Selected Agents Used in Respiratory Disease
advertisement
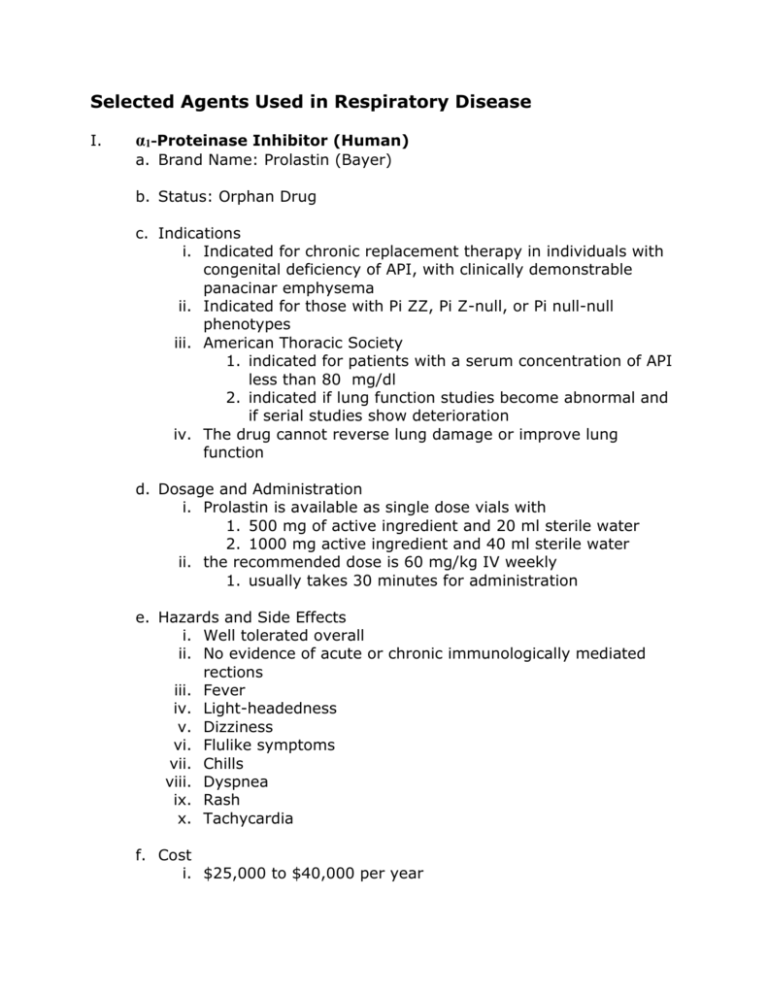
Selected Agents Used in Respiratory Disease I. α1-Proteinase Inhibitor (Human) a. Brand Name: Prolastin (Bayer) b. Status: Orphan Drug c. Indications i. Indicated for chronic replacement therapy in individuals with congenital deficiency of API, with clinically demonstrable panacinar emphysema ii. Indicated for those with Pi ZZ, Pi Z-null, or Pi null-null phenotypes iii. American Thoracic Society 1. indicated for patients with a serum concentration of API less than 80 mg/dl 2. indicated if lung function studies become abnormal and if serial studies show deterioration iv. The drug cannot reverse lung damage or improve lung function d. Dosage and Administration i. Prolastin is available as single dose vials with 1. 500 mg of active ingredient and 20 ml sterile water 2. 1000 mg active ingredient and 40 ml sterile water ii. the recommended dose is 60 mg/kg IV weekly 1. usually takes 30 minutes for administration e. Hazards and Side Effects i. Well tolerated overall ii. No evidence of acute or chronic immunologically mediated rections iii. Fever iv. Light-headedness v. Dizziness vi. Flulike symptoms vii. Chills viii. Dyspnea ix. Rash x. Tachycardia f. Cost i. $25,000 to $40,000 per year ii. proven cost effective in individuals who have severe α1antitrypsin deficiency and severe COPD g. α1-Antitrypsin Deficiency (API) i. Definition 1. a genetic defect that leads to the development of severe panacinar emphysema a. worse in lower lung zones b. accelerated by cigarette smoking c. usually accompanied by i. history of pneumonia ii. increased cough and sputum iii. parental history of emphysema ii. Onset 1. panacinar emphysema usually presents at 30 to 50 years of age iii. Incidence 1. accounts for 2% of all emphysema in the U.S. 2. 60,000 to 100,000 Americans with severe API 3. most prevalent in individuals of northern European descent iv. Pathohysiology 1. an imbalance between proteases (neutrophil elastase) and antiproteases (α1-proteinase inhibitor) 2. a process of alveolar wall destruction caused by insufficient protection from the protease neutrophil elastase a. the enzyme can cleave all forms of connective tissue and degrade elastic fibers in the lungs by solubilizing elastin b. with inadequate API levels in the lung to balance protease activity, emphysema results at a significantly earlier age than normally seen 3. A presentation of severe emphysema at an unexpectedly young age (third or fourth decade) leads to al high suspicion of API deficiency v. Genetics 1. A glycoprotein found on chromosome 14 2. Alleles of the API gene a. normal i. individual has normal serum levels of API 1. 150 to 350 mg/dl (20 to 48 µM) 2. Pi MM b. Deficient i. Lower than normal serum concentrations ii. Pi ZZ 1. most common form of deficiency c. Null i. Undetectable API levels in the serum ii. Pi null-null d. Dysfunctional i. API is present in normal amounts, but does not function normally ii. Pi Z-null II. Smoking Cessation Drug Therapy a. Nicotine i. The chief alkaloid in tobacco products ii. Nicotine addiction is the basis for tobacco dependence iii. Desirable Effects 1. pleasure and cognitive arousal 2. enhanced concentration 3. enhanced alertness and memory 4. decreased tension and anxiety iv. Undesirable Side Effects 1. GI and urinary tract a. diarrhea b. urination 2. Cardiovascular a. hypertension b. tachycardia c. peripheral vasoconstriction 3. Neuromuscular a. tremor b. loss of hand steadiness 4. Central Nervous System a. respiratory stimulation b. tremors c. convulsions d. nausea e. emesis b. Symptoms of Nicotine Withdrawal i. Nicotine craving ii. Nervousness iii. Irritability iv. Anxiety v. Drowsiness vi. Sleep disturbance vii. Impaired concentration viii. Increased appetite and weight gain c. Indications for Smoking Cessation Drug Therapy i. Indicated as an aid to smoking cessation to relieve nicotine withdrawal symptoms ii. Should be used as part of a comprehensive smoking cessation program to increase compliance and reduce relapse iii. Smokers with signs of high physical dependence on nicotine may benefit most Signs of High Physical Dependence on Nicotine Smokes more than 15 cigarettes per day Prefers brands with nicotine levels above 0.9 mg Has habit of inhaling smoke frequently and deeply Smokes within 30 minutes of rising Finds it difficult to give up the first morning cigarette Smokes most frequently in the morning Finds it difficult to refrain from smoking in smoke-free environments Smokes even when ill enough to be bed-ridden d. Drug Formulations Category Nicotine transdermal system Nicotine polacrilex Brand Name Habitrol Nicoderm Nicotrol Prostep Nicorette (gum) Nicorette DS (gum) Nicotrol NS (nasal spray) Nicotrol Inhaler Dosage 21 mg/day for 6 wk, 14 mg/day for next 2 wk, 7 mg/day for last 2 wk 21 mg/day for first 6 wk, 14 mg/day for next 2 wk, 7 mg/day for last 2 wk 15 mg/day for first 12 wk, 10 mg/day for next 2 wk, 5 mg/day for last 2 wk 22 mg/day for 4 to 8 wk, 11 mg/day for 2 to 4 wk 2 mg if fewer than 25 cigarettes/day; 9-12 pieces/day; maximum of 30 pieces/day 4 mg if 25 or more cigarettes/day; 912 pieces/day; maximum of 20 pieces/day 0.5 mg/spray, one each nostril (1.0 mg); 1-2 doses/hr, up to 5 doses/hr, or 40 doses/day for 6-8 wk; gradually reduce over next 4-6 wk 4 mg/use; recommended dosage is 24 to 64 mg per day, up to 12 wk, with gradual reduction over a period Bupropion Zyban up to 12 wk 150 mg sustained-release tablets; begin at 150 mg/day for 3 days; increase to 150 mg/day bid, with maximum of 300 mg/day, interval of 8 hr between doses; continue treatment for 7-12 wk i. Nicotine Transdermal and nicotine polacrilex are nicotine replacement agents ii. Bupropion is an antidepressant 1. it may relieve nicotine withdrawal 2. may be used in combination with nicotine replacement agents e. Precautions i. Potentially toxic concentrations of nicotine can occur in the blood 1. individuals should stop smoking when initiating therapy ii. transference of nicotine dependency from the tobacco product to the replacement product can occur 1. replacement formulations should be gradually withdrawn and stopped by three months iii. use of nicotine replacement therapy should be carefully weighed in patients with cardiovascular disease iv. healthcare workers should avoid handling active nicotine products 1. nicotine is easily absorbed through the skin 2. wash with water only a. soap will increase absorption v. used products must be disposed of properly 1. children and pets should not be exposed III. Nitric Oxide (NO) a. Background i. Produced by endothelial cells in the body ii. This endogenously produced vasodilator can be inhaled as a gas iii. Investigated for its ability to lower pulmonary vascular resistance in various states 1. Persistent pulmonary hypertension of the newborn (PPHN) 2. Acute respiratory distress syndrome (ARDS) b. Status: Orphan Drug c. Indications i. FDA approved on December 23, 1999 for use in neonates with hypoxic respiratory failure, to reduce pulmonary artery pressure and increase oxygenation in newborns with pulmonary hypertension and hypoxia 1. nitric oxide is used in conjunction with ventilatory support and other critical care in the treatment of term and near-term neonates (>34 weeks) with hypoxic respiratory failure associated with clinical or echocardiographic evidence of pulmonary hypertension ii. Off-label Uses 1. reduction of pulmonary vascular resistance and pulmonary artery pressure during neonatal cardiac surgery 2. treatment of hypoxemia or pulmonary hypertension after lung transplantation 3. treatment of acute respiratory distress syndrome (ARDS) d. Dosage and Administration i. Nitric oxide is supplied in two sizes of gas cylinder 1. 353 L 2. 1963 L ii. The recommended dose is 20 ppm iii. Treatment should be maintained up to 14 days or until the underlying oxygenation problem has resolved and the neonate can be successfully weaned from nitric oxide iv. May be administered with the INOvent system v. The vasodilating effect of inhaled nitric oxide ends with the removal of the gas 1. rebound hypertension may occur 2. an increase in FiO2 may be needed 3. close monitoring is critical e. Effect on Pulmonary Circulation i. Inhaled NO produces no effect when normal vascular resistance is present ii. With increased pulmonary vascular resistance, inhaled NO dilates pulmonary blood vessels in lung regions that receive gas flow 1. improved ventilation-perfusion matching 2. increased PaO2 f. Effect on Systemic Circulation i. No systemic vasodilation or hypotension occurs 1. nitric oxide rapidly combines with hemoglobin making it inactive g. Toxicity i. nitric oxide 1. mediator of lung injury ii. nitrogen dioxide 1. causes lipid peroxidation in cells a. causes pulmonary edema 2. exposure to > 150 ppm is usually fatal iii. methemoglobin 1. unable to carry oxygen 2. usually not a problem at usual inhaled NO doses 3. should be monitored h. Contraindications i. Inhaled NO should not be used in neonates who are known to dependent on right-to-left shunt