities. Psychiatric Services. 47:12, 1371-1377. Mueser, KT, Bond, GR, Drake, RE, Resnick, SG (in press). Models of Community Care for Severe Mental Illness: A Review of Research on Case Management. Schizophrenia Bulletin. Muser, KT and Gingerich, S (1994). Coping with Schizophrenia: A Guide for Families. Oakland, CA: New Harbinger Publications, Inc. Nelson, CJ and Edmonds, BC (1997). A Leadership Academy for Consumers and Families. Conference materials handed out at IAPSRS Conference, Vancouver, Ontario, 1997. Charleston, WV: West Virginia State Department of Health and Human Resources, Office of Behavioural Health Services. Northeast Independent Living Program (undated). Services to the Mental Health Community that Share, Educate, and Empower. Lawrence, MA: Northeast Independent Living Program, Inc. Palmer, HP and Carling PJ (1997). Developing an Implementation Model for Community Support Services in Ontario: An Analysis of policy Documents and Suggestions for Next Steps. Burlington, VT: Trinity College of Vermont, Centre for Community Change through Housing and Support. Pape, B (1997). Personal communication. Paulson, RI, Kiney, R, Herinckx, H, and Clark, G (1997). Consumers and NonConsumer Providers Practice Differently? Presentation and handout materials at IAPSRS conference, Vancouver, British Columbia. Unpublished material. Powell, I and Knight E (1992). Initiatives Related to Coping and Recovery: SelfDirected Rehabilitation. Community Support Network News. Boston, MA: Centre for Psychiatric Rehabilitation. Ragins, M. (1993). Partners in Medication Collaboration. In Weisburg, D (ed.) (1993). The Journal: Does Anything Work -- the ISA Experiment. Sacramento, CA: California Alliance for the Mentally Ill. 4:2. Rapp, CA (1996). The Active Ingredients of Effective Case Management: A Research Synthesis. In Geisler, LJ (ed) (1995). Case Management for Behavioural Managed Care. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental health Services Administration, Centre for Mental Health Services. Rapp, CA (1988). The Strengths Perspective of Case Management with Persons Suffering from Severe Mental Illness. Lawrence, KS: University of Kansas School of Social Welfare. Ryglewicz, H. (1985). How Can Professionals Help Families -- and Patients: Issues and Approaches. Tie Lines. 2:1, 1-8. Segal, SP, Silverman C, and Temkin, T (1995). Characteristics and Service Use of Long Term Members of Self Help Agencies for Mental Health Clients. Psychiatric Services. 46:3, 269-274. Scott, P, Pomeroy, E, and Pape, B (1995). Tools for Consumer Participation. Toronto, Ontario, Canadian Mental Health Association. Sharac, J., Yoder, B, and Sullivan, AP (1997). Consumers as Supported Education Mentors. In Mowbray, CT, Moxley, DP, Jasper, CA, Howell, LL (1997). Consumers as Providers in Psychiatric Rehabilitation. Columbia, MD: International Association of Psychosocial Rehabilitation Services (IAPSRS) Soloman, P (1992). The Efficacy of Case Management Services for Severely Mentally Disabled Clients. Community Mental Health Journal, 30:4, 163-181. Soloman, P and Drain, J (1995). The Efficacy of Consumer Case Management Team: Two Year Outcomes of a Randomized Trail. Journal of Mental Health Administration. 22. 135-146. Stepping Stone (undated). Stepping Stone Peer Support Centre. Claremont, NH: Stepping Stone Peer Support Centre, Inc. Strand, K. (1993). Getting out of the Box and Getting into the World. In Weisburg, D (ed.) (1993). The Journal: Does Anything Work -- the ISA Experiment. Sacramento, CA: California Alliance for the Mentally Ill. 4:2. Stroul, BA (1988). Community Support Systems for Persons with Long Term Mental Illness: Questions and Answers. Rockville, MD: National Institute of Mental Health, Community Support Program. Spaniel, L, Gagne, C, Koehler, M (1997) Psychological and Social Aspects of Psychiatric Disability. Boston, MA: Boston University, Centre for Psychiatric Rehabilitation. Sullivan, WP (1994). A Long and Winding Road: The Process of Recovery from Severe Mental Illness. Innovations and Research. 3:3, 19-27. Surber, RW (ed.)(1994). Clinical Case Management: A Guide to comprehensive Treatment Services. Thousand Oaks, CA: Sage Publications. Teague, GB, Drake RE and Ackerson TH (1995). Dartmouth Assertive Community Treatment Fidelity Scale. Hanover, NH: Dartmouth University. Trainor, J, Pomeroy E, Pape, B (1993). A New Framework for Support for People with Serious Mental Health Problems. Toronto, Ontario: The Canadian Mental Health Association. Unger, K (1992). Adults with Psychiatric Disabilities on Campus. Washington, DC: American Council on Education, Health Resource Centre. Unger, K (1993). Creating Supported Education Programs Utilizing Existing Community Resources. Psychosocial Rehabilitation Journal. 17:1, 11-23. Valentine, MB and Capponi P (1989). Mental Health Consumer Participation on Boards and Committees: Barriers and Strategies. Canada's Mental Health. 37:2, 8-12. Vandergang, AJ (1996). Consumer/Survivor Participation in the Operation of Community Mental Health Agencies and Programs in Metro Toronto: Input or Impact? Canadian Journal of Community Mental Health. 154-170. Van Tosh, L (1994). Consumer/Survivor Involvement in Supportive Housing and Mental Health Services. The Housing Centre Bulletin. 3:1, 1-6. Vermont Department of Mental Health (1996). A Position Paper on Recovery and Psychiatric Disability: Legislative Summer Study Committee. Waterbury, VT: Vermont Department of Mental Health. Viccora, E, Perry, J, Mancuso, L. (1994). Exemplary Practices in Employment Services for People with Psychiatric Disabilities: A Review of State Mental Health Initiatives Nominated for NASMHPD's 1993 Exemplary Employment Services Award. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD). Vosler-Hunter, RW (1990). Families and Professionals Working Together: Issues and Opportunities. Focal Point. Portland, OR: Portland State University, Research and Training Centre on Family Support and Children's Mental Health. Weisburg, D (ed.) (1995). The Journal: Self Help. Sacramento, CA: California Alliance for the Mentally Ill. 6:3. Weisburg, D (ed.) (1994). The Journal: Recovery. Sacramento, CA: California Alliance for the Mentally Ill. 5:3. Weisburg, D (ed.) (1993). The Journal: Does Anything Work -- the ISA Experiment. Sacramento, CA: California Alliance for the Mentally Ill. 4:2. Weisburg, D (ed.) (1990). The Journal: Rehabilitation. Sacramento, CA: California Alliance for the Mentally Ill. 1:3. Whelton, C, Pawlick J, Cardamone, J. (FIND CITE). Involving Families in psychosocial Rehabilitation. Psychiatric Rehabilitation Journal. Wisconsin Blue Ribbon Commission on Mental Health (1997). Wisconsin Blue Ribbon Commission on Mental Health: Final Report. Madison, WI: State of Wisconsin, Office of the Governor. Wolff, N, Helminiak, TW, and Diamond, RJ (1995). Estimated Societal Costs of Assertive Community Mental Health Care. Psychiatric Services, 46:9, 898-906. Yess, JP (1977). What Families of the Mentally Ill Want. Community Support Service Journal. 2:1, 1-3.