Open Access version via Utrecht University Repository
advertisement
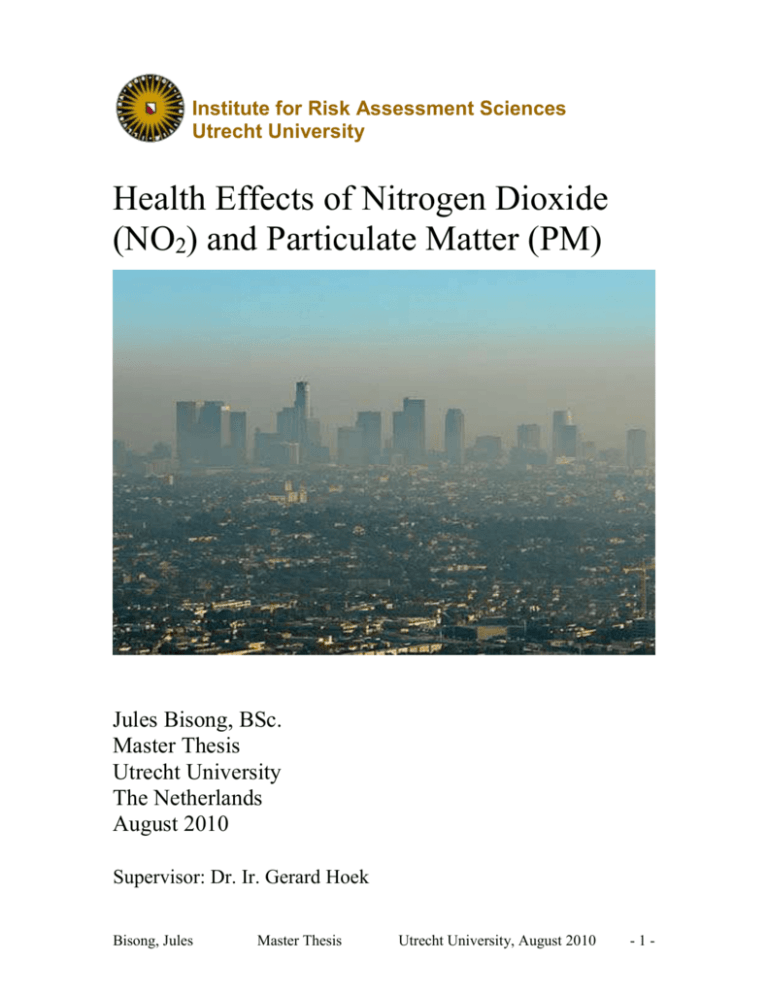
Institute for Risk Assessment Sciences Utrecht University Health Effects of Nitrogen Dioxide (NO2) and Particulate Matter (PM) Jules Bisong, BSc. Master Thesis Utrecht University The Netherlands August 2010 Supervisor: Dr. Ir. Gerard Hoek Bisong, Jules Master Thesis Utrecht University, August 2010 -1- Contents: Page Abstract 3 Introduction 4 Relevance of Thesis Topic 5 Sources of NO2 and PM 7 Health Effects of NO2 9 Health Effects of PM 12 Risk Groups 15 Conclusion 17 References 18 Bisong, Jules Master Thesis Utrecht University, August 2010 -2- Abstract: This thesis outlines the health effects of air pollutants such as NO 2 and PM. They involve a variety of diseases like asthma, heart disease, lung disease, and allergies. The pollutants are from various sources, including the combustion of fossil fuel from motor vehicles, and other dust-generating processes, such as construction and demolition. Certain individuals, such as asthmatics, people with compromised immunity, etc, are included in the risk groups for diseases caused by NO2 and PM. Bisong, Jules Master Thesis Utrecht University, August 2010 -3- Introduction: Nitrogen dioxide (NO2) and particulate matter (PM) are among the most investigated air pollutants. Many epidemiological studies have been carried out to pinpoint possible links between these pollutants and diseases. Asthma, cardiopulmonary disease, and allergies are among the most important diseases associated with the pollutants (Koren (1995); Delfino et al. (2006); Bhaskaran et al. (2009). Sulfur dioxide (SO2) used to be of interest too, but recently, its concentration has reduced and the focus is now on NO2 and PM (Bernard et al. n.d.). The most important sources of these pollutants include fossil fuel combustion, e.g. from motor vehicles, trains, boats and industrial processes, gas stoves and heaters, etc, and from dust-generating processes such as construction and demolition of buildings, roads, bridges, etc (Bernard et al. n.d.). Current EU limits for the Netherlands are as follows: 40 µg/m3 for the annual average NO2 concentration, to be met by 2010, and 50 µg/m3 for the daily average PM10 concentration, not to be exceeded more often than 35 times a year, from 2005 onwards (Velders and Matthijsen, 2009). The burden of the diseases caused by these pollutants is a public health issue and measures need to be taken to address it. It may be possible that certain groups of people are more at risk of contracting air pollution-related diseases, but this is unlikely the usual case, as air pollution is a global problem. Polluted air in one part of the world or one part of a country or even a city can quickly travel to other parts (Reuther, 2000). A detailed outline of the diseases and their mechanisms of action is given in the following sections of this thesis. Bisong, Jules Master Thesis Utrecht University, August 2010 -4- Relevance of Thesis Topic: The relevance of researching the health effects of NO2 and PM is seen in the various associations made between exposure to these substances and disease. NO2 is one of the major pollutants in heavily populated areas, with ambient air levels normally in order of 10 to 50 µg/m3 (Bernard et al. n.d.). In pollution hot spots, such as tunnels or street canyons, this concentration may reach 100 µg/m3 as a 1-hour average during high pollution episodes (Bernard et al. n.d.). NO2 has not been proven to be a major health risk. However, it reacts with components in the fluid lining the respiratory tract (Bernard et al. n.d.). It has also been found to have the capacity to activate oxidant pathways, in in vitro animal and human studies (Brunekreef & Holgate, 2002). Asthmatic individuals are more vulnerable to its effects, which include narrowing of the airways and increased responsiveness to irritants and allergens (Bernard et al. n.d.). Since it occurs in a mix of other gases, its concentration can give insight into that of the other gases which have been proven to be harmful to health. It is therefore a proxy to other known disease-causing gasses. A human adult inhales 20 m3 PM per day, and this means a handful of particles can be deposited in the airway epithelium, especially in heavily polluted areas, where particle concentration may reach 50 µg/m3 (Baeza-Squiban et al, 1999). However, particle size and aerodynamic diameter determine the level of deposition (Baeza-Squiban et al, 1999). The respiratory system has defence mechanisms, such as the mucociliary lining the epithelium, which sweep these particles away (upward) from the respiratory tract to the throat, where they are swallowed and digested in the stomach, or sneezed out through the nasal tract (Baeza-Squiban et al, 1999). There are also macrophages in the alveoli, which engulf these particles by endocytosis (Baeza-Squiban et al, 1999). However, clearance by endocytosis can be overwhelmed, leading to a longer duration of particles in the airway, which creates contact between the particles and the epithelium, which in turn, can cause cellular damage (Baeza-Squiban et al, 1999). It is worthy of note that, although macrophages engulf particles, the fate of the latter is unknown (BaezaSquiban et al, 1999). Epidemiological studies have associated increased cardiopulmonary mortality and hospital admissions with episodes of high particulate air pollution (BaezaSquiban et al, 1999). An AIRNET report of Work Group 2 associated short-term Bisong, Jules Master Thesis Utrecht University, August 2010 -5- increases in PM air pollution with increased daily mortality and hospital admissions for respiratory and cardiovascular disease. The report also suggests that daily exposure to polycyclic aromatic hydrocarbons (PAH) may in addition to causing cancer, have effects on foetuses and infants. Moreover, there is a correlation between increases in allergic asthma, nasal allergies, and chronic bronchitis with increased levels of airborne particles (Baeza-Squiban et al, 1999). Thus, more awareness of the health impacts of these airborne particles is important and can motivate the setting up of standards for emission control beneficial to health. Also, it can stimulate more mapping of high-concentration zones, so that structural measures, such as re-location of industries or transportation networks can be taken in order to limit the level of pollution. Although it is not exactly clear what concentration of these substances is not harmful to health, which means any concentration could be harmful, it would be, however, useful to know the concentration at a particular place and at a particular time. This would aid epidemiological research, for instance, in finding a link between disease and an air pollutant, as with time-series studies. Bisong, Jules Master Thesis Utrecht University, August 2010 -6- Sources of NO2 and PM: Natural sources of NO2 include biological processes in soil and the atmospheric oxidation of ammonia (DEQ, 2003. Anthropogenic (man-made) sources include high-temperature fuel combustion in motor vehicles and in industrial and utility boilers (EICB, n.d.). NO2 is produced from gas stoves, and other domestic combustion processes, such as butane gas heaters (EICB, n.d.). These sources are more important because they are concentrated in the more populated areas and account for the greater share of the NO2 emissions in such areas (Bernard et al., n.d.). PM on the other hand, also referred to as fine particles, includes finely divided solids or liquids such as dust, fly ash, soot, smoke, fumes, mists and condensing vapours that can be suspended in the air or gas for extended periods of time (EICB, n.d.). Primary sources of PM include both natural and anthropogenic sources and the latter include agricultural operations, industrial processes, combustion of wood and fossil fuels, construction and demolition activities, and entrainment of road dust into the air (EICB, n.d.; Bernard et al., n.d.). Natural sources include windblown dust and soot (EICB, n.d.). Secondary sources of PM directly emit air contaminants into the atmosphere that form or contribute to the formation of PM (EICB, n.d.; Bernard et al., n.d.). These pollutants are therefore considered precursors to PM formation. The secondary pollutants include oxides of sulfur (SOx), oxides of nitrogen (NOx), volatile organic compounds (VOCs), and ammonia (NH3) (EICB, n.d.). The figure below illustrates the various sources of PM. Bisong, Jules Master Thesis Utrecht University, August 2010 -7- Figure 1: Possible Sources of PM (Polichetti et al., 2009) Bisong, Jules Master Thesis Utrecht University, August 2010 -8- Health Effects of NO2: Primary health problems associated with NO2 are acute pulmonary function responses, acute respiratory infectious disease and chronic lung disease (Hodgkins et al., 2010; McKee and Rodriguez, 1993). NO2 can act as an adjuvant, thereby allowing for allergic sensitization to an innocuous inhaled antigen and the generation of an antigen-specific Th2 immune response manifesting in an allergic asthma phenotype (Hodgkins et al., 2010). This occurs through NO2 exposure, which causes pulmonary CD11c+ cells to acquire a phenotype capable of increased antigen uptake, migration to the draining lymph node, expression of MHCII and co-stimulatory molecules required to activate naïve T cells, and secretion of polarizing cytokines to shape a Th2/Th17 response (Hodgkins et al., 2010). Some asthmatics experience increased airway response as a result of NO2 exposure (McKee and Rodriguez, 1993). Young children have been found to have increased acute respiratory illnesses (McKee and Rodriguez, 1993). Also, individuals who exercise in places with NO2, exposed to indoor NO2 sources, or are concurrently exposed to other pollutants, have been found to have increased risk of respiratory illnesses (McKee and Rodriguez, 1993). Acute exposure to less than 1 ppm NO2 (typical outdoor ambient levels) does not seem to affect pulmonary function in healthy, normal individuals (McKee and Rodriguez, 1993). This suggests that the respiratory health effects of NO2 are only experienced after long-term exposure. According to epidemiological studies, there is a relation between long-term NO2 exposure and an increase in respiratory illness (McKee and Rodriguez, 1993). This relation is supported by human and animal studies which indicate that NO2 can cause alterations of host immunity and result in increased susceptibility to viral and bacterial pulmonary infections (McKee and Rodriguez, 1993). Animal studies can be used to draw conclusions on humans in relation to NO2 exposure and pulmonary disease because humans share the same pulmonary defense mechanisms with animals (mammals) (McKee and Rodriguez, 1993). Animal studies show that NO2 causes structural alterations in the ciliated cells of the mucociliary escalator (McKee and Rodriguez, 1993). The alveolar macrophage is the primary host defense affected by acute, long-term NO2 exposure (McKee and Rodriguez, Bisong, Jules Master Thesis Utrecht University, August 2010 -9- 1993). The effects include: decrease in bactericidal and viricidal activity; decrease in the production of a radical involved in bactericidal activity; decrease in phagocytosis; morphological and metabolic changes; and other functional changes (McKee and Rodriguez, 1993; Nitschke et al., 1999). These effects were shown by most studies at exposure levels between 1 and 5 ppm (McKee and Rodriguez, 1993). Other studies showed effects such as suppression of T and B cell responsiveness to mitogens, decrease in the number of T cells, and suppression of primary antibody responsiveness, in animals (McKee and Rodriguez, 1993). Air pollution, it should be noted, is not only an external problem. Many people are affected by internal sources too. A study by Kawamoto et al. (1993) measured personal exposure to indoor NO2 sources in students using filter badges attached to their chests or collars, for 1 week. The urinary hydroxyproline/creatinine ratio (HOP/C) was examined as a biomarker for health effects. Outdoor NO2 concentration during the study period was 13.5 – 13.7 µg/m3, whereas indoor concentration was 219 µg/m3 for students using a kerosene heater and 474 µg/m3 for students using an oil fan heater. Smoking and the use of electric heaters did not influence exposure to NO2. The correlation between the period of cooking and personal exposure was also observed, with NO2 levels being 290 µg/m3. Neither smoking nor NO2 exposure where found to cause an increase in urinary HOP/C. This could be due to the very short exposure time. The non increase does not mean that there were no health effects. A week may just have been too short to detect any changes. The important thing to grasp here is that, there is that much increase in exposure when we do not use environmentally-friendly technology. This gives insight into how easily health effects can occur. Beckett et al. (1995) carried out a study to investigate the effects of nitrous acid on lung function in asthmatics. Nitrous acid is a primary product of combustion and may also be a secondary product when NO2 reacts with water, in this case, in the linings of the lungs. In the double-blinded crossover chamber exposure study, researchers exposed 11 mildly asthmatic adult subjects for 3 hours to 650 ppb nitrous acid and to filtered room air with three 20-minute episodes of moderate cycle exercise. Symptoms, respiratory parameters during exercise, and spirometry after exercise were measured. Statistically, there was a significant decrease in forced vital capacity on days when subjects were exposed to Bisong, Jules Master Thesis Utrecht University, August 2010 - 10 - nitrous acid. Aggregate respiratory and mucous membrane symptoms were also significantly higher when exposed to nitrous acid. Thus, the concentration and duration of exposure to nitrous acid altered lung mechanics slightly and produced mild irritant symptoms in asthmatics. It may be confusing, however, to find that some studies dispute the health effects attributed to NO2. For example, in the PATY study by Pattenden et al (2006), NO2 was not linked to the health effects mentioned earlier. It was rather associated with very few effects, such as indirect contribution to inhalation allergies. Therefore, bronchitis or asthma were not caused by NO2, according to the study. That notwithstanding, NO2 was ruled as a possible indicator of traffic related air pollutants, which refers us to earlier sections of this thesis, in which NO2 is mentioned to be an indicator of other air pollutants. What stands firm is that NO2, be it a direct or indirect cause of respiratory diseases, is a good indicator of the concentration of other pollutants that may be more directly associated with respiratory diseases. Bisong, Jules Master Thesis Utrecht University, August 2010 - 11 - Health Effects of PM: There are more studies carried out to investigate the health effects of PM. The mechanisms by which PM affects human health are more understood than those of NO2. Meng and Zhang (2006), investigated in vitro toxicological effects of PM2.5 suspensions, their water-soluble fractions and solvent-extractable organics from dust storm on the viability and DNA of rat alveolar macrophages and in vivo toxicological effects of PM2.5 suspensions on DNA of lung cells of rats. In their results, they found that in vitro, PM2.5 suspensions, their water-soluble fraction and solvent-extractable organics from both dust storm and normal weather caused a decrease of the cell viability and an increase of DNA damage of rat alveolar macrophages in a dose-response manner. In vivo, PM2.5 from both dust storm and normal weather caused an increase of DNA damage of rat lung cells in a dose-response manner. How exactly, PM and other pollutants affect health can only be seen in in vivo and in vitro toxicological studies. It may not be easy to determine what parts of PM cause what types of health effect, using epidemiological studies. It is in light of this, that different effects can be seen from the same pollutant, but of different sources. For example, toxicological studies have shown that source influences the toxicity of particles in in vivo and in vitro models (Gordon, 2007). Adverse lung changes observed in rats instilled with ambient PM from different cities were dependent on the urban or rural environment in which the particles were collected (Costa and Dreher, 1997). Gavett et al. (2003) also found significant differences in the effects on rodents treated with PM collected from two German cities. They found ambient particles from the industrial city of Hettstedt to have more potential in causing allergic asthma than those collected from the agricultural and administrative centre of Zerbst. On the other hand, toxicological studies show health effects of exposure only at much higher than ambient levels (Schlesinger, 2000). Therefore, both toxicological and epidemiological approaches to finding links between exposure and disease should be employed. Toxicological evidence can be used to support epidemiological evidence if necessary. Epidemiological studies have shown associations between PM exposure and cardiopulmonary health outcomes (Heal et al. 2009). However, this study by Heal et al. (2009) was aimed at finding whether the water-soluble and extractable metal content in PM was responsible for Bisong, Jules Master Thesis Utrecht University, August 2010 - 12 - cardiopulmonary health effects. Their findings did not show any significant association between the metal content alone and the health effects. Other researchers, though, hold that metals in PM generate oxidative stress (Li et al, 2008). Mehta et al. (2008) found that transition metals such as nickel and chromium, and oxidative stress-induced lipid peroxidation metabolites such as aldehydes can greatly inhibit nucleotide excision repair (NER) and enhance carcinogen-induced mutations. They also tested the effect of PM on DNA repair capacity in cultured human lung cells using in vitro DNA repair synthesis and host cell reactivation assays. Their findings show that PM greatly inhibits NER for ultraviolet (UV) light and benzo(a)pyrene diol epoxide (BPDE)-induced DNA damage in human lung cells. Furthermore, they demonstrated that PM exposure can significantly increase both spontaneous and UV-induced mutagenesis. They also suggest from their results that the carcinogenicity of PM may act through its combined effect on suppression of DNA repair and enhancement of DNA replication errors. The principal health effect of PM on the pulmonary system is the exacerbation of inflammation and this is especially the case with susceptible individuals (Li et al, 2008). A mechanism by which it occurs is the generation of oxidative stress by its chemical compounds and metals (Li et al, 2008). Cells respond to this oxidative stress by activating oxidant defense, inflammation, and toxicity (Li et al, 2008). In the lung, proinflammation by PM causes increased cytokine/chemokine production and adhesion molecule expression (Li et al, 2008). It has also been found that ambient PM can act as an adjuvant for allergic sensitization, which suggests that long-term PM exposure may lead to increased prevalence of asthma (Li et al, 2008). Short-term increases in PM concentration are associated with increased daily mortality and hospital admissions for respiratory and cardiovascular disease (Downs et al. n.d.). However, long-term effects may have more health impact than short-term effects (Downs et al. n.d.). It is not easy, though, to determine whether a health effect is a result of short-term and/or long-term exposure because the effect of an acute exposure to PM could easily be superimposed to that of a chronic exposure (Polichetti et al., 2009). Increased mortality risks seem to be more attributed to anthropogenic (e.g. from motorvehicle emissions) than to natural PM sources (Downs et al. n.d.). Many studies attribute the larger part of PM toxicity to its smaller fractions, that is, fine and ultrafine particles (Polichetti et al., 2009). However, considerations need to be made on the fact that these Bisong, Jules Master Thesis Utrecht University, August 2010 - 13 - size fractions make up part of the internal constituents of PM10. Freitas et al. (2010) found statistically significant (p < 0.001) associations between atmospheric levels of PM10 and hospital admissions due to respiratory conditions in a study carried out in Lisbon. In their review, Brunekreef and Holgate (2002) associated PM exposure with increased mortality and hospital admissions for respiratory and cardiovascular diseases. The effects were found in short-term studies relating day-to-day variations in air pollution and health, and long-term studies in which cohorts of exposed individuals were followed over time (Brunekreef and Holgate, 2002). Since effects were found at very low exposure levels, it is unclear whether a threshold at which there is no effect exists (Brunekreef and Holgate, 2002). A WHO 2008 health quality report asserts that PM affects more people than any other pollutant and its effects occur at exposure levels currently experienced by most urban and rural populations in both developed and developing countries (WHO, 2008). Long-term PM exposure contributes to the risk of developing cardiovascular and respiratory diseases, as well as lung cancer (WHO, 2008). Some health effects of PM exposure in developing countries include increased risk of acute lower respiratory infections and associated mortality among young children (WHO, 2008). Other effects include increased risk of chronic obstructive pulmonary disease and lung cancer among adults (WHO, 2008). The occurrence of these health effects in developing countries is attributed to indoor combustion of solid fuels on open fires or traditional stoves (WHO, 2008). Cities with high levels of pollution show 15-20 % more mortality than relatively cleaner cities (WHO, 2008). Average life expectancy in the EU is 8.6 months lower, due to exposure to PM from anthropogenic sources (WHO, 2008). Bisong, Jules Master Thesis Utrecht University, August 2010 - 14 - Risk Groups: The effects of air pollution are widespread and indiscriminate. However, variations in human behaviour may make them manifest with different levels of severity; some affected individuals experience severe effects, while others only mild effects. Other factors that make some people more susceptible to the effects of air pollution are age, asthma, exercise in the presence of a pollutant (McKee and Rodriguez, 1993). Children and the elderly have less immunity and are therefore more vulnerable (McKee and Rodriguez, 1993). People with compromised immunity (e.g. AIDS patients) also have a higher risk of suffering from the effects of air pollution McKee and Rodriguez, 1993). Some of the effects these risk groups are likely to suffer include acute symptoms and lung function impairment, increased susceptibility to acute respiratory infection, and possibly conditions leading to chronic long disease (McKee and Rodriguez, 1993). Pope (2000), though, explains that it is difficult to draw a straight line between who is at risk and who is not. He further distinguishes risk groups into short term, acute exposure risk group and long term, chronic exposure risk group. In this view, the short term risk group comprises those whose condition would be worsened (mortality) by an episode of acute exposure, such as in the 1952 London smog. They include the elderly, the very young, persons with chronic cardiopulmonary disease, influenza or asthma (Pope, 2000). However, recent research has showed that these persons may not be the only ones to be included in the group (Pope, 2000). Study data from Philadelphia and Pennsylvania suggest that mortality for many may be advanced substantially, rather than by just a few days or weeks, as in cases of mortality by acute exposure (Pope, 2000). The data also suggest that those at increased risk of mortality from acutely elevated exposure may include more than just the most old and frail who are already very near death (Pope, 2000). The long term group, on the other hand, comprises every exposed person. There is no evidence that mortality due to cumulative exposure is unique to a particular group (Pope, 2000). Therefore, adults, children, diseased and healthy people are all susceptible to mortality from chronic exposure. However, since the relative risk is small, the long term cumulative effects are most likely to be observed in older people with relatively higher baseline risks of mortality (Pope, 2000). Bisong, Jules Master Thesis Utrecht University, August 2010 - 15 - It is sometimes suggested that socioeconomic status (SES) is a determinant of susceptibility to the effects of air pollution. Some examples used in making such suggestions include the installation of refuse disposal facilities in low income neighbourhoods, garbage disposal jobs by low income earners, the use of inefficient technology (home appliances like gas stoves, heaters, etc), etc. In a study, though, Charafeddine and Boden (2007) investigated whether income inequality may modify the association between fine particulate pollution and self-reported health. They found that the odds of reporting fair or poor health for a 10 µg/m3 increase in particulate pollution is 1.34 (95% confidence interval 1.21 – 1.48) when income inequality is low. The similar odds ratio for higher income inequality is 1.11 (95% confidence interval 1.06 – 1.16) (Charafeddine and Boden, 2007). Income inequality was therefore found to be an effect modifier of the association between general self-reported health and particulate pollution (Charafeddine and Boden, 2007). The researchers also say that these findings contradict their hypothesis that people living in higher income inequality areas are more vulnerable to the impact of air pollution. Note that information for this study was self-reported, which does not rule out the possibility of recall bias. Burra et al (2009) investigated socioeconomic variation in ambulatory physician consultations for asthma and assessed possible effect modification of SES on the association between physician visits and air pollution for children aged 1 – 17 and adults aged 18 – 64 in Toronto, Canada, between 1992 and 2001. In their results, they found a socioeconomic gradient in the number of physician visits among children and adults and both sexes. SO2, NO2 and PM2.5 had positive associations with physician visits and the risk ratios for the low socioeconomic group were significantly greater than those for the high socioeconomic group in many of the models of SO2 and PM2.5. Bisong, Jules Master Thesis Utrecht University, August 2010 - 16 - Conclusion: Air pollution causes respiratory, cardiovascular and other diseases. It has also been associated with increased hospital admissions and mortality in young children and adults. Sources of NO2 and PM include fossil fuel combustion, dust-generating activities, such as construction and demolition, amongst others. Individuals with Asthma, compromised immunity, etc, are particularly at higher risk of experiencing health effects of pollution. Developing countries experience significant air pollution-related health effects, due to indoor solid fuel combustion in open fires. The reduction of average life expectancy in the EU is one of the effects of PM-related air pollution. Bisong, Jules Master Thesis Utrecht University, August 2010 - 17 - References: Koren, H. S. (1995). Associations between Criteria Air Pollutants and Asthma. Environ Health Perspect. 103 (Suppl 6): 235 – 242. Delfino, R. J. et al. (2006). Personal and Ambient Air Pollution is Associated with Increased Exhaled Nitric Oxide in Children with Asthma. Environmental Health Perspectives. Vol. 114, No. 11. Bhaskaran, K. et al. (2009). Effects of air pollution on the incidence myocardial infarction. Heart. 95: 1746 – 1759. doi:10.1136/hrt.2009.175018. Bernard, A. et al. (n.d.). Air pollution and the risks to human health: a toxicological perspective. AIRNET Work Group 3. p.p. 1 – 75 Reuther, C. G. (2000). Winds of Change: Reducing Transboundary Air Pollutants. Environmental Health Perspectives. Vol. 108. No. 4. Brunekreef, B. and Holgate, S.T. (2002). Air pollution and health. The Lancet, 360: 1233 – 42. Baeza-Squiban, A. et al. (1999). Airborne particles evoke an inflammatory response in human airway epithelium. Activation of transcription factors. Cell Biology and Toxicology. 15: 375 – 380 EICB (n.d.). Wat is stikstofdioxide? http://www.informatie.binnenvaart.nl/milieu/216.html DEQ (2003). Nitrogen Dioxide. http://www.deq.state.ok.us/factsheets/air/no2.pdf Polichetti, G. et al. (2009). Effects of particulate matter (PM10, PM2.5 and PM1) on the cardiovascular system. Toxicology. 261: 1 – 8. Hodgkins, S.R. et al. (2010). Inhalation of NO2 induces maturation of pulmonary CD11c+ cells that promote antigenspecific CD4+ T cell polarization. Respiratory Research. 11: 102. McKee, D.J. & Rodriguez, R.M. (1993). Health Effects Associated with Ozone and Nitrogen Dioxide Exposure. Water, Air, and Soil Pollution. 67: 11 – 35 Nitschke, M. et al. (1999). Respiratory health effects of nitrogen dioxide exposure and current guidelines. International Journal of Environmental Health Research. 9: 39 – 53. Kawamoto, T. et al. (1993). Personal Exposure to Nitrogen Dioxide from Indoor Heaters and Cooking Stoves. Arch. Environ. Contam. Toxicol. 25: 534 – 538 Bisong, Jules Master Thesis Utrecht University, August 2010 - 18 - Beckett, W.S. et al. (1995). Effects of Nitrous Acid on Lung Function in Asthmatics: A chamber Study. Environmental Health Perspectives. Vol. 103, No. 4 Pattenden, S. et al. (2006). NO2 and children’s respiratory symptoms in the PATY study. Occup Environ Med. 63: 828 – 835. Meng, Z. and Zhang, Q. (2007). Damage effects of dust storm PM2.5 on DNA in alveolar macrophages and lung cells of rats. Food and Chemical Toxicology. 45: 1368 – 1374. Gordon, T. (2007). Linking Health Effects to PM Components, Size, and Sources. Inhalation Toxicology. 19(suppl. 1): 3 – 6. Costa, D.L. and Deher, K.L. (1997). Bioavailable transition metals in particulate matter mediate cardiopulmonary injury in healthy and compromised animal models. Environmental. Health Perspectives. 105 (Supplement 5): 1053 – 1056. Gavett, S.H. et al. (2003). Metal composition of ambient PM2.5 influences severity of allergic airways disease in mice. Environmental Health Perspectives. 111: 1471 – 1477. Schlesinger, R.B. (2000). Properties of ambient PM Responsible for Human Health Effects: Coherence Between Epidemiology and Toxicology. Inhalation Toxicology. 12 (Supplement 1); 23 – 25. Heal, M.R. et al. (2009). A time series study of the health effects of water-soluble and total-extractable metal content of airborne particulate matter. Occup Environ Med. 66: 636 – 638. Li, N., Xia, T., and Nel, A.E. (2008). The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radical Biology & medicine. 44: 1689 – 1699. Mehta, M. et al. (2008). Particulate matter inhibits DNA repair and enhances mutagenesis. Mutation Research. 657: 116 – 121. Downs, S. et al. (n.d.). Air pollution and the risks to human health: Epidemiology. AIRNET Work Group 2. p.p. 1 – 61. Freitas, M.C. et al. (2010). Effect of particulate matter, atmospheric gases, temperature, and humidity on respiratory and circulatory diseases’ trends in Lisbon, Portugal. Environ Monit Assess. 162: 113 – 121. Pope, C. A. (2000). Epidemiology of Fine Particulate Air Pollution and Human Health: Biologic Mechanisms and Who’s at Risk? Environmental Health Perspectives. Vol. 108, Supplement 4. Bisong, Jules Master Thesis Utrecht University, August 2010 - 19 - Charafeddine, R. and Boden, L.I. (2007). Does income inequality modify the association between air pollution and health? Environmental Research. 106: 81 – 88. Velders, G.J.M. and Matthijsen, J. (2009). Meteorological variability in NO2 and PM10 concentrations in the Netherlands and its relation with EU limit values. Atmospheric Environment. 43: 3858 – 3866 WHO (2008). Air quality and health. Fact http://www.who.int/mediacentre/factsheets/fs313/en/ Bisong, Jules Master Thesis sheet Utrecht University, August 2010 N° - 20 - 313.