Respiratory I and II
advertisement
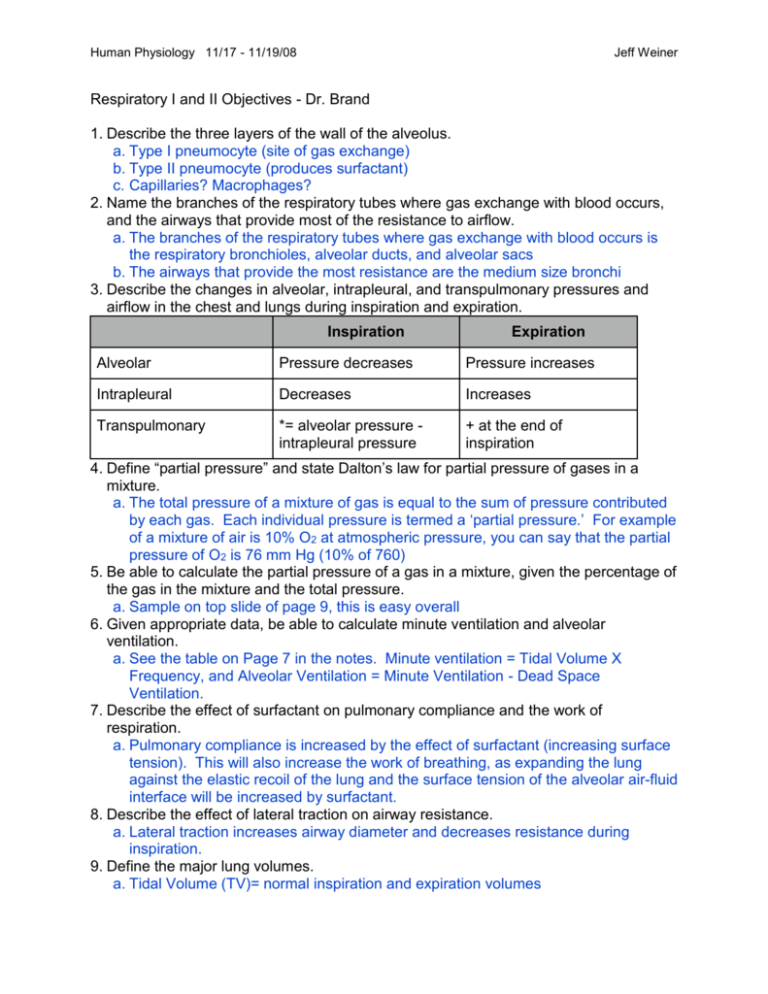
Human Physiology 11/17 - 11/19/08 Jeff Weiner Respiratory I and II Objectives - Dr. Brand 1. Describe the three layers of the wall of the alveolus. a. Type I pneumocyte (site of gas exchange) b. Type II pneumocyte (produces surfactant) c. Capillaries? Macrophages? 2. Name the branches of the respiratory tubes where gas exchange with blood occurs, and the airways that provide most of the resistance to airflow. a. The branches of the respiratory tubes where gas exchange with blood occurs is the respiratory bronchioles, alveolar ducts, and alveolar sacs b. The airways that provide the most resistance are the medium size bronchi 3. Describe the changes in alveolar, intrapleural, and transpulmonary pressures and airflow in the chest and lungs during inspiration and expiration. Inspiration Expiration Alveolar Pressure decreases Pressure increases Intrapleural Decreases Increases Transpulmonary *= alveolar pressure intrapleural pressure + at the end of inspiration 4. Define “partial pressure” and state Dalton’s law for partial pressure of gases in a mixture. a. The total pressure of a mixture of gas is equal to the sum of pressure contributed by each gas. Each individual pressure is termed a ‘partial pressure.’ For example of a mixture of air is 10% O2 at atmospheric pressure, you can say that the partial pressure of O2 is 76 mm Hg (10% of 760) 5. Be able to calculate the partial pressure of a gas in a mixture, given the percentage of the gas in the mixture and the total pressure. a. Sample on top slide of page 9, this is easy overall 6. Given appropriate data, be able to calculate minute ventilation and alveolar ventilation. a. See the table on Page 7 in the notes. Minute ventilation = Tidal Volume X Frequency, and Alveolar Ventilation = Minute Ventilation - Dead Space Ventilation. 7. Describe the effect of surfactant on pulmonary compliance and the work of respiration. a. Pulmonary compliance is increased by the effect of surfactant (increasing surface tension). This will also increase the work of breathing, as expanding the lung against the elastic recoil of the lung and the surface tension of the alveolar air-fluid interface will be increased by surfactant. 8. Describe the effect of lateral traction on airway resistance. a. Lateral traction increases airway diameter and decreases resistance during inspiration. 9. Define the major lung volumes. a. Tidal Volume (TV)= normal inspiration and expiration volumes Human Physiology 11/17 - 11/19/08 Jeff Weiner b. IRV = inspiratory reserve volume, or the amount that can be forcibly inhaled during a deep breath i. Inspiratory capacity = TV + IRV c. ERV = expiratory reserve volume, or the amount that can be forcibly exhaled d. ReV = residual volume, or the amount that will remain in the lungs even after a forced exhale (prevents lung collapse) i. Functional residual capacity = ERV + ReV e. Vital capacity = IRV + TV + ERV f. Total lung capacity = sum of everything 10. Define forced vital capacity (FVC) and forced expiratory volume in 1 sec (FEV1) a. FEV1 = Forced Expiratory Volume in 1 second b. FVC = Forced vital capacity = the amount that can be forcibly exhaled over a longer period of time (~10 seconds) 11. Explain how vital capacity and FEV1 change in obstructive or restrictive lung disease. a. Obstructive disease: FEV1 will be < 80% of FVC b. Restrictive disease: VC is reduced, but the ratio of FEV1/FVC remains normal 12. Define anatomic and physiological dead space. a. The anatomic and physiological dead space consists of the conducting zone (trachea, bronchi, bronchioles, terminal bronchioles). The term ‘dead zone’ means that there is no gas exchange 13. Describe the effects of changing alveolar ventilation, metabolism, and breathing air low in O2 concentration on alveolar partial pressures of O2 and CO2. Condition Breathing air with low PO2 Alveolar PO2 Alveolar PCO2 Decreases No change Inc. Alveolar ventilation & unchanged metabolism Increases Decreases Dec. Alveolar ventilation & unchanged met. Decreases Increases Inc. metabolism & unchanged alveolar ventilation Decreases Increases Dec. Metabolism & unchanged alveolar ventilation Increases Decreases Proportional increases in metabolism and alveolar ventilation No change No change 14. Explain the role of ventilation-perfusion inequalities in causing hypoxemia. a. Ventilation without perfusion: Blood flow is blocked, alveolar gas will not get to exchange O2 and CO2 with blood, so PO2 and PCO2 will be equal to 149 mm Hg and 0 mm Hg, respectively, the level of inspired air b. Perfusion without ventilation: Example- tumor blocking air flow to alveoli: Gases will equilibrate with venous blood levels, as no new oxygen is brought in c. With a significant V/Q mismatch (perfusion w/o ventilation), pulmonary venous blood from the mismatched region will have low PO2, (hypoxemia) Human Physiology 11/17 - 11/19/08 Jeff Weiner 15. Name the two forms in which O2 is carried in the blood, and state the relative amount carried in each form. a. Oxygen carried by hemoglobin: 1 gram of hemoglobin combines with 1.34 ml O2 at 100% saturation. Normal blood contains 15g/100 ml Hb at 98.5% saturation. 1.34 ml/gm of Hb x 15g/100 ml x 0.985 = 19.7 ml O2/100 ml blood or 197 ml O2/L b. Oxygen carried in solution: The amount of gas dissolved in a liquid is the product of the partial pressure of the gas in the gas phase and the solubility of the gas in the liquid (Henry’s law). 0.03 ml O2 per mm HG per L plasma x 100 mm Hg = 3 ml O2/ Liter plasma 16. Describe the effects of partial pressure of PCO2, the H+ concentration (pH), temperature and DPG concentration on the O2-Hemoglobin dissociation curve. a. Hemoglobin gives up O2 more readily with: i. Decrease in pH, rise in PCO2, a rise in temperature, and a rise in 2,3 DPG from red blood cells 17. Name the three forms in which CO2 is carried in the blood, and state the relative amount carried in each form as given in class. a. 80-90% carried as HCO3 b. 5-10% carried as carbamino Hb c. 5-10% is dissolved in the plasma 18. Describe the role of carbonic anhydrase in CO2 transport. a. Carbonic anhydrase catalyzes the conversion of H2O and CO2 --> H2CO3, (and essentially HCO3 + H+) making it a virtually instantaneous conversion. The reverse reaction is also catalyzed by CA, depending on the concentration of the reactants/products. 19. Give the location of the central and peripheral chemoreceptors. a. Central: Central chemoreceptors of the central nervous system, located on the ventrolateral medullary surface, are sensitive to the pH of their environment. These act to detect a change in pH of the cerebral spinal fluid that are indicative of a change in oxygen or carbon dioxide concentration available to brain tissues. An increase in carbon dioxide tension of the arteries, often resulting from increased CO 2 intake (hypoxia) indirectly cause the blood to become more acidic; the cerebral spinal fluid pH is closely comparable to the plasma pH, as carbon dioxide easily diffuses across the blood/brain barrier. However, it is important to note that a change in plasma pH will not stimulate central chemoreceptors as H+ will not be able to diffuse into the CSF. Only CO2 levels affect this as it can diffuse across into the CSF, forming H+ and decreasing pH. Central chemoreception remains, in this way, distinct from peripheral chemoreceptors. B. Peripheral: Peripheral chemoreceptors act most importantly to detect variation of the oxygen in the arterial blood, in addition to detecting arterial carbon dioxide and pH. These nodes, called the aortic body and carotid body, are located on the arch of the aorta and on the common carotid artery, respectively. A continual signal is sent, via cranial nerves IX and X, from the peripheral chemoreceptors. Human Physiology 11/17 - 11/19/08 Jeff Weiner With a decrease in arterial oxygen tension, the signal intensifies, calling for an increase in respiration. 20. Describe the effects of changes in PO2, PCO2 and H+ concentration on the central and peripheral chemoreceptors. a. A rise in arterial PCO2, decrease in PO2 or drop in pH will stimulate peripheral chemoreceptors, which will act on respiratory neurons, which stimulate respiratory muscles to increase ventilation b. Central sets off the same neurons and reactions, but only responds to a rise in arterial CO2 21. Describe the effects of aging on the respiratory system and tell how they affect oxygenation of arterial blood. a. Lungs: i. Loss of alveolar surface area, loss of pulmonary capillaries, increased lung compliance due to loss of elastic and connective tissue, loss of pulmonary elastic recoil, decreased transpulmonary pressure, decreased traction on small airways, increased resistance to air flow, decreased maximal expiratory air flow, decreased FEV1 b. Chest wall i. Decreased compliance of the chest wall ii. Decreased respiratory muscle strength 22. Name the major buffers of intra- and extracellular fluids. a. Extracellular buffers: H2CO3 (acid) and HCO3- (base) b. Intracellular buffers: proteins and organic phosphates i. Proteins contain NH2 and carboxyl groups that act as proton donors or acceptors. Phosphates may act as proton donors or acceptors 23. Describe the respiratory compensation for metabolic acid base disturbances, and the renal compensation for respiratory acid base disturbances. a. Disorder Primary Defect Buffering Compensation Metabolic acidosis Increase H+ production ECF: HCO3ICF: Protein, phosphate Hyperventilation Respiratory acidosis Increase PCO2 ICF proteins, organic phosphates Increased HCO3generation Metabolic alkalosis Increase HCO3production Increase lactic acid synthesis (minor) Hypoventilation Respiratory alkalosis Decrease PCO2 Increase lactic acid synthesis (major) Increased HCO3excretion b.