Falls prevention policy - Minnesota Hospital Association
advertisement
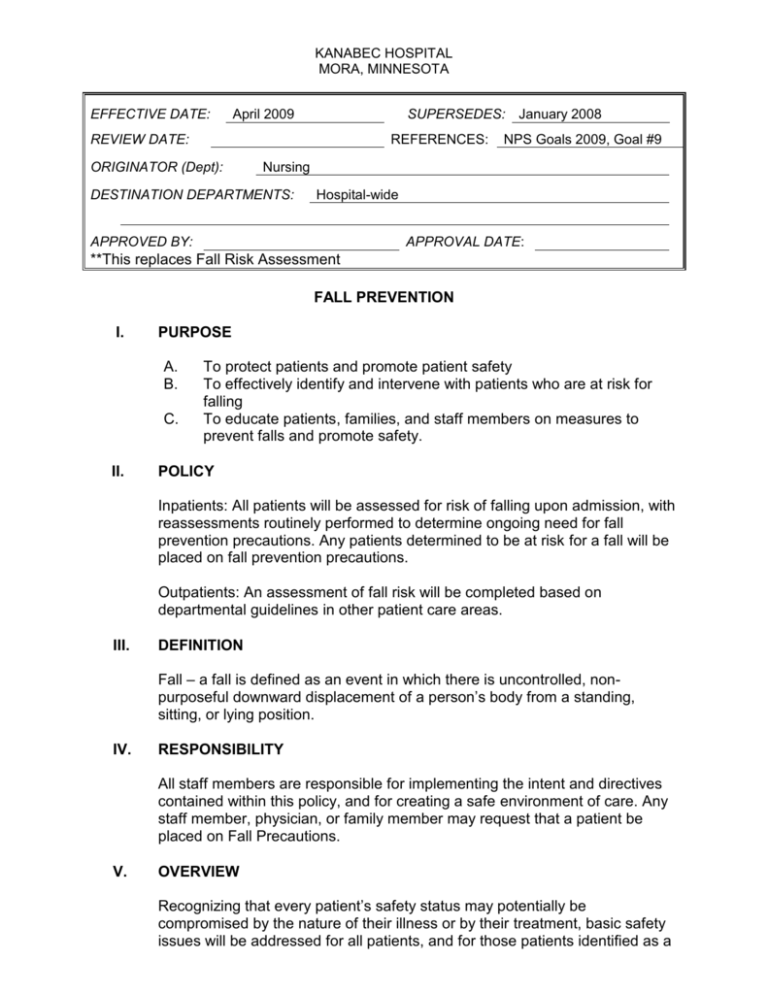
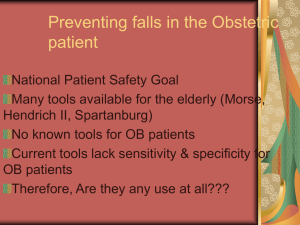
KANABEC HOSPITAL MORA, MINNESOTA EFFECTIVE DATE: April 2009 SUPERSEDES: January 2008 REVIEW DATE: REFERENCES: ORIGINATOR (Dept): NPS Goals 2009, Goal #9 Nursing DESTINATION DEPARTMENTS: Hospital-wide APPROVED BY: APPROVAL DATE: **This replaces Fall Risk Assessment FALL PREVENTION I. PURPOSE A. B. C. II. To protect patients and promote patient safety To effectively identify and intervene with patients who are at risk for falling To educate patients, families, and staff members on measures to prevent falls and promote safety. POLICY Inpatients: All patients will be assessed for risk of falling upon admission, with reassessments routinely performed to determine ongoing need for fall prevention precautions. Any patients determined to be at risk for a fall will be placed on fall prevention precautions. Outpatients: An assessment of fall risk will be completed based on departmental guidelines in other patient care areas. III. DEFINITION Fall – a fall is defined as an event in which there is uncontrolled, nonpurposeful downward displacement of a person’s body from a standing, sitting, or lying position. IV. RESPONSIBILITY All staff members are responsible for implementing the intent and directives contained within this policy, and for creating a safe environment of care. Any staff member, physician, or family member may request that a patient be placed on Fall Precautions. V. OVERVIEW Recognizing that every patient’s safety status may potentially be compromised by the nature of their illness or by their treatment, basic safety issues will be addressed for all patients, and for those patients identified as a 2 Fall Prevention Policy higher level of risk, more in-depth prevention interventions will be implemented. VI. PROCEDURE A. Inpatient Fall Prevention 1. Inpatients will be assessed on admission and every shift thereafter. Specific guidelines are implemented for OB, pediatric, and post-operative orthopedic patients. 2. Fall risk screening will be completed by an RN or LPN. The RN is responsible for establishing and updating the individual plan of care related to safety and fall prevention. 3. All interventions will be documented in the medical record. 4. Family, if available, will be consulted for individualizing fall prevention interventions. B. Upon admission 1. Complete the Fall Risk Data Collection Intervention. 2. If the patient’s score is ≥ 7, or at the nurse’s discretion, initiate Fall Precautions. a. Write Fall Precautions on patient grease board in room. b. Apply yellow Fall Precautions armband on patient. c. Place Fall Precautions label on Kardex. d. Initiate appropriate interventions to minimize the patient’s risk of falling. e. Identify appropriate interventions on patient’s care plan. C. Ongoing risk assessment 1. Complete the Fall Risk Reevaluation with patient assessment every shift and with a change in patient condition. 2. If patient condition/score changes, or at the nurse’s discretion, Fall Precautions may be initiated or discontinued. 3. All patients who have had a lower extremity nerve block anesthetic will be automatically placed on Fall Precautions until the nerve block is discontinued. The patient will then be reevaluated to determine his/her fall risk. D. If a patient experiences a fall: 1. Document what occurred in the nurse’s progress notes including: patient appearance at time of discovery, patient response to event, evidence of injury, location, medical provider notification, medical/nursing actions. 2. Complete the Patient/Visitor Accident/Incident Report. 3. Conduct a Post Fall Huddle as soon as possible after the fall. This should include the charge nurse, RN, LPN and NA involved in the patient’s care. The patient and/or family member may be included in the huddle. 4. Complete Post Fall Analysis 5. Complete the Post Fall Flowsheet. 6. Notify the physician if injuries are noted. 7. Notify the patient’s family. 3 Fall Prevention Policy 8. Update interventions if changes are noted in the patient’s condition. 9. Communicate to all shifts that the patient has fallen and is at risk to fall again. 10. For falls with significant harm, inform Quality Director and Nursing Manager. E. Emergency Department Fall Prevention All Emergency Dept. patients will be assessed for fall risk by the Triage Nurse. 2. These criteria will be assessed: a. Fall within 30 days b. Dizziness c. Confusion d. Current Seizures e. Age > 70 or < 3 3. Fall Precautions are initiated in the ED if the patient meets > 2 criteria. 1. F. Surgery Department Fall Prevention - All surgical patients are considered to be at risk for fall due to the effects of surgical preparation, medications received, and the surgical procedure performed. Fall risk is mitigated through continuous/frequent monitoring and observation of status pre, intra, and post-operatively. Procedure: 1. Place yellow identification band on surgical inpatients and communicate risk for fall during transfer of care communication to receiving nurse/unit. 2. Stay with all patients during episodes of transfer. 3. At the time of discharge: a. Assess ability to dress independently and safely. b. Instruct patient to remain seated while dressing. c. All Same Day Surgical patients will be discharged via wheelchair. d. Based on mobility and transfer ability, accompany patient with 1-2 staff members and assist safely into vehicle. 4. Patient Education a. Provide patient handouts at the time of admission b. Provide “Discharge Information pamphlet” upon discharge. VII. FALL PREVENTION PROGRAM EVALUATION: The Fall Prevention Team will analyze incident reports, post fall flow sheets and post fall analysis forms to determine patterns/concerns and to determine the need for action plans. VIII. REFERENCES: 4 Fall Prevention Policy 1. Perrell KL Assessing the Risk of Falls: Guidelines for Selecting Appropriate Measures for Clinical Practice Settings. Generations Winter 20022003. 2. Perrell KL, Nelson A. Goldman RL, Luther SL, et al. Fall Risk Assessment Measure: An Analytic Review. Journal of Gerontology 2001 vol 56A, No 12 M761-M766. 3. Oliver D, Britton M, Seed P, et al. Development and Evaluation of Evidence- based Risk assessment Tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ 1997; 315: 1049-1053. 4. Oliver D, Daly F, Martin F, et al. Risk Factors and risk assessment tools for falls in hospital in-patients: a systematic review. British Geriatrics Society 2004 33: 122-130. 5. Stevens JA Falls Among Older Adults-Risk Factors and Prevention Strategies 2005 NOCOA Falls Free: Promoting a National Falls Prevention Action Plan 6. Cameron KA The Role of Medication Modification in Fall Prevention 2005 NCOA Falls Free: Promoting a National Falls Prevention Action Plan 7. Hendrich AL, Bender PS, Nyhuis. Validation of the Hendrich II Fall Risk Model: A Large Concurrent Case/Control Study of Hospitalized Patients. Applied Nursing Research Vol 16 No 1 (Feb) 2003. p 9-21. 8. Halfens R, Roll S, Dassen T. Psychometric evaluation of the Hendrich Fall Risk Model. Journal of Advanced Nursing 53(3), 327-332. 9. Gray-Miceli, Deanna Fall Risk Assessment: Hendrich II Scale. Try This: Best Practices in Nursing Care to Older adults. Harford Institute for Geriatric Nursing. 8 (winter) 2006. 10. Health East Assessing Fall Risk and Determining Fall Risk Prevention Interventions 11. VA Fall Incident Reports and Assessment Tools 12. VA National Council on Patient Safety (NCPS) Tool Kit May 2004. Assessment Tools Reviewed 1. St Cloud Hospital- Hospital Inpatient Flow Sheet and Fall Assessment Tool 2. Marianjoy Fall Risk Assessment- from Marianjoy Rehabilitation Hospital -Pilkington, Ruroede, Cutler (Donna Pilkington, 1-630-4624000) 3. Morse Fall Scale 4. Owatonna Hospital (Hendrich II) 5. Fairview Southdale Hospital Fall Prevention Tools