Innovation Workbench
advertisement

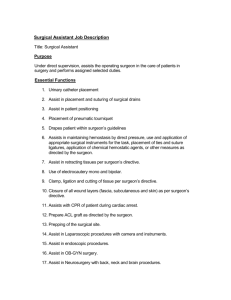
Inventive Problem Solving Ideation Process Project Initiation 1. Project objectives The specific aims are: · modification of existing infrared visualization system, · optimization of design specifications for integration into a surgical setting, · verification of designed system both in vitro and in vivo. 2. Importance of the Situation This system would improve performance in preserving the parathyroid and thyroid glands during endocrine surgery by mitigating the impact of surgeon enperience in a low-cost, time-saving way. Innovation Situation Questionnaire 1. Brief description of the situation Complications from incomplete or accidental removal of the parathyroid glands are a major concern associated with endocrine surgery. Current localization techniques are primarily preoperative and only applicable in select surgeries. The proximity of the various tissues encountered in the neck during surgery and the tendency of these tissues to blend together serve as confounding factors for surgeons. There is a need for a sensitive, real-time, intra-operative diagnostic tool to assist with anatomical guidance. Previous studies have shown the ability of near-infrared (NIR) autofluorescence to differentiate between the parathyroid and the surrounding tissue based on the intrinsic optical properties. The parathyroid exhibits stronger fluorescence than all other tissues in the neck. Near-infrared imaging would provide spatial context as a more intuitive approach for the surgeon. Here we present the first application of an autofluorescencebased imaging system for real-time intra-operative use in endocrine surgery. A 785nm diode laser is used to excite the tissue and a converter tube is employed to detect the NIR fluorescence and render it in the visible wavelengths. The image is then captured by CCD and processed to apply a false color gradient for distinction between tissue types. We demonstrate the utility of the NIR fluorescence imaging system in vivo and in vitro. Preliminary results indicate that imaging is able to capture the higher level of autofluorescence exhibited by the parathyroid differentiating it from the surrounding tissue. 2. Detailed description of the situation 2.1. Supersystem - System - Subsystems 2.1.1. System name Parathyroid Intra-operative Visualization System 2.1.2. System structure This system consists of a diode laser, expanding optical elements, an infrared viewer, CCD camera, and Innovation WorkBench® software. Apr/09/2010, 11:31 1 Inventive Problem Solving Labview interface. The optical elements include focussing, expanding lenses and a liquid-light guide. The infrared viewer uses a telephoto c-mount camera lens and photomultiplier tube. The CCD camera connects to the NI DAQ board via BNC cables. NI Labview program handles data processing. 2.1.3. Supersystems and environment The system will function within an endocrine surgery operating room; nearby systems include surgical tools, patient monitoring equipment, and other devices used in surgery. The system will be operated by the surgeron, handled a surgical aide, nurse, or technician. Requires a computer interface and power supply. Must be located outside of surgical halo. Dimensions must not interfere with surgical protocol or equipment. 2.1.4. Systems with similar problems Other imaging devices used for intraoperative modeling have similar restrictions and issues, necessitating use of collimated light to span the distance of the sterile field. 2.2. Input - Process - Output 2.2.1. Functioning of the system The system emits near-infrared light onto the tissue and detects the light emitted from the fluorescing parathyroid glands which it displays in visible wavelengths. The purpose of this function is to increase surgeon's ability to discriminate between tissues by using relative brightness as an indicator. 2.2.2. System inputs Infrared autofluorescent light that has scattered from the parathyroid and thyroid tissues is the system input. 2.2.3. System outputs A real-time image of the surgical field is displayed through a labview controlled computer interface. 2.3. Cause - Problem - Effect 2.3.1. Problem to be resolved The problem that exists is the inability to establish absolute levels of fluorescence to use as a threshold for parathyroid gland emission. Innovation WorkBench® software. Apr/09/2010, 11:31 2 Inventive Problem Solving 2.3.2. Mechanism causing the problem Cause: Each patient has different physiology and variations existed with emitted signal intensity. Effect: No absolute value can be arbitrarily assigned as a threshold that will always work for all patients. Cause: Location of parathyroid glands varies for all patients, sometimes not on thyroid surface. Effect: Resolution decreases and light is further attenuated by scattering-- decreased light emission. 2.3.3. Undesirable consequences if the problem is not resolved If not addressed, technology would give little help to surgeon. Also, if not addressed, system must be calibrated for each patient before use. 2.3.4. Other problems to be solved 2.4. Past - Present - Future 2.4.1. History of the problem This problem has existed since the inception of the system: fluorescence has strong patient variability and must be accounted for. 2.4.2. Pre-process time Pre-surgical levels of autofluorescence cannot be tested in a non-invasive method, thus the variability must be accounted for on a patient to patient basis during each surgery. 2.4.3. Post-process time This is not an option as the device is intended for use in the surgery and after the process wiol have no effect. 3. Resources, constraints and limitations 3.1. Available resources Substance resources: 785nm Diode laser, ex vivo thyroid, parathyroid tissue, filters, lenses, IR Viewer, Computer, DAQ board Field Resources: EM light filed from laser Space Resources: Surgeon's field of view, imagng field Time Resources: preliminary surgical planning, intra-operative time, post-surgical time Informational Resources: fluorescence of tissue, measured and fed to computing interface Functional resources: Identification of fluoresceing cancer tissue in an unexpected area. 3.2. Allowable changes to the system Small changes to the system are allowed: Imaging device and software can be altered if improved technology is available. Excitation method, image processing also allowed to be changed if the improvements can be attained. 3.3. Constraints and limitations IR viewer and computer interface must remain constant, can be altered if better technology is affordably attained. Cost must not significantly increase. Excitation wavelength and power must remain constant for safety considerations. 3.4. Criteria for selecting solution concepts Finished device should operate with >80% sensitivity and specificity. Innovation WorkBench® software. Apr/09/2010, 11:31 3 Inventive Problem Solving Problem Formulation and Brainstorming IR V Diagram 4/9/2010 11:14:24 AM. 8. Find a way to eliminate, reduce, or prevent Interpatient fluorescence variation in order to avoid Complications exist. Enhance useful parameters Universality Use software interface to select region of thyroid tissue to use as a baseline. This will account for inter-patient variability of fluorescence and remove need for absolute fluorescence levels. Develop Concepts 1. Categorize preliminary ideas Use arbitrary threshold levels to quantify fluorescence. Innovation WorkBench® software. Apr/09/2010, 11:31 4 Inventive Problem Solving Determine method of relative evaluation using patient specific baseline normalization. 2. Combine ideas into concepts Method for real-time visualization to detect differential fluorescence of tissues: Idea: use head-mounted apparatus for surgeon- hands free, can focus on patient without looking away from working field. Short-coming: current technology is cost-prohibitive, difficult to apply processing interface, must apply filtering optics, different excitation light source necessary Idea: use mounted IR viewer outside surgical field that outputs to video screen in OR-Still hands free, allow image processing programs, simple mounted excitation source, can apply necessary filters, cheap, zoom capabilities. Short-comings: bulky, may require adjusting to focus on patient or region of interest. Idea: Use program interface to select region of interest for patient baseline. Short-comings: Fluorescence baseline will be dependent upon surgeon's discretion and experience. Evaluate Results 1. Meet criteria for evaluating Concepts Improve sensitivity and specificity of process compared to current values. Do not reduce surgical performance. Reduce time required for endocrine surgery. 2. Reveal and prevent potential failures System does not excite tissue beyond surface-- surgeon must decide where to begin resecting based on experience. 3. Apply Patterns/Lines of Evolution Increasing ideality Ensure reduction of surgical time requirement while improving surgical results Increasing controllability Allow adaptable lenses for use with a hands free system that will auto-focus. Element universalization Allow for this system to be used in other surgeries if IR excitation is found useful for tissue discrimination. 4. Plan the implementation Create a software interface that will allow the user to select a region as a baseline, based on suregeon experience and environmental factors, Use external light source for co-registration purposes. Innovation WorkBench® software. Apr/09/2010, 11:31 5