Collaborating organizations and key contact
advertisement
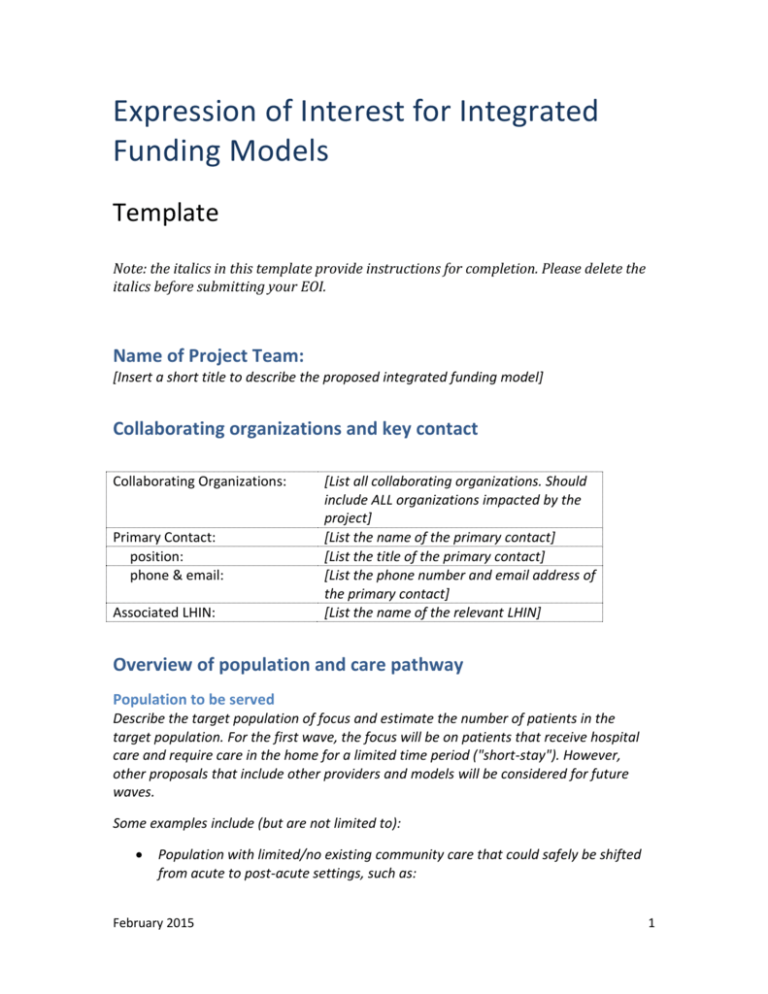
Expression of Interest for Integrated Funding Models Template Note: the italics in this template provide instructions for completion. Please delete the italics before submitting your EOI. Name of Project Team: [Insert a short title to describe the proposed integrated funding model] Collaborating organizations and key contact Collaborating Organizations: Primary Contact: position: phone & email: Associated LHIN: [List all collaborating organizations. Should include ALL organizations impacted by the project] [List the name of the primary contact] [List the title of the primary contact] [List the phone number and email address of the primary contact] [List the name of the relevant LHIN] Overview of population and care pathway Population to be served Describe the target population of focus and estimate the number of patients in the target population. For the first wave, the focus will be on patients that receive hospital care and require care in the home for a limited time period ("short-stay"). However, other proposals that include other providers and models will be considered for future waves. Some examples include (but are not limited to): Population with limited/no existing community care that could safely be shifted from acute to post-acute settings, such as: February 2015 1 o Patients who are admitted for stroke and require home care for 60 days following hospital discharge o Chronic Diseases such as COPD or CHF with patients at high risk for readmission Current care pathway Describe the existing care pathway(s) (e.g., current pathway(s) patients in the target population would experience, from hospital admission/discharge to assessment for postacute care, to intake and discharge from post-acute care). Provide baseline data for the target population going through the current care pathway(s), using indicators of health outcomes, health care utilization, etc. Please include comparisons to evidence-based benchmarks for the indicators. Examples of indicators include: Hospital readmission rates ED visits Hospital length of stay ALC Patient experience Wait time for home care services Primary care visit within 7 days of discharge Medication reconciliation at discharge Case Costing Opportunities for improvement Describe (at a high level – more details to be included below) the proposed care pathway(s) and how it differs from the current state (NOTE: Teams will be assessed on readiness to implement their care pathway(s), but care pathway(s) do not need to be at the implementation stage to be considered). Key commitments 1. Service delivery model Describe the proposed service delivery model, including: a. The types of services included in the care pathway(s). b. How patients’ assessment of care needs will be determined. c. How the target population will be defined for inclusion in the project. d. How each patient’s single care plan will be developed, monitored, and evaluated in partnership with the team, patient, and family. February 2015 2 e. How the discharge process from each involved sector will be conducted. f. How patients will be transitioned to appropriate long-term community-based care as-needed (e.g., ensuring that patients with chronic diseases are not excluded). g. How the new approach is in accordance with regulatory/legislative requirements OR how current legislation might be challenged by the new approach. h. What is the geographic distribution of the target population. 2. Integrated payment Provide details of how existing base funding across providers (such as hospitals, CCACs, direct service home care providers, physicians, and others) will be leveraged for service delivery. Describe the plan to transition to integrated funding once an integrated care process has been established. 3. Patient/Family engagement Describe the plan to engage patients and families in the process of developing, implementing, and evaluating the project. Describe how patients’ preferences and participation in planning of services will be accounted for and measured. 4. Commitment to evaluation and continuous quality improvement a. By checking the box below, we agree to participate in, and support, a central evaluation of the project. This includes willingness to amend elements of the intervention design to accommodate the evaluation and using quality improvement supports and frameworks to support change management. ☐ b. By checking the box below, we agree to provide and/or review data as part of the central evaluation, including: Quality indicators, including patient experience surveys Individual-level data to track which patient received which services (including a plan to obtain patient consent on data linkage for the purpose of provincial evaluation) Patient-reported outcome measures Home care activity and assessment Case costing data, where applicable Discharge Abstract Database (DAD), National Ambulatory Care Reporting System (NACRS) February 2015 3 ☐ c. By checking the box below, we agree to participate in knowledge translation with other sites, including participation in a Community of Practice. ☐ 5. Implementation and outcomes Project Implementation Describe how you intend to implement your project, including goals, deliverables, and timelines. Please provide a contingency plan including risk and mitigation tactics. Roles and Responsibilities Describe the roles and responsibilities of all participating providers. Measurement of Outcomes Describe your plan to measure progress (e.g., rate of implementation, success of patient recruitment, degree of care and payment integration across sectors), process (e.g., type and volume of services provided to patients at individual-level) and outcomes (e.g., use of standardized measures and outcomes including hospital readmission, ED visits, hospital length of stay, ALC length of stay, patient experience, etc.). Resource plan Budget Provide a budget, indicating anticipated project-related expenditures (Note: It is expected that annual (one-time) project-related costs will be approximately $175,000 per team. This project will not pay for direct service delivery, including case management and care coordination services. Direct service delivery costs will be drawn from existing funding among the organizations participating, i.e. no net new funds will be provided). It is expected that term of the agreements will be a maximum 36 months. Sustainability Please describe the plan to ensure the project can continue beyond the funding period. February 2015 4 Capacity, governance, and buy-in Capacity Please describe the team’s current experience with integration initiatives (e.g., how experience can be leveraged). Please describe the team’s current experience with quality improvement methodologies (e.g., participation in IDEAS, LEAN, IHI, etc.). Governance Please describe how the respective boards and quality committees of participating organizations have been involved and engaged in the development of this proposal. Stakeholder commitment Describe key stakeholder support for integrated pathway development and/or implementation, including: physician leads, clinical leadership, most relevant clinicians, and other providers that are not directly involved but may be impacted by the project. Sign-off ☐ The LHIN supports this EOI for further consideration (e.g. readiness assessment) and has consulted with relevant stakeholders (e.g. CCAC and CSS) The following team members endorse this Expression of Interest: Name of team member Title Affiliated organization name and address Signature [Provide information on the primary contact] [Provide information on the CEO/Executive Director and Board Chair from each organization affected by the project] [Templates must be submitted to IFM@ontario.ca by March 18, 2015.] February 2015 5