Best Evidence Topics Report by: Lucy Adcock Institution: LTHT Date
advertisement
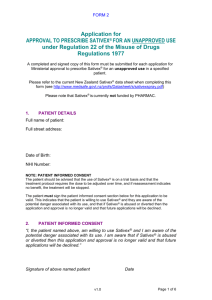
Best Evidence Topics Report by: Lucy Adcock Institution: LTHT Date Completed: April 2014 Three Part Question What is the evidence for Nabilone in the treatment of pain for Palliative patients? Clinical Scenario Sitting in Chronic Pain MDT. A patient presented by one consultant, another consultant suggests adding in Nabilone for neuropathic pain. I wondered, is there a role for our population and where the evidence base lies for use in pain? Pharmacology of Synthetic Cannabinoids 2 main cannabinoid receptors (CB1, CB2). May be activated by endogenous and synthetic cannabinoids. CB1 primarily in terminals of central and peripheral neurons, controlling levels of neurotransmitters (ACh, NA, D2, 5HT, GABA, D-aspartate and cholecystokinin). CB2 mainly expressed in immune cells, affecting cytokine release. 3 synthetic CB1/CB2 agonists: Nabilone, licensed 1981, for chemotherapy induced N&V. Dronabinol, 1985, anti-emetic and appetite stimulant (AIDS patients) Sativex (oral mucosal spray), 2005, prescribed for neuropathic pain in MS and adjunctive analgesia for adults with advanced cancer. Adverse effects incl: light-headedness, dry mouth, fatigue, myalgia, palpitations. Search Strategy Medline/Embase 1. Cannabinoids exp AND pain exp AND palliat* (limit humans and English) 2. Nabilone AND cancer AND pain (limit humans and English) 3. Nabilone AND pain (limit humans and English) Cross referencing in relevant articles Search Outcome Several review articles discuss potential for use. 1 original article Few original articles with some relevance to palliative population Relevant Paper(s) Author, date and country Maida et al, 2008 Canada Patient group Study type Outcomes Key results Study Weaknesses Cancer patients referred to SPCT Jan 05Oct 06. Prospective observational. Edmonton Symptom Assessment Scale (ESAS), Palliative Performance Scale (PPS), Morphine Sulphate Equivalence (MSE) use, other analgesic use. 112 patients, 65 untreated, 47 treated (24 for pain). Open label, no randomisation, groups not comparable. Treated:Mean pain 7.1 ->3.0 (adj) – p<0.001 Don’t specify how they decided who to treat. Untreated:Mean pain 5.6 -> 5.5 N=11. No documentation of pain type Small numbers Intention to treat model. Wissel J et al, 2006, Germany MS patients with spasticityrelated pain Placebocontrolled, double-blind, cross-over 11-Point-BoxTest Turcotte et al, 2011 Canada MS induced neuropathic pain, on doses >1800mg/day gabapentin and inadequate pain relief. Randomised, placebocontrolled, double-blind. VAS daily pain rating. Toth C et al, 2012, Canada Diabetic peripheral neuropathy, pain score Randomised, placebocontrolled, double-blind VAS functional impact rating. VAS, HADS, Medical Outcomes Study Sleep Significant decrease in pain (p<0.05). NO change in spasticity, motor function or ADLs 15 patients. Pain significantly reduced in treatment group (p<0.001) 1 patient dropped out in treatment arm due SEs N=37 26/37 had >30% pain (unable to obtain full paper) Small numbers Nonresponders were eliminated >4/10 Reynolds & Osborn, 2013, UK Man with poorly controlled chronic pain 2’ to facial tumour resection Scale, European QoL index Case study reduction in first 4wk open label phase. 13 continued nabilone for 5 more weeks and effect sustained. (p<0.05). Mean reduction of pain 1.27. 2 subjects discontinued due to SE in first phase. Pain improved, managed to reduce opioids and ketamine doses. from subsequent stats. Small numbers. Single case study “Results of a Phase III study (N = 177) comparing Sativex, THC-predominant extract and placebo in intractable pain due to cancer unresponsive to opiates (Johnson and Potts 2005) demonstrated that Sativex produced highly statistically signify cant improvements in analgesia (Table 1), while the THC predominant extract failed to produce statistical demarcation from placebo, suggesting the presence of CBD in the Sativex preparation was crucial to attain significant pain relief.” -Above ‘study’ is basis for approval in Canada for Sativex in the treatment of intractable cancer pain. Clinical Bottom Line Potential for use. Insufficient trial evidence for regular or first line use. Might be worth considering, particularly within licensed population. References Maida V et al; Adjunctive Nabilone in Cancer Pain and Symptom Management:A Prospective Observational Study Using Propensity Scoring; J Support Oncol 2008;6:119-124. Wissel J et al; Low dose treatment with synthetic cannabinoid Nabilone significantly reduces spasticity-related pain. A double-blind placebo-controlled cross-over trial; Journal of Neurology 2006; 253(10): 1337-1341. Turcotte D et al; A randomised, double-blinded, placebo-controlled study evaluating the efficacy and safety of nabilone as an adjunctive to gabapentin in managing multiple sclerosis induced neuropathic pain; Conference:5th Joint Triennial Congress of the European and Americas Committee for Treatment and Research in Multiple Sclerosis 2011. (Above also presented in 18th Annual Conference of Rehabilitation in MS 2013) Toth C et al; An enriched-enrolment, randomised withdrawal, flexible-dose, double-blind, placebocontrolled, parallel assignment efficacy study of nabilone as adjuvant in the treatment of diabetic peripheral neuropathic pain; Pain 2012;153:2073-2082. Reynolds TD, Osborn HL; The use of cannabinoids in chronic pain; BMJ case reports 2013. Johnson JR, Potts R. 2005. Cannabis-based medicines in the treatment of cancer pain: a randomised, double-blind, parallel group, placebo-controlled, comparative study of the efficacy, safety and tolerability of Sativex and Tetranabinex in patients with cancer-related pain.; 2005 March 8-11; Edinburgh, Scotland.