Communication Strategy - Divisions of Family Practice
advertisement

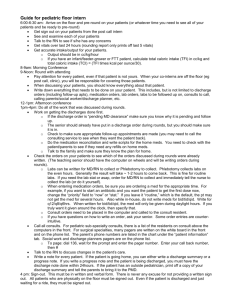
May Report on Discharge Barriers Thompson Region Division of Family Practice Transitions in Care - Acute to Community Communication and Information Exchange for the Frail Elderly 310 Nicola Street, #209 Kamloops, BC V2C 2P5 2013 EExxeeccuuttiivvee SSuum mm maarryy Two patient journey mapping exercises took place in November, 2011 and March, 2012. The intent of the journey mapping was to better understand the experience of frail elder patients with co-mobidities as they went through the health care system in Kamloops. In particular, it was highlighted that there was room for improvement as the frail elder was discharged from acute to home or to a residential facility. Since October, 2012 an environmental scan has taken place and feedback received through numerous mechanisms, to gain a better understanding of the experience of health care providers and others who impact, or are impacted by, the discharge process. Common themes were experienced by all providers, and aligned with the information learned through the patient journey mapping. Discharge processes were inconsistent, and there was a lack of communication and coordination between providers, patient and family to ensure the necessary support systems were in place for a successful discharge. There is need for greater coordination, communication, collaboration and education. Most importantly, consistency in delivering health care services is critical. This report identifies the challenges and opportunities available to enhance communication and information transfer between the health care providers, hospitalists, specialists, community physicians, patient, family, and supporting community organizations and services. The following key categories were identified for improvement: Standards and processes Forms and documentation Discharge communication Health care services and discharge planning Medication Organizational structure and resourcing Education Health Records/Technology Other This presents significant opportunity for testing and evaluating improvements to address some key gaps highlighted in the categories identified. A few opportunities highlighted for improvement include: 2 Development of consistent discharge standards. Ensuring discharge summaries are distributed in a timely manner. Streamlining key forms required that support the discharge process. Development of discharge packages for the patient and family, including providing education on critical discharge information. Development of consistent communication processes for CIHS to inform physicians/specialists on patient status updates. Development of consistent communication processes between RIH and CIHS, residential, external providers such as pharmacists, physicians, etc. This includes those that are doing the discharge planning and includes hospitalist and Emergency to community physician. For complex discharges, diverse multi-disciplinary teams coming together with patient and family to do comprehensive discharge plans (including CIHS, RIH Pharmacy and Community Physician). A consistent patient navigator/case manager that supports the patient and health care providers once patient discharged. Polypharmacy addressed at key transfer and transition points in patient’s care and when goals change and medication reconciliation at discharge. Providing education and resources to health care providers and physicians explaining community resources available and outlining residential care facilities and services provided. Next steps include prioritizing the opportunities identified, confirming what work may be in process within our region to avoid duplication, and beginning small tests of change through multiple PDSA cycles. 3 PPrroojjeecctt O Ovveerrvviieew w Through a Memorandum of Understanding with the Provincial Transitions in Care program, the Division, Royal Inland Hospital and Community Integrated Health Services, it was determined that the process of frail elderly patient transitioning out of acute care settings needed to be reviewed in detail. This project focuses primarily on the relationships between primary care, hospitalists, specialist support, community care supports, and acute care practitioners. The relationships with external and community organizations and professionals such as community pharmacists, private residential care homes, and community seniors organizations such as Seniors Outreach and ASK Wellness has also been considered. It was agreed upon that improved communications and information transfer is needed between specialists, hospitalists, family physicians, in hospital and community services allied professionals, and patients, their families and caregivers. Project goals include enhancing discharge communications and knowledge transfer tools resulting in better patient outcomes. The target population includes: Frail Elderly - Acute to Residential Care (including IH funded beds, IH facilities, P3 facilities and Hospice) Frail Elderly – Acute to Home with/without support of community services The key objectives are: To better define the communications and knowledge transfer barriers between specialists, hospitalists, family physicians with and without privilege’s, in hospital and community services allied health professionals, patients and families To recommend improvements To test and report on effectiveness of at least one qualitative improvement area AApppprrooaacchh A number of approaches were used to solicit input and feedback on the transition from acute to home and residential. Key approaches included: 1:1 meetings Focus groups Process mapping 4 Review of transition case studies A diverse group of individuals and stakeholders participated in providing feedback. This includes those who do the discharging and those on the receiving end of the discharge. Stakeholders include: Mental Health and Home Health allied professionals and nursing Acute allied professionals and nursing Family Physicians Specialists Hospitalists Pharmacists (in hospital and community) Seniors Outreach ASK Wellness Residential staff (IH funded and Private) Aboriginal Health providers Hospice staff Patients (through the Patient Journey Mapping exercise) RReessuullttss “There are no shortcuts to any place worth going”. Beverly Sills The information gathered from the various perspectives resulted in similar views and, in the majority of cases, highlighted lack of communication and coordination of health care services resulting in a negative impact for the patient. Information provided was based on individual perspectives and experiences. It is recognized that all health care providers are tremendously busy and doing their best to meet the needs of the patients. This report is not intended to infer blame to anyone. The feedback has come from the providers directly. It is understood that there are challenges and obstacles within the system for health care providers to provide the best care possible. The barriers presented will allow opportunities for improvement to enhance the patient’s experience, their health outcomes, and in turn positively impact 5 the health care providers experience in delivering care and enhancing the lines of communication. There is opportunity for providers to think beyond a single moment in time and recognize it “takes time to save the time” at a future date. As Scott Adams says “Of course I don’t look busy, I did it right the first time”. If the time is put in upfront preparing comprehensive and collaborative care and discharge plans with the multidisciplinary functions (acute, community, and residential), patient/family, hospitalist, community family physician, including providing education on the discharge plan, medication utilization, and ensuring the support services are provided at the right time, it will result in fewer readmissions to the hospital and the cycle starting over again by the health care providers. Key themes were identified and aligned with all perspectives, including the patient journey mapping, as follows: Standardized Processes o There are a lack of policy, standardized processes and procedures, particularly on the discharge plan, to ensure that consistent discharge planning is occurring throughout all floors, at all times (weekdays and weekends), and when the hospital is at, or over capacity. At times, discharges have occurred without a written physician’s order, which could place the facility at risk from a legal/liable perspective. o Lack of clear guidelines for short stay residential beds. o Multiple health care providers review charts and prioritize discharge (eg. Patient Care Coordinator and Community Access Coordinator), and multiple providers conduct individual assessments of patient (Emergency, Hospitalist, Allied Care workers, etc.). This results in duplication of work and reduced communication between providers, and ultimately overwhelms the patient. o Process to identify aboriginal health patients is inconsistent. Information not transferred to nursing units or other facilities such as Ponderosa. Forms/Documentation o There are a significant number of forms utilized for discharge, but utilized inconsistently. Forms include transfer forms, referral forms, assessments (Palliative, Long Term Care, etc.), pre-admission documentation, readmission checklists for residential facilities, and so on. Forms are incomplete and/or little to no information is sent with patients being discharged to other facilities 6 for follow up care. It is also noted that documentation sent with the patient when the patient is sent to hospital from a residential care facility appears not to be referred to or read in detail, largely due to the large volume of material. The Advance Care Directives, which is of critical importance in this population, is often not present or buried in the mound of paper work send and difficult to tease out. Admission, Discharge and Transfer Communication The single biggest problem in communication is the illusion that it has taken place. George Bernard Shaw o Approximately 70% of elderly are cognitively impaired at discharge (in accordance with one hospitalist interviewed). Therefore, it is very difficult for the patient to fully comprehend the information presented by the health care providers. There is a lack of written discharge instructions, medication information, and understanding by the patient and their family provided at discharge. o There has been consistent feedback that information in Emergency “stays in Emergency” and does not get shared. For example, chart notes may not always be sent to community physician, nursing homes do not get chart notes at all, and the lack of notes prepared at admission is a concern. If the notes are received, the notes are illegible. o Residential care facilities report that there is a lack of communication with the hospital for their residents. This includes lack of verbal report with nursing, paperwork and documentation to provide understanding required for follow up care and medications. Residential care facilities also have provided feedback that health information sent with patient to hospital appears not to be read in detail, if at all. o There is not always verbal or warm handover from facility to physician/nurse to triage when a patient goes into Emergency or hospital, especially regarding goals of care and advanced directive. o Community physicians have confirmed that more communication with hospitalists at admission and discharge outlining medication condition/diagnosis, medication changes and code status would be helpful; discharge summaries are often delayed up to a month which is an issue if patient comes in for follow up appointment. Physician has no information. 7 o Access to speak with a family physician about a patient at admission and discharge by the hospitalist can be a barrier. o Rehab assessment and discharge notes not being referred to by physicians, and other health care providers. o Below are 3 cases identified from two residential facilities demonstrating poor communication: • A patient from a residential facility was admitted to RIH with detailed instructions that the patient is unable to get out of bed and needs a transfer with a lift. Hospital staff tried to get her out of bed to go to the bathroom without a lift and the patient broke her ankle. Patient has been declining since that incident. • A resident was sent to emergency for x-rays and assessment following a fall. The resident was sent via ambulance with a family member. The nurse had a call from the hospital indicating that the resident did have a fractured rib. However, when the resident returned the family member advised she had been told that there was not a fracture. No paperwork was received to confirm. • Resident was in hospital for over 3 weeks. The resident was discharged on Saturday. No paperwork was sent with resident and no report from RIH nurse to notify of transfer or provide any information. Residential nurse called to hospital for report and was told to call back as nurse was going on break. This appears to be the “norm”. Health Care Services and Discharge Planning There are opportunities to enhance care for the betterment of the patient to support the care plan and discharge process. A number of areas have been identified as follows: Acute o Complexity of frail elderly has increased dramatically and patients more complicated with multiple co-mobidities. o Elderly are not mobilized or supported soon enough in hospital so they deteriorate the longer they are there. The Community Access Coordinators (CAC’s) confirm that it is difficult to screen frail elderly and start discharge planning process in Emergency due to workload. More rehabilitation services are needed in Emergency and throughout hospital to ensure mobilization occurs in a timely manner for elderly. Rehab referrals are not occurring soon 8 enough resulting in Rehab assessing patient at discharge (eg. getting referral same day as discharge). Patients need to be getting up more regularly prior to discharge date. o Discharges of elderly occurring from the Emergency room very late or throughout the middle of the night, when the mode of safe transport, is often lacking. If they are being discharged late to home or to a residential facility, support systems are not in place and the facility may be locked preventing readmission of the resident. o If patient is transferred within the hospital prior to the discharge plan being finalized, it results in duplication of work between the two wards and lack of continuity of care. o Discharging occurring without ensuring appropriate systems, supports, referrals or services are in place or coordinated accordingly. This can include Community Home Health Nursing, QRP, Rehab, Home Support, medications, housing, referrals to Mental Health, Heart Program, equipment (Red Cross), food in fridge, etc. This also includes confirming a patient’s home is safe prior to patient being discharged, confirmation that the patient’s caregiver is able to care for the patient at home, and the patient is mobilized and able to transfer. o Lack of communication with community physician – this includes at admission and discharge or when a patient has passed away. As one rural community physician advised, she may find out a patient has been in hospital only by receiving blood work or a family member calling. o Lack of consistent coordinated discharge plan occurring with multidisciplinary functions for complex patients in particular (Nursing, Rehab, Social Work, in house Pharmacist, Heart Program, Hospitalist, Community Physician, Specialist, Community Integrated Health Services, Patient/Family). o Lack of knowledge and consideration by acute staff on what happens when patient leaves the hospital (eg. no food in the house, no medications delivered, home safe for patient and community health care providers, etc.). o Hospitalist/Most Responsible Physician ensuring patient understands diagnosis (eg. patients seen by Home Health not understanding their medical diagnosis such as diabetes or deemed palliative). o Discharges happening too soon and discharge plans are not comprehensive enough. On 1 South, it is anticipated that 50% fail after discharge (anecdotal). o Below are 3 cases that demonstrate concerns in this area. 9 • In May 2012 and 81 year old female living at Kamloops Seniors Village (assisted living) went to Emergency with leg weakness. She was discharged back home the same day by the ambulance and a referral to the Quick Response Program (QRP). The ambulance left the patient at home in her power chair. QRP went in to see the client the same day to set up home support, but did not assess clients’ transfer. Client spent the night in her power chair. Community Occupational Therapy went in to see client the following day and realized the patient could not transfer out of her power chair and was incontinent. The patient was readmitted back to Emergency and 3 West for additional 8 days. • In early 2011, a patient had been seen multiple times and admitted into hospital with failure to thrive. Physicians confirmed that this patient was not stable to be discharged home and was becoming too difficult for his wife to manage him at home and he required placement. Despite documentation by two physicians, patient was discharged home without additional supports arranged. By this point, the patient’s wife was unable to cope and presented to her family doctor with a note that she was no longer able to speak and was sobbing uncontrollably. After a nurse was brought in from the Elderly Services Program, she was finally able to share that when the patient was brought home she was unable to get him into the house. The patient kept falling on the pavement and in the yard. Finally neighbors noted this and came to help. The electric chair just purchased for him was inappropriate and dangerous as the patient kept sliding out from the chair. His wife was unable to get him up off the floor and had to keep calling neighbors to assist. The patient was incontinent of bladder and bowel. The nurse from Elderly Services advocated on behalf of this couple for a respite bed. The wife stated that if she had not been there to help her, she would have gone to Emergency to be admitted to 1 South. • Patient admitted to hospital through Emergency with mental health issues. This was a difficult discharge as there was no housing available for the patient. Eventually patient was discharged to Scott’s Motor Inn with no shoes and limited clothing and no referral to Mental Health. Community Integrated Health Services (CIHS) As patients get discharged sooner from acute care, the increased level of complexity of care is transferred to providers in community, who in many cases, many not have the tools and resources to handle the higher level of care. Key issues for CIHS include: 10 o Home Health not consistently part of multidisciplinary team participating in complex discharge planning at RIH. o Home Health operates in time slots for care vs. continual assessment. For example, a nurse may go into a home to change a dressing for a 15 minute time slot, but may not have time to assess, identify or respond to other issues. o There are long waiting lists for long term care assessments resulting in patients being readmitted to hospital as “failure to thrive” and having to go through the process multiple times before assessment and ability to access long term care. If a patient suffers a major stroke for example, they often need immediate placement in long term care. This is currently not available and therefore they get discharged home with the expectation that they will be readmitted to hospital 3 times before assessment and placement. o Lack of Quick Response services (QRP) available for patients. o Services are very limited in remote and rural locations, including areas within a 25 minute drive (Savona). o Lack of communication from Home Health and Rehab back to community family physician and specialist. o One year wait list for mental health assessments for elderly services. Residential/Ponderosa o Many similar discharge concerns expressed for Ponderosa as it relates to acute/CIHS. Concern expressed that providers were not getting enough communication, discharge summary, referrals and medication information from Ponderosa (Pathway to Home). o Residential facilities contact family physicians on weekends by fax with concerns for resident. Physicians are not in their offices on the weekends and therefore would not receive the faxes until the following Monday. o Heart program does not see referrals from Ponderosa. Wound Care Follow up on wound care needs to improve. 11 Medication A number of concerns regarding medication issues that impact the care of patients, have been identified, including: o Medication orders missing at discharge or discharge prescriptions and reconciliation not complete. o Home Health does not get medication information or orders needed for patients; medications a significant issue in delivering home health nursing services and medication management for patients. o Community family physicians unaware of medication changes. o Community pharmacist not provided enough lead time to prepare medications prior to patient discharged, particularly if blister packing is required. RIH does not contact community pharmacists to confirm patient discharge. Community pharmacists spend significant amount of time following up with physicians and hospitalists to clarify prescriptions. When pharmacists call for information, health records have been filed, the most responsible physician has changed, and if medications have been “auto-subbed” and the pharmacist is unable to get the information required, it creates challenges. As well, pharmacists may have to redo orders if not advised to blister pack initially. This results in additional costs for the patient or Pharmacare, and impacts the human resources required to fulfill the order right the first time. o RIH in-house pharmacy requires advance notice of discharge to prepare pass medications in a timely fashion. In-house pharmacy does participate in some discharge planning, medication instructions to patients upon discharge, medication reconciliation or polypharmacy at discharge, but there is opportunity to expand. There is currently limited pharmacy coverage in Emergency, which would support the medication reconciliation at discharge from Emergency. o A review of medications in the patient’s home is not done. When a patient is discharged from hospital, medication changes have typically occurred. The patient may have vitamins, over the counter medications, and old medications prior to hospital admission lying around their home. This can result in patients taking medications inappropriately, creating adverse drug reactions, and possible readmission to hospital. o Medications that need special authority require an understanding by the Community Physician of patient history. If this is an unattached patient that they have agreed to take on, they will not have history. The hospitalist or specialist have signed off on discharge medications that require special authority and the family physician is left trying to determine if the patient qualifies or not. 12 Organizational Structure and Resourcing From the feedback, there are a number of areas that impact discharge planning due to resourcing and organizational structure within the health authority. These areas may not be the top priorities for testing cycles of change through this initiative, however, they should be mentioned for awareness and consideration by the relevant leadership teams. o Health care is a 24/7 business. However, many key roles operate primarily Monday-Friday or have significantly reduced coverage on the weekends or do not have extended hours (eg. Rehab, CAC, Social Work in acute; no weekend convalescent care or rehab in Ponderosa on weekends; Mental Health and Home Health in community). Family physicians have limited availability on the weekend, Aboriginal Health does not have health care staff available on weekends on reserves to provide support to discharged patients and Red Cross is not open for patient to get required equipment. This makes it difficult to provide consistent and comprehensive care and support for discharged patients. As identified by acute Rehab, the resourcing and care model for Rehab has not changed since the 80’s in contrast to the drastic changes in healthcare model in the last two decades. o Health care operates in siloes. More integration between acute and community integrated health services is needed to remove fragmented service and deliver the best care for patients. o Lack of case management for the patient at discharge. One central go-to person to support navigation for patient and health care providers is needed. o Ponderosa does not have a CAC/Discharge Planner or Patient Navigator at their facility. o RIH does not have a Pharmacist in Emergency. o Ability for CIHS to see patients in a timely manner - Ambulatory Nursing Clinic is at capacity and there can be a delay in getting Home Health and Home Support services in when patient ready for discharge (capacity issues). o No overnight home support services available. o Lack of Home Health and Home Support available in rural areas. o Long Term Care assessment process with its wait list is challenging with individuals getting discharged, readmitted to hospital with failure to thrive multiple times before assessment can be provided. 13 o CAC’s do utilization, as well as discharge planning. This has impacted their ability to have a clear focus on discharge planning and workload has been highlighted as a concern. For example, it can take 4 to 5 days on average for an discharge assessment by CAC and 6 days from the stepdown unit; elderly demobilize quickly so that creates issues. CAC’s have been integrated into the acute care setting which is beneficial, but they must have a strong knowledge of the services available in community, which many do not. o Frail elderly are mixed with general population on 1 South. It is very difficult for frail elderly to get better when they are in a small space with younger mentally ill/psychotic patients. Space is a big issue for this population with mental health. o There is significant change occurring in health care resulting in resource constraints, roles, responsibilities and reporting structures changing. There are scheduling changes, employees changing positions frequently, a multitude of vacancies at any given time, attrition and turnover. This results in some employees not in their roles long enough to be oriented well or gaining knowledge and experience that comes with time in a role. This is significant as it impacts role clarity for employees, which in turn impacts the continuity and consistency of care provided. Education Many areas of education are needed for health care providers, patients and families, including: o Mental health (dementia, delirium protocols, medications). o Community services available (within health authority and external). o Protocols and assessments (eg. Hospice Palliate Care Assessment and protocols). o Assisted Living/Residential facilities – types and levels offered within region; understanding of resources and services available for residents (eg. assisted living charge for nursing services vs. Home Health); hours of operation so patients have support systems in place and can get in. o Care plans, diagnosis information, discharge instructions and medication information for patients and families. o Resources, support and education available for patients and families (successful aging). Seniors are facing many emotional, physical and mental changes and they need to participate in the process. 14 o Orientation of health care providers (orientation in roles, orientation on roles of others in both acute/community, ongoing training on safe handling of patients, etc.). o Health Programs (Heart program, Diabetes, Nutrition, King Street etc.) – for patients, families and health care providers. o Education for health care providers on Aboriginal organizations, health services available and federal health system vs. provincial health system for aboriginal patients. o Education on guidelines and policy for long term care. o Health Records/Technology Having the right tools in place enables people to do their work as efficiently as possible. There are some key items impacting the efficiency and effectiveness of the discharge process. o Charts misfiled and unorganized. o Information in held in multiple places: Meditech, Hot Files, Patient Chart. o Meditech – Rehab/Social Work enter notes in system, but they are not printed out and placed in chart, Nursing does not chart on system, so only paper notes are kept in chart, Rehab, Social Work and CAC notes not referenced enough by physicians and nursing. o Many health care providers cannot access Meditech. o Notes are not transcribed in a timely manner to facilitate effective discharge communication for family physicians and specialists, which is critical for follow up. o All computers need WORD program on it and more computers are needed. o Physicians are unable to type progress notes in Meditech. o Lack of Wi-Fi in RIH for good access. o Meditech does not allow for multiple screens to be opened. o Difficult process for health care providers to access Pharmanet. 15 Other o Discharge plan done in RIH and when patient is repatriated to another facility, discharge plan starts over. o Lack of lab and follow up in community after discharge. o Patients may stay in a hospital bed longer than required while sorting financial needs out at a cost of $1,300/day or be discharged home unsafely. Residential short stay bed costs ($31.51 a day); this is approximately $900/month. Family agendas and housing are big issues for discharge for frail elderly (eg. family sells home or family doesn’t want elderly parent discharged home). o Unattached patients are a significant concern for continuity of care for patient. o Elderly may not have the ability or means to complete the various paperwork in order to prove income to get necessary services. o Lack of public transportation for patients in both city and rural areas (eg. HandyDart). o Lack of ability for rural patients to get services (home health, follow up tests or care required, etc.). o Geriatric clinic and multidisciplinary team needed to provide health care for seniors. This will support seniors with advanced alzeimers and prevent admission to hospital. SSoolluuttiioonnss Although there are a number of gaps identified, it is important to recognize that there are multiple solutions available to resolve the gaps. Many system improvements are currently underway. The following guiding principles will assist with prioritizing solutions identified for testing: Alignment with the project charter and key objectives to enhance communications and knowledge transfer between specialists, hospitalists, family physicians with and without privilege’s, in hospital and community services allied health professionals, patients and families Alignment with the feedback received from health care providers, patients and families 16 Alignment with “SMART” principles – specific, measurable, achievable, realistic and timely (small tests of change) Avoids duplication of work or conflict with other initiatives or systems improvements underway that may address similar gaps In reviewing case studies, the discharges that went particularly well had a common theme. The required health care providers came together at the right time to develop and deliver on a comprehensive care and discharge plan. Services were coordinated and communicated well between the health care providers, patient and family. With this in mind, the following areas have been identified as key priorities for improvement: o Development of discharge standards. o Development of discharge summary turnaround times for community physicians. o Streamlining key forms (eg. transfer forms, discharge summary, assessment forms, checklists required). o Development of customized discharge packages with clear discharge instructions, medication information, follow up and contact information, considering literacy. Provide education to patient and family. o Development of communication processes for CIHS to inform physicians/specialists on patient status. o Development of communication processes between RIH and CIHS, residential, external providers such as pharmacists, physicians, etc. This includes those that are doing the discharge planning and includes hospitalist and Emergency to community physician. o For complex discharges, conduct a pilot of diverse multi-disciplinary teams coming together with patient and family to do comprehensive discharge plans (including CIHS, RIH Pharmacy and Community Physician). o A consistent patient navigator/case manager to support the patient and health care providers once patient discharged. o Medication reconciliation and polypharmacy to occur at transfer and at transitions in patient status. o Facilitate patient ownership of their medication profile. o Revision of the prescription form at hospital to include a tick box to identify when medications are needed for blister packing. 17 o As part of discharge planning standards, to include standards around turnaround time for community pharmacists to complete medication orders. o Provide education to health care providers and physicians on community resources available and types of residential care. In addition, it would be appropriate to distribute the information learned with other working groups established for follow up. For example, Meditech access issues could be related to education and training and can be raised with IMIT. N Neexxtt SStteeppss It is important that over the next two months, testing and evaluating solutions occurs. Next steps include prioritizing the opportunities identified, confirming what work may be in process to avoid duplication, and beginning small tests of change through multiple PDSA cycles. 18