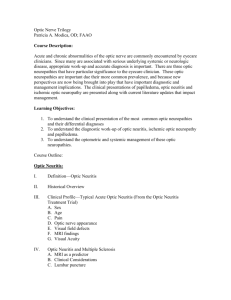
Select cases of optic nerve disease and their management

Select cases of optic nerve disease and their management
Rex Ballinger, OD FAAO VAMHCS Baltimore,MD, David Reed, OD FAAO, Havre de Grace, MD
Optic nerve overview:
The subarachnoid space of the brain is continuous with the optic nerve sheath
four parts; intraocular, intraorbital, intracanalicular, intracranial
Intraorbital: ~5 mm in diameter, with fat surround.
Intracanalicular: lesser wing of the sphenoid, surrounded by muscle cone
subarachnoid space: (CSF) with intracranial continuity
Case: Doc, the nerve is swelling up!!
Papilledema:
optic disc swelling secondary to elevated intracranial pressure
vision usually is well preserved with acute papilledema
almost always presents as a bilateral phenomenon
may develop over hours to weeks
The term is not be used to describe optic disc swelling with underlying infectious, infiltrative, or inflammatory etiologies.
Pathophysiology:
Disc swelling is result of axoplasmic flow stasis with intra-axonal edema in optic disc area
cerebrospinal fluid (CSF) pressure increases
pressure is transmitted to the optic nerve
optic nerve sheath acts to impede axoplasmic transport
accumulation of material at the level of the lamina cribrosa
characteristic swelling of the nerve head
Papilledema may be absent in cases of prior optic atrophy
Symptoms:
Headache: worse on awakening, exacerbated by coughing or other Valsalva maneuver.
Nausea and vomiting: if severe rise in ICP. Mmay be followed by a loss of consciousness, pupillary dilation, and death.
Visual symptoms often are absent: However: o transient visual obscurations (may be orthostatically related o Blurring of vision o constriction of the visual field o decreased color perception may occur. o Diplopia may be seen occasionally if a sixth nerve palsy is associated. o Visual acuity is preserved except in very advanced disease.
Clinical evaluation:
Disc hyperemia
Subtle edema of the nerve fiber layer especially nasal disc
Obscuration of fine peripapillary vessels.
Later obscuration of disc margins
Small NFL hemorrhages
Spontaneous venous pulsations, followed by venous congestion/ exudates/CWS
Peripapillary retinal radial folds (Paton lines). Choroidal folds also may be seen.
Chronic disease may lead to atrophy.
Etiology:
Any tumors or space-occupying lesions of the CNS
Idiopathic intracranial hypertension
Decreased CSF resorption
Increased CSF production (tumors)
Obstruction of the ventricular
system
Cerebral edema/encephalitis
Craniosynostosis
Management:
Tailored medical or surgical management
Specific therapy should be directed to the underlying mass lesion if present.
Diuretics: acetazolamide useful in selected cases (esp. idiopathic intracranial hypertension).
Weight reduction .
Corticosteroids
Surgical Care: removal of mass lesion
Lumboperitoneal shunt or ventriculoperitoneal shunt.
Optic nerve sheath decompression
Diet: (idiopathic intracranial hypertension)
Pseudotumor Cerebri
Pathophysiology: unclear.
Presumed resistance to absorption of CSF across the arachnoid villi.
Other theories: abnormality in cerebral circulation with increase in brain's H20
increase in ICP transmitted intracranial structures, including the optic nerves
commonly occurs in women who are overweight
role of obesity is unclear
increased intra-abdominal pressure suggested affecting cardiac filling pressures
leads to impeded venous return from the brain
untreated: may lead to optic neuropathy.
DDx:
Pseudopapilledema
Drusen of the optic nerve heads
Malignant hypertension
Bilateral infiltrative/infectious/inflammatory optic neuropathy
Bilateral anterior ischemic optic neuropathy
Bilateral optic nerve papillitis
Bilateral optic nerve tumors (eg, glioma, meningioma)
Work-up
Neuroimaging
Ultrasonography
Lumbar Puncture
Management:
Monitor: visual acuity, color vision, optic nerve head observation, and perimetry.
Weight control for patients who are overweight, 6% weight loss has been shown to reduce ICP and papilledema.
Use of diuretics to control the intracranial pressure: Acetazolamide 1 g/d (500 mg sequel bid) up to 2 g/d
furosemide if intolerant to acetazolamide (but less effective)
Corticosteroids: if inflammatory etiology, may supplement acetazolamide
Optic nerve sheath fenestration
Lumboperitoneal or ventriculoperitoneal shunt
The case of the hurting nerve
Optic neuritis:
Inflammation of the optic nerve- pain
initial episode in multiple sclerosis
DX is usually made clinically.
.
15- 20% of MS cases manifest as optic neuritis
38-50% of MS patients develop optic neuritis at some point
risk of development of MS after an episode of isolated optic neuritis was 30% at 5year follow-up and 38% at 10-year follow-up.
Other Etiologies:
Lyme disease orbital cysticercosis
Tuberculosis
Syphilis
viral agents such as HIV, hepatitis
B virus, herpes virus, and CMV
paranasal sinus infection
radiation therapy drugs gluten sensitivity hypereosinophilic syndrome vasculitis (GCA).
Management:
Optic Neuritis Treatment Trial:
28% and 35% of patients developed recurrence within 5 and 10 years,
Most recover spontaneously
Intravenous methylprednisolone therapy has shown to increase rates of visual recovery without significant long-term benefit for visual function.
Corticosteroids: considered for patients who require faster recovery
Treatment with corticosteroids and/or immunomodulation agents (eg, interferon beta-
1a, interferon beta-1b, glatiramer acetate) higher risk pts. (multiple sclerosis. )
Optic nerve glioma
cell of origin for optic nerve gliomas is unknown
classified as grade I astrocytomas (usually not, but may develop malignancy
meningeal hyperplasia vs perioptic meningioma.
Work-up:
MRI with gadolinium- imaging of choice
CT: evaluate erosion or expansion of the optic canal
Ultrasound: not helpful
Management:
Varies with size of tumor and pts. Health
Goal: cure the disorder, relieve symptoms, or improve vision or comfort.
Surgical removal may cure some optic gliomas
Partial removal to reduce some of the bulk of the tumor in many cases
Radiation therapy if tumor extensive and surgery not possible
Corticosteroids reduce swelling and inflammation during radiation Tx, or if symptoms recur.
The Cases of the swollen optic nerves:
A.
Disc edema
B.
Papilledema:
1.
Definition: bilateral disc edema secondary to increased intracranial pressure
2.
EMERGENCY!!
C.
Differential diagnosis of swollen optic nerves
1.
Ischemia: AION
Sex a.
Most common acute optic neuropathy > 50 years old
2.
Inflammation: optic neuritis
3.
Infiltrative: Sarcoid
4.
Infectious
5.
Compression: anterior orbital lesions
6.
Idiopathic and diabetic papillopathy
D.
65 yo WF Routine Eye Exam: Giant Cell (Temporal) Arteritis:
Characteristic
Age
AAION mean: 70
NAAION mean: 60
F>M F=M
Assoc. Symptoms
Visual Acuity
Optic Nerve
ESR
CRP
HA, scalp tenderness jaw claudication
TVL
< 20/200: 60% pallid edema normal size cup mean= 70m/hr male: age/2 female: age+10/2 high
high CRP & ESR=97% specific for GCA none
> 20/200: 60%
Pallid or hyperemic small cup: “disc at risk” mean=20-40mm/hr normal
FFA
Natural History
Management
Alphagan: 5/day disc and choroidal delay rarely improve fellow eye: 54%-95%
TA biopsy
1-2g. IV methylprednisone x 2-5 days
then 60-100mg oral prednisone x 6-8 weeks
then taper according to ESR/CRP months-year disc delay up 42% improve fellow eye: 12%-19% none proven:
1.
Arteritic Anterior Ischemic Optic Neuropathy: 5%-10% a.
Giant Cell Arteritis b.
American College of Rheumatolgy: need 3 of 5 criteria for diagnosis i.
development of symptoms or findings > 50 years old ii.
new onset, or new localized headache iii.
temporal artery tenderness or decreased pulsation iv.
Westergren ESR > 50mm/hr v.
positive TA biopsy: mononuclear cells or granulomatous inflammation c.
ocular manifestations: i.
ischemic optic neuropathy: anterior: 40%, posterior: 3% ii.
amaurosis fugax: 2%-19% iii.
central retinal artery occlusion: 15% iv.
other: vein occlusion, EOM palsy, retinal ischemia
2.
Non-Arteritic Anterior Ischemic Optic Neuropathy: 90%-95% a.
Risk Factors: i.
HTN: 50% ii.
Diabetes: 25% iii.
Other: smoking, collagen-vascular, hyperlipidemia, chronic renal failure & dialysis, and migraine b.
Pseudo Foster Kennedy Syndrome c.
IONDT: Ischemic Optic Neuropathy Decompression Trial: No benefit d.
NPION: Neuro Protection in Ischemic Optic Neuropathy: Pilot study i.
Alphagan 5 times per day ii.
May have small benefit: larger trial needed
E.
9 yoWF referred for blurry vision in one eye: Cat Scratch Neuroretinitis
1.
Organism: a.
Bartonella henselae: gram (-) rickettsia b.
transmitted: cats or fleas from infected cats
2.
Characteristics: a.
regional, painful lymphadenopathy b.
fever c.
malaise d.
2 weeks after cat scratch
3.
Clinical Findings: a.
Parinaud oculoglandular syndrome: i.
most common ocular manifestation: 7% ii.
granulomatous conjunctivitis iii.
PAN b.
Neuroretinitis: i.
Most common neuro-ocular manifestation ii.
visual loss with optic disc edema iii.
uveitis iv.
retinal edema with exudates: stellate v.
white retinal inflammatory lesions c.
BRAO: rare: retinal vasculitis with focal retinitis
4.
Management: a.
usually self-limited b.
doxycycline 100mg bid PO c.
ciprofloxacin 750 mg bid PO d.
other: trimethoprim-sulfamethoxazole & clindamycin