Supplementary Information (doc 49K)
advertisement
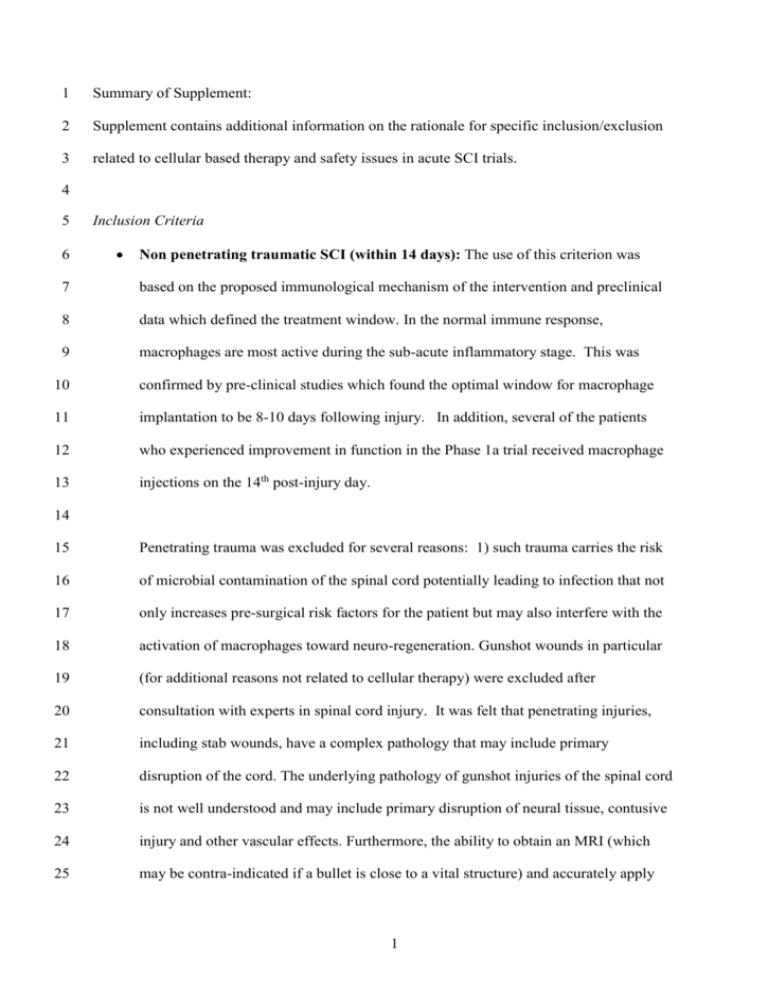
1 Summary of Supplement: 2 Supplement contains additional information on the rationale for specific inclusion/exclusion 3 related to cellular based therapy and safety issues in acute SCI trials. 4 5 6 Inclusion Criteria Non penetrating traumatic SCI (within 14 days): The use of this criterion was 7 based on the proposed immunological mechanism of the intervention and preclinical 8 data which defined the treatment window. In the normal immune response, 9 macrophages are most active during the sub-acute inflammatory stage. This was 10 confirmed by pre-clinical studies which found the optimal window for macrophage 11 implantation to be 8-10 days following injury. In addition, several of the patients 12 who experienced improvement in function in the Phase 1a trial received macrophage 13 injections on the 14th post-injury day. 14 15 Penetrating trauma was excluded for several reasons: 1) such trauma carries the risk 16 of microbial contamination of the spinal cord potentially leading to infection that not 17 only increases pre-surgical risk factors for the patient but may also interfere with the 18 activation of macrophages toward neuro-regeneration. Gunshot wounds in particular 19 (for additional reasons not related to cellular therapy) were excluded after 20 consultation with experts in spinal cord injury. It was felt that penetrating injuries, 21 including stab wounds, have a complex pathology that may include primary 22 disruption of the cord. The underlying pathology of gunshot injuries of the spinal cord 23 is not well understood and may include primary disruption of neural tissue, contusive 24 injury and other vascular effects. Furthermore, the ability to obtain an MRI (which 25 may be contra-indicated if a bullet is close to a vital structure) and accurately apply 1 1 the MRI eligibility criteria in this group of patients was felt to be limited by metal 2 artifact. 3 4 A single spinal cord lesion between C5 motor/C4 sensory level and T11 5 neurological level by the ISNCSCI: The neurological levels chosen originally were 6 C5 to T11. The upper level (C5) was chosen for safety reasons to lessen the risk that 7 ascent of the neurological level caused by adverse effects of parenchymal macrophage 8 injection could result in damage to the phrenic nucleus. Therefore, this criterion 9 allows for a one level safety margin for respiratory status and ventilatory 10 requirements. Early in the trial it was noted that many “C5” injuries were indeed C5 11 motor, but had some sensory deficit in the C5 dermatome, which, by the ISNCSCI, 12 would indicate the neurological level of injury was C4. After a review by the Steering 13 Committee, the inclusion criterion was changed and the protocol amended to C5 14 motor as it was felt that if motor function was intact at C5 despite some sensory 15 impairment, there was minimal increased risk of additional respiratory compromise, 16 thus meeting the original safety-based intent of the neurological level eligibility 17 criterion. There also may be a question of the validity of the C5 sensory point (as 18 defined in the ISNCSCI reference manual as the lateral side of the antecubital fossa1) 19 and whether it is truly representative of the C5 versus the C6 dermatome in the 20 majority of individuals.2 T11 was chosen as the lowest level in order to avoid conus 21 medullaris and cauda equina injuries since the proposed mechanism of action was the 22 promotion of axonal regeneration in the spinal cord rather than neuroprotection of 23 anterior horn cells or regeneration of axons in the cauda equina. For those injuries at 24 or close to T11, a careful review of the MRI was required to ensure that the lesion did 25 not, in fact, extend significantly into the conus medullaris creating technical 2 1 difficulties for the surgeons due to the diminished cross-sectional area of the conus 2 and also increasing the chances of significant concomitant lower motor neuron injury. 3 4 Complete SCI (AIS A): Participants with a complete SCI were chosen to lessen the 5 risk of adverse neurological outcome since this group of patients is clearly the least 6 likely to experience spontaneous improvement. Although the neurological level and 7 completeness criteria were based on the ISNCSCI, one exception was discussed mid- 8 study. Several cervical injury participants were examined at baseline (7-10 days post 9 injury) and found to have evolving buttock or foot sensation in the absence of ano- 10 rectal sensation or volition. While these patients were technically classified as 11 “complete” by the International Standards, they were felt to be “in evolution” to 12 incomplete status and as such, did not meet the intent of the safety-based eligibility 13 criterion. As the goal of the trial was to enroll participants with clinically complete 14 injuries, those individuals with a zone of partial preservation extending greater than 5 15 segments below the level of injury were excluded as it was felt they were potentially 16 evolving to an incomplete injury, although technically complete by the ISNCSCI. 17 18 19 Exclusion Criteria Fever (>38.4 °C), 24 hours prior to scheduled tissue harvest: Febrile patients were 20 excluded to minimize the risk of product contamination with bacteria that might be 21 circulating in the blood. 22 23 24 Blood transfusion within 3 days prior to scheduled tissue harvest: As this was an autologous therapy, it was necessary to ensure the blood required to isolate the 3 1 monocytes was a true autologous sample. Estimates on the half life of circulating 2 monocytes range from 4.5 -20 hours.3,4 3 4 Human immunodeficiency virus (HIV), hepatitis B and C positive: As the basis 5 for the therapy is immunological, the cells involved in the immune system response 6 could not be compromised by HIV. Patients with HIV, Hepatitis B or C were 7 excluded to minimize risks to manufacturing staff processing the autologous blood 8 sample (handling potentially contaminated blood). 9 10 Previous or concomitant treatment with: o Immune modulators or experimental drugs 60 days prior to study 11 12 enrollment o Acute immune modulators (i.e. dexamethasone, methylpredisolone 13 14 (MPSS)) within 5 days prior to scheduled skin harvest 15 These exclusions were to ensure the macrophage and immune responses were not 16 compromised. An exception was the standard use of MPSS in the 24-48 hours 17 following SCI, as the mean half-life 3.54 days in patients with acute spinal cord 18 injury; therefore immune system response would no longer be impacted by day 7-8 19 following injury.5 Dexamethasone and other immune modulators such as 20 fludrocortisone, also required a 5 day window for clearance prior to skin and blood 21 harvest. 22 23 24 Hematopoetic inducers (e.g. erythropoietin [Procrit]) following injury: This was added to the list of exclusions as a protocol amendment after discovering technical 4 1 difficulties during the cell separation procedure in participants who had received 2 hematopoetic inducers. 3 4 Longitudinal dimension of injury determined by MRI > 3 cm and anatomical 5 transection of the cord visualized by MRI: A contusion size ≤ 3 cm without spinal 6 cord transection was determined based on Phase 1a data. In that study, a lesion size 7 of one vertebral segment was used in order to target a “moderate” size lesion, 8 eliminating the most severe contusions. As the length of one vertebral segment 9 varies depending on the location in the spinal column and based on individual 10 characteristics of the participant (height), a more objective measurement was chosen 11 for Phase 2. The MRI criterion of no transection was chosen, because an individual 12 with transection of the long tracts was less likely to benefit from the intervention. 13 Additionally, it was noted in the Phase I trial that for the one participant with spinal 14 cord transection noted intra-operatively, it was difficult to accurately inject the 15 macrophages due to the condition of the cord, nor did this individual demonstrate 16 recovery. 5 References: 1. American Spinal Injury Association. International standards for neurological classification of spinal cord injury, revised 2000, reprinted 2002. Chicago, IL: American Spinal Injury Association; 2002. 2. Browne BJ, Jacobs SR, Herbison GJ, Ditunno JF. Pin sensation as a predictor of extensor carpi radialis recovery in spinal cord injury. Arch Phys Med Rehabil 1993; 74: 14-18. 3. Weinberg JB (ed). Mononuclear phagocytes. In: Greer J (ed). Wintrobe’s Clinical Hematology. 11th edn. Lippincott Williams and Wilkins: Philadelphia, PA, 2004, pp 355-378. 4. Guyton AC, Hall JE (eds). Resistance of the body to infection. In: Textbook of Medical Physiology. 10th edn. W.B. Saunders Company: Philadelphia, PA, 2000, pp 392-401. 5. Segal JL, Maltby BF, Langdorf MI, Jacobsen R, Brunnemann SR, Jusko WJ. Methylprednisone disposition kinetics in patients with acute spinal cord injury. Pharmacotherapy 1998;18(1): 16-22. 6