NICU Survival Guide - School of Medicine
advertisement
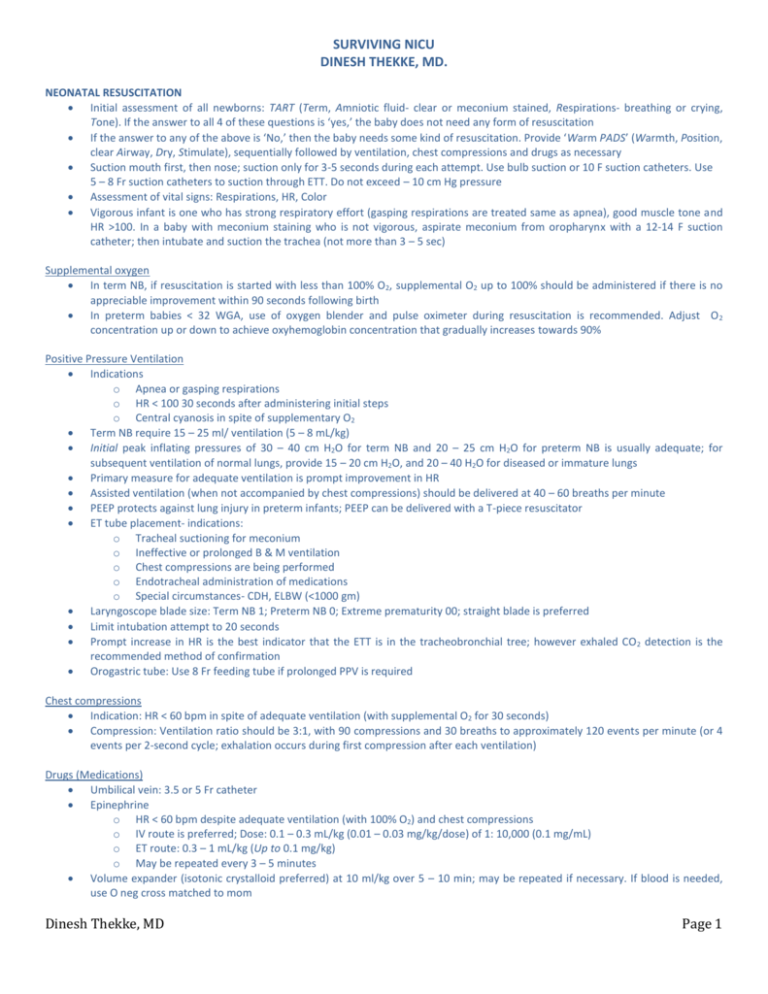
SURVIVING NICU DINESH THEKKE, MD. NEONATAL RESUSCITATION Initial assessment of all newborns: TART (Term, Amniotic fluid- clear or meconium stained, Respirations- breathing or crying, Tone). If the answer to all 4 of these questions is ‘yes,’ the baby does not need any form of resuscitation If the answer to any of the above is ‘No,’ then the baby needs some kind of resuscitation. Provide ‘Warm PADS’ (Warmth, Position, clear Airway, Dry, Stimulate), sequentially followed by ventilation, chest compressions and drugs as necessary Suction mouth first, then nose; suction only for 3-5 seconds during each attempt. Use bulb suction or 10 F suction catheters. Use 5 – 8 Fr suction catheters to suction through ETT. Do not exceed – 10 cm Hg pressure Assessment of vital signs: Respirations, HR, Color Vigorous infant is one who has strong respiratory effort (gasping respirations are treated same as apnea), good muscle tone and HR >100. In a baby with meconium staining who is not vigorous, aspirate meconium from oropharynx with a 12-14 F suction catheter; then intubate and suction the trachea (not more than 3 – 5 sec) Supplemental oxygen In term NB, if resuscitation is started with less than 100% O2, supplemental O2 up to 100% should be administered if there is no appreciable improvement within 90 seconds following birth In preterm babies < 32 WGA, use of oxygen blender and pulse oximeter during resuscitation is recommended. Adjust O 2 concentration up or down to achieve oxyhemoglobin concentration that gradually increases towards 90% Positive Pressure Ventilation Indications o Apnea or gasping respirations o HR < 100 30 seconds after administering initial steps o Central cyanosis in spite of supplementary O2 Term NB require 15 – 25 ml/ ventilation (5 – 8 mL/kg) Initial peak inflating pressures of 30 – 40 cm H2O for term NB and 20 – 25 cm H2O for preterm NB is usually adequate; for subsequent ventilation of normal lungs, provide 15 – 20 cm H2O, and 20 – 40 H2O for diseased or immature lungs Primary measure for adequate ventilation is prompt improvement in HR Assisted ventilation (when not accompanied by chest compressions) should be delivered at 40 – 60 breaths per minute PEEP protects against lung injury in preterm infants; PEEP can be delivered with a T-piece resuscitator ET tube placement- indications: o Tracheal suctioning for meconium o Ineffective or prolonged B & M ventilation o Chest compressions are being performed o Endotracheal administration of medications o Special circumstances- CDH, ELBW (<1000 gm) Laryngoscope blade size: Term NB 1; Preterm NB 0; Extreme prematurity 00; straight blade is preferred Limit intubation attempt to 20 seconds Prompt increase in HR is the best indicator that the ETT is in the tracheobronchial tree; however exhaled CO 2 detection is the recommended method of confirmation Orogastric tube: Use 8 Fr feeding tube if prolonged PPV is required Chest compressions Indication: HR < 60 bpm in spite of adequate ventilation (with supplemental O2 for 30 seconds) Compression: Ventilation ratio should be 3:1, with 90 compressions and 30 breaths to approximately 120 events per minute (or 4 events per 2-second cycle; exhalation occurs during first compression after each ventilation) Drugs (Medications) Umbilical vein: 3.5 or 5 Fr catheter Epinephrine o HR < 60 bpm despite adequate ventilation (with 100% O2) and chest compressions o IV route is preferred; Dose: 0.1 – 0.3 mL/kg (0.01 – 0.03 mg/kg/dose) of 1: 10,000 (0.1 mg/mL) o ET route: 0.3 – 1 mL/kg (Up to 0.1 mg/kg) o May be repeated every 3 – 5 minutes Volume expander (isotonic crystalloid preferred) at 10 ml/kg over 5 – 10 min; may be repeated if necessary. If blood is needed, use O neg cross matched to mom Dinesh Thekke, MD Page 1 Ethics Naloxone o HR and color must be first restored by supporting ventilation o History of maternal narcotic administration within the past 4 hours o Preferred route is IV over IM (ET route is not recommended) o Dose: 0.1 mg/kg o Naloxone should not be given to babies of mothers suspected of having had long term exposure to opioids, or who are on methadone maintenance o Naloxone has a very short half-life; monitor baby to assess need for further doses Sodium bicarbonate o Should only be used only after ensuring that there is adequate ventilation o 4 mL/kg (2 mEq/kg) of 4.2% (0.5 mEq/mL) solution at a rate no faster than 1 mEq/kg/min Resuscitation is not indicated for: Extreme prematurity (GA < 23 wks or BW < 400 gms), anencephaly, chromosomal abnormalities not compatible with life (Trisomy 13) In conditions associated with high rate of survival and acceptable morbidity, resuscitation is nearly always indicated, This generally includes babies ≥ 25 WGA (unless there is evidence of fetal compromise such as intrauterine infection or hypoxia-ischemia) and those with most congenital malformations In conditions associated with uncertain prognosis, where survival is borderline, the morbidity is relatively high, parental desires concerning initiation of resuscitation should be supported After 10 minutes of continuous and adequate resuscitative efforts, discontinuation of resuscitation may be justified in infants without signs of life (no heart beat and no respiratory effort) Miscellaneous Normal VS of NB: Temp: 36.5 – 37.5 oC (97.7 – 99.5 oF) MAP = [DBP + (SBP – DBP)]; Keep MAP > GA of infant 3 ETT size (WGA/10) GA (WKS) WEIGHT (GRAMS) < 28 28 – 34 34 – 38 > 38 < 1000 1000 – 2000 2000 – 3000 > 3000 ETT SIZE 2.5 3.0 3.5 4.0 HR: 100-180 RR: 40-60 Suction catheter (Fr) 5–6 6–8 8 8 -10 Depth (from upper lip) (BW + 6) WEIGHT (Kg) DEPTH (cm) 1 7 2 8 3 9 4 10 7-8-9 rule for babies weighing 1-2-3 kgs Dinesh Thekke, MD Page 2 GESTATION vs. WEIGHT Weeks Grams 24 600 26 800 28 1000 30 1200 32 1400 34 1600 IUGR Weight increases by 100 gms/wk NB lose 10% (up to 15% in preterm babies) of their BW, and regain their BW by 10 – 14 days of life Correct for prematurity up to 2 yrs of age SGA <10th centile; severe IUGR < 3rd centile Placental insufficiency accounts for 70% of cases Long standing maternal Ty-1 DM causes IUGR (cf. gestational DM, which causes LGA) Catch-up growth possible in IUGR Early IUGR (1st trimester) - Symmetric IUGR Late (3rd trimester)-Asymmetric IUGR (Sparing of CNS) Genetically predisposed to be small- no pathology evident. So there is no potential for catch-up growth NEONATAL JAUNDICE 80 % of bilirubin is from breakdown of Hgb; the remaining is from other heme-containing enzymes Indirect bilirubin is fat-soluble, and therefore able to cross BBB, causing neurotoxicity Conjugated bilirubin is not normally reabsorbed from the GIT. Intestinal β-glucuronidase converts conjugated bilirubin to unconjugated bilirubin, which is reabsorbed and delivered back to the liver (Enterohepatic recirculation) Direct bilirubin = conjugated bilirubin + Δ bilirubin (conjugated bilirubin covalently bound to albumin) Clinically evident if > 5 mg/dl Direct bilirubin = Conjugated bilirubin + Delta bilirubin (i.e. bilirubin conjugated to albumin) Physiological jaundice There is a deficiency in bilirubin receptors in the liver up to DoL 4 High levels of intestinal β-glucuronidase, causing increased enterohepatic recirculation Decreased UDPGT activity, causing decreased conjugation Peaks in term babies at 3 – 5 days and in preterm babies, at 5 – 6 days Breast-feeding jaundice: Due to dehydration, usually in first 2-3 days of life Breast milk jaundice: Free fatty acids in milk compete with bilirubin for albumin binding sites. Maternal hormones (which also need to be conjugated in liver) also compete with bilirubin Pathologic jaundice Jaundice on DoL 1 Any elevation of serum bilirubin > 0.5 mg/dL/hr >12 mg/dl in term baby; >15 mg/dl in preterm babies Jaundice in a term baby beyond 8 days; jaundice in a preterm baby beyond 14 days ABO incompatibility: Mom O; baby A. Check direct Coomb’s test Causes for late onset (>1 week) of jaundice Breast milk jaundice (breast feeding need not be interrupted) G6PD deficiency Hypothyroidism Phototherapy Increase fluid intake by 10 ml/kg/for each PT light PT lights cause transient Lactase deficiency in intestinal brush border cells, causing diarrhea. This may actually be beneficial in getting rid of bilirubin that may otherwise be recirculated via entero-hepatic circulation Dinesh Thekke, MD Page 3 Term baby Preterm PT > 15 mg/dL > 0.5% of BW (Age in weeks/2)-5 Weight in gms/200 < 1000 gms > 5 mg/ dL > 1800 gms > 9 mg/ dL ET > 20 mg/dL > 1% of BW Age in weeks/2 > 10 mg/ dL > 18 mg/ dL IV FLUIDS/ TPN Keep Accuchecks to <150 mg% Glucose infusion rate (GIR) = Gms of Dextrose (5 or 10; not .05) x IV rate (cc/hr) [GIR= TF x D/144] 6 x Wt (kgs) Keep GIR 5 –8 mg/kg/min Insensible water losses: 20 – 40 ml/kg/day in term NB; < 26 WGA may lose as much as 100 ml/kg/day Excretion of renal solute load requires 25 – 50 ml/kg/day Stool losses assumed to be 5 ml/kg/day Electrolytes not usually required during first 24 hours > 2000 Gms Day 1: 80 cc/kg D10; Calcium 300-500 mg/kg/day (Ca 1 mEq ≈ 200 mg) Day 2 onwards: Increase by 20 cc/day every day to a maximum of 140 – 160 cc/kg/day; add Na 2-4 mEq/kg/day; K 1-3 mEq/kg/day <2000 Gms Day 1 Use D5 if <1000 gms (but if SGA then D10 may be used); D10 if > 1000 gms o <750 gms: 150 cc/kg/day o 750-1000 gms: 120 cc/kg/day o 1000-1500 gms: 100 cc/kg/day Increase by 20 ml/ kg everyday to a maximum of 180 cc/kg/day; day 2 Start TPN Proteins: Start at 0.5 g/kg/day, increase by 0.5 g/kg daily to a max of 3 g/kg/day (use Trophamine + cysteine). Proteins cause BE, pH and BUN. IL: Start at 0.5 g/kg/day, increase by 0.5 g/kg Q daily to a max of 3 g/kg/day (Start IL 1-3 days after initiation of TPN). Decrease or stop IL if TG > 200 (monitor at initiation and weekly). Reduce or stop IL if sepsis, hyperbilirubinemia (FFA in IL bind to albumin), Thrombocytopenia and severe respiratory distress are present Calculating TPN Use current weight for calculations, as TPN bag is usually hung up later in the day Determine Total fluid volume for 24 hours Subtract volume of enteral feeds, IL, transfusions, umbilical line flush; balance is fluid volume to be given by TPN Decide on % of D in TPN (Maximum concentration of dextrose tolerated in peripheral IV is 12.5%) Decide on gms of protein/kg (at EJGH, calculate gms of protein in 100 ml of TPN fluid; cannot be > 6 gms protein/100 cc) Lipids (20% IL): Determine amount of IL (gms/kg x Weight); multiply by 5 to obtain cc of IL. Infuse over 18-20 hours. Electrolytes, trace elements, Cysteine (Grams of protein/100 ml x 40), Zinc 400 mcg/kg/day, MVT Acetate and phosphate are buffers and may be used to counter metabolic acidosis Electrolyte abnormalities Hypoglycemia: (< 40 mg/dl): D10 2-4 ml/kg. Maintain GIR at 6-8 mg/kg/min Hyperglycemia: (>125 in term NB; >150 in preterm): Check GIR and decrease Dextrose concentration (but not below 2.5). May use Insulin 0.05 – 0.1 U/kg SC or IV Hypernatremia: Increase IVF by 20 – 40 ml/kg and decrease exogenous Na Hyperkalemia (> 7): 10% Ca-gluconate 1 ml/kg over 5 min (if EKG changes present); NaHCO3 (1-2 mEq/kg) over 5-10 min, Insulin 0.05 – 0.1 U/kg SC or IV (give D5 concurrently if blood glucose < 150) and Albuterol nebs. Hypokalemia ( <2.5) Give k-run 0.5 – 1.0 mEq/kg/dose at 0.5 – 1.0 mEq/kg/hr Dinesh Thekke, MD Page 4 Calorie count Use Birth weight for calculations until baby regains birth weight (usually 2 weeks) Thereafter, use previous day's weight (except for calculating TPN requirements, in which case, use current weight- as TPN bag is usually hung up later in the day) Kcal from Dextrose = Volume of TPN x %D (e.g. 0.10 for 10%D) x 3.4 Kcal from IL: Volume of IL x 2 Kcal from Formula: Oz x Calorie content of formula HMF: 1 pack to 50 cc = 22 cal/Oz; 1 pack to 25 cc = 24 cal/oz Polycose: 3.8 kcal/gm; MCT oil 7.7 kcal/cc; Microlipid 4.5 kcal/cc; Rice cereal 5 kcal/tsp TRANSFUSIONS Blood volume in term NB: 80 ml/kg; preterm 90 – 100 ml/kg Polycythemia is Hct >65 in venous blood Physiologic anemia: Term NB Hgb 11 at 8-12 wks; Preterm Hgb 7 – 9 at 4 – 8 wks (check reticulocyte count); transfuse if A’s or B’s or persistently elevated HR or lacking adequate weight gain Keep Hct >40 initially if baby is on MV; maintain at least 35 if on long standing MV, or needing significant O2 support 1 cc/kg of PRBC will raise Hct by 1 ( usual volume 10 – 15 ml/kg over 3 hrs) Do not use A-line for PRBC transfusions Neonatal isoimmune thrombocytopenic purpura: Mom is PLA-1 (-) and baby is PLA 1 (+). Transfusion of baby’s platelets into maternal circulation results in mother developing anti-PLA-1 Ab, which cross over into fetal circulation and attaches to baby’s platelets. These ‘marked’ platelets are then cleared by the spleen. The mother is not thrombocytopenic. IVH is a possible complication, so the baby is treated with maternal washed and irradiated platelets or IVIG. Neonatal autoimmune thrombocytopenia: Maternal IgG attacks both maternal and fetal platelets. Less likely to cause IVH Transfuse (10 cc/kg over 1 hour) platelets for Plt count <50,000. Check counts in 1 hour and again after 24 hrs FFP 10 ml/kg UMBILICAL CATHETERIZATION UAC There are 2 umbilical arteries and 1 vein Low-lying: L3-L4 intervertebral space (tip at bifurcation of the aorta, below the renal and mesenteric vessels). This is roughly 60% of the distance between the shoulder (lateral end of the clavicle) and the umbilicus High-lying: (tip at T6 – T10) may be preferred for its longevity and decreased incidence of catheter toes (a high lying UAC may be used by the cardiologist to identify a right sided aortic arch). “High” catheters are preferred over “low.” On the x-ray, UAC is seen dipping down before ascending up the aorta UA catheterization should not be performed if: Omphalitis, peritonitis, NEC, intestinal hypoperfusion Never use hypoosmolar fluids through UAC < 1000 gms: 2.5 F (single lumen only) > 1000 gms: 3.5 F (single/ double lumen)a Term NB: 5F (single/ double lumen)a Low: L3 – L4 High: T6 – T10 UAC If the diameter of the catheter is too large for the lumen of the aorta, there is an increased risk of vascular trauma, thromboembolism and vasospasm BW (kg) + 7 cm b [Wt (in kg) x 3] + 9b a Single lumen catheters provide better arterial blood pressure tracings. The (BP) transducer should be calibrated every time the line is sampled and if the fluids are changed. There can be +/- 10 mm Hg discrepancy between the cuff BP and the UAC BP. If the arterial trace is good, then the invasive reading should be considered more accurate b Add length of the umbilical stump Formula may not be appropriate for SGA/ LGA infants Dinesh Thekke, MD Page 5 UVC UVC is passed through the umbilical vein ductus venosus IVC. The tip should lie at the junction of the IVC with the right atrium (this lies at T9 – T10, just above the diaphragm on the x-ray). Placement of the catheter tip in the portal circulation is not acceptable On the x-ray, UVC shows a slight right deviation UVC < 1500 gms: 3.5F (single/ double lumen) Larger infants: 5F (single/ double lumen) (Length of high UAC/2) + 1 (Wt (kg) x 1.5) + 5.5 Add length of the umbilical stump Formula may not be appropriate for SGA/ LGA infants UVC complications Throughout insertion, the catheter must be kept filled with fluid and a closed 3-way tap attached. If the infant takes a deep inspiration, negative pressure may be generated and air drawn into the catheter which could result in air embolism Beware advancing a UVC too far across a PFO and into the left atrium, as accidental air emboli may then proceed to the cerebral circulation) A life threatening complication can include cardiac tamponade from infiltration of fluid; it can occur irrespective of proper positioning of the UVC, and must be treated with pericardiocentesis Until correct positioning of the UVC is documented in the x-ray, do not use it to infuse hypertonic solutions as direct intrahepatic administration of hypertonic solutions may result in hepatic injury and necrosis. An exception to this may occur in the delivery room, where emergent umbilical venous access may be needed during resuscitation. An UVC should be placed to a depth of 5 cms (3 cms in small babies), just until free blood flow returns Common complications of umbilical lines Vascular accidents (thromboembolic incidents involving the kidneys, bowel, legs, and rarely the spinal cord) Infection DIC Vessel perforation All these complications are indications for catheter removal Major landmarks T12: Diaphragm, Celiac artery L1: SMA, Renal artery L3: Inferior mesenteric artery L4: Aortic bifurcation Dinesh Thekke, MD Page 6 Procedure Measure length Cap on, wash, gown, gloves Open kit and display all contents Get a triple stop-cock and 3 single stop-cocks Clean umbilicus well with betadine and drape Draw up NS in 4 syringes Remove air from all syringes Remove air from all lines by flushing Remove air from stop-cocks Test cath ports' patency by attaching syringes; 1 to each port Dinesh Thekke, MD Put "stop" to main (white) - so won’t get blood leak via any port Lift up umbilicus and tie with a string (don’t catch skin) Tease out Artery and vein Pass cath For UAC, aim tip towards feet For UVC, aim tip towards right shoulder Check for back flow Suture- first anchor, then wind (no need for needle holder) X-ray (AP/Lateral): UAL T6-9; UVL 1 cm above liver Page 7 Dinesh Thekke, MD Page 8 INFECTIOUS DISEASES I = Myeloblasts+ Promyelocytes+ Myelocytes+ Metamyelocytes+ Bands I:T of > 0.15 represents shift to left; >0.2 implies sepsis; I:M > 0.3 is suggestive of sepsis ANC < 1500 is Neutropenia CRP usually done 8-12 hours after birth, and not immediately after birth LP only if +ve Blood Cx UTI is unlikely in first few days of life, ; Urine Cx for sepsis work up >3 DoL Both Ampicillin and Penicillin cross BBB, but only Ampicillin exerts synergistic action on Gentamicin to enable Gm also to cross BBB. Hence the combination of Amp-GM preferred AMPICILLIN CEFOTAXIME GENTAMICIN VANCOMYCIN < 28 DoL > 28 DoL < 28 DoL > 28 DoL < 29 WGA 30 – 33 WGA 34 – 37 WGA ≥ 38 WGA < 29 WGA 30 – 44 WGA mg/kg 100 100 50 50 5 4.5 4 4 10 - 15 10 - 15 Frequency Q12 Q8 Q12 Q8 Q48 Q48 Q36 Q24 Q18 Q12 1st week of life: Peak after dose 1; Trough prior to dose 2. Peak: 5 – 12 mcg/ml. Trough 0.5 – 1.0 mcg/ml 1st week of life: Trough prior to dose 2; peaks- especially if meningitis. Peak: 30 – 40 mcg/ml Trough: 5 – 10 mcg/ml MECHANICAL VENTILATION % of Oxygen delivered by nasal cannula FiO2 Rate (Lpm) 1.0 0.8 0.6 0.4 0.25 34% 31% 26% 22% 0.5 44% 37% 31% 24% 0.75 60% 42% 35% 25% 1.0 66% 49% 38% 27% Normal term NB ELBW Respiratory failure Wean pH 7.30 – 7.40 > 7.25 – 7.28 < 7.20 7.35 – 7.45 PaCO2 (mm Hg) 30 – 35 45 - 70 > 55 – 60 35 – 50 PaO2 (mm Hg) > 60 50 - 70 < 60 (while on O2) 60 – 80 FiO2 0.21 0.4 – 0.5 0.21 Base deficit (mEq/L) - 5 to 0 < -7 -5 to 0 SaO2 > 90 – 92 % 88 – 98 % < 85 % 92 – 95 % CBG: pH roughly parallels ABG values. PCO2 is about 5 mm higher in CBG, and PO2 is about10 mmHg lower Indications for instituting MV: ABG criteria o PaO2 < 50-60 in 100% O2 o PaO2 <60 in 40% O2 for babies <1250 gms o PaCO2 > 55-65, with pH <7.20 - 7.25 Clinical criteria o o o o Apnea/Bradycardia requiring resuscitation Unresponsive to CPAP Inadequate respiratory effort Shock and asphyxia with hypotension Initial settings: IMV 30-40 PIP 14 – 20 PEEP +5 FiO2 100% Normal (physiologic) PEEP is 2-3 cm H2O; use lower PEEP (0-2) for PIE PIP < 1kg: 14 cm H2O; 1-2 kg: 15-20 H2O; >2 kg: 20-25 cm H2O O2 Index: FiO2 x MAP x 100 / PaO2 Dinesh Thekke, MD It 0.35 – 0.5 sec Page 9 Oxygen saturations of 88-93% are acceptable in preterm babies Bicarbonate infusions o During resuscitation1-2 mEq/kg over 5 min o During mechanical ventilation if base deficit is greater than -7 [Base deficit x Wt (in kg) x 0.3] over 30 min. Correct half of this deficit initially and then reassess ABG Alkalosis is worse than acidosis (low PCO2 reduces cerebral blood flow) Heparinized specimen may show a metabolic acidosis ETT tip should be below level of clavicles and above carina Do not wean MAP until FiO2 < 60% Extubation criteria: IMV 8 – 10 PIP 13 – 15 PEEP 4 Specific circumstances RDS PEEP 4 – 5 cm H2O, PIP 18 – 25 H2O, Ti 0.35 – 0.5, Rate 30 – 60; pH 7.30 – 7.40, PCO2 40 -55, PO2 50 -70 PPHN Keep PCO2 low (35 – 40), PO2 75 -110 and pH alkaline (7.35 – 7.45). Increase rate (40 – 60) PO2 high (>60) and low PEEP (2 cm H2O); (and low It for MAS) MAS PIE PCO2 may be higher (use lower PIP), low PEEP (0 -1), low It (0.1 – 0.2) and higher rates (60 – 120); Consider HFOV RATE PIP PEEP It CHANGE pCO2 (↑PEEP causes shunting & V/Q mismatch) -To CO2: Increase rate, PIP. Decrease PEEP. pO2 -- To O2: increase FiO2, PEEP, It and PIP ↑ in CO2 by 10 reduces pH by 0.08 Volume Control ventilation: Do not use VC mode for babies < 2 kg (cannot ensure precise TV). PC (+ PS) is preferred for these babies PEEP reduces TV, while PIP increases TV Exhaled TV is a better indicator of true TV than inhaled TV HFOV Frequency (Hz): <1 kg: 15 Hz 1-2 kg: 12 Hz 2-10 kg: 10 Hz MAP= MAPIMV +2; start at about 10 cm H2O ΔP (Amplitude): PIP (on CMV) will be ΔP. Start ΔP at 12 (usually MAPIMV x 2), and look for enough 'umbilical jiggle.' Go up in 3's. Never let ΔP be more than 3 x MAP Increased jiggle correlates with CO2 removal Expansion [no. of ribs (9-10)] indicates oxygenation Changes in blood gases will be seen only 4-6 hrs after starting HFOV Wean from HFOV TO CMV if MAP 12 Get CXR Q6H while on HFOV Frequency (3-15 Hz; ≈ 180 – 300 bpm) MAP ΔP (Amplitude = PIP – PEEP) Dinesh Thekke, MD CHANGE PCO2 -- To remove CO2: Increase ΔP, decrease Hz PO2 -- --- Page 10 Sedation during MV Fentanyl o Infusion 1 – 5 mcg/kg/hr o Bolus 1 – 4 mcg/kg/ dose (Q2 – 4 H) Midazolam o Infusion 0.01 – 0.06 mg/kg/hr o Bolus 0.05 – 0.15 mg/kg/dose (Q2 – 4H) Vecuronium (Norcuronium) 0.03 – 0.15 mg/kg (Q1 – 2H); Pancuronium (Pavulon) 0.04 – 0.15 mg/kg (Q1 – 2H) RDS: Lung maturity L/S PG <2 Immature >2 Transitional >2 + Mature Apnea of prematurity Usually occurs in < 34 WGA or < 1800 gms Obstructive apnea: No A’s (monitor interprets struggling movements of the baby to be respiratory movements), but there will be B’s and D’s Caffeine: Desired level 5 – 25 mcg/ml Do MCP if caffeine needed on discharge. Arrange apnea monitor if abnormal MCP Xopenex dose: 0.1 mg/ kg Kg 0.5 ml (0.63 mg/3 ml) 0.2 1.0 0.5 1.5 0.7 2.0 1.0 2.5 1.2 3.0 1.5 3.5 1.7 NURSERY ISSUES Wean to open crib by 32- 34 weeks (>1800 gms) <32 WGA: No gastric acidity- so questionable role for Ranitidine in treatment of Reflux in this age group Prior to discharge, ensure/ arrange for: NBS, BAER, Immunizations/ Synagis, PCP, Developmental clinic, CPR training to caretakers, RoP follow up, HUS (if indicated), MCP (if on caffeine), car seat test (for babies < 37 WGA), circumcision NBS must be performed after at least 48 hrs and while baby is on a protein containing diet Preterm babies need their first Head USS at 3-7 DoL (unless clinically indicated earlier) Eye exams (RoP surveillance) Initially done at 4-6 wks of life, and followed up every 2 weeks thereafter o Prescribe Phenylephrine 2.5%/Tropicamide 0.5% 1 gtt both eyes q5 minutes x 3 30 minutes prior to examination o Retinal vascularization is complete at 34 WGA; so no RoP in babies born after 34 weeks For preterm babies being fed enterally, start PolyVisol with Iron on DoL 14. Start with 0.5 ml Q12H and switch to 1 ml Q-Daily when the baby attains 2 kgs. Start iron after 4-8 weeks of age (elemental iron 2 mg/kg/day) Nutrition Nippling not developmentally possible until 34 WGA ( 1650 gms) 120 Kcals/kg/day [BMR 50, Growth 25, GI 20 (Digestion/Absorption 12; Stool losses 8), Cold stress 10, Activity 15] To attain 120 Kcals/kg o 180 cc/kg of 20 cal/oz formula (Breast milk 20 Kcals/oz) o 160 cc/kg of 22 cal/oz formula o 150 cc/kg of 24 cal/oz formula Add HMF after 2nd week of life, or when baby is tolerating full volume feeds (for weight/ GA) HMF: 1 pack to 50 cc = 22 cal/Oz; 1 pack to 25 cc = 24 cal/oz Polycose: 3.8 kcal/gm; MCT oil 7.7 kcal/cc; Microlipid 4.5 kcal/cc; Rice cereal 5 kcal/tsp Weight gain should be 10-15 gm/kg/day Infants <1200 gm usually do not tolerate bolus feeds, and hence are usually placed on continuous feeds. (Bolus feeds may be attempted for infants >1200gm) Hold feeds if residuals > 30% of bolus feeds or >1.5 times rate of continuous feeds Dinesh Thekke, MD Page 11 NECROTIZING ENTEROCOLITIS Management: IVF,NPO, OG tube to gravity (to suction if abdomen distended); KUB and cross-table lateral Q6H until stable; heme test all stools, serial CBC, stool Cx; Abx- Amp/ Gm if not on abx; add Vancomycin or 3rd generation Cspn if already on abx; if perforation suspected, add Metronidazole. If there is evidence of peritonitis/ perforation, consult surgery It is safe (from NEC view point) to increase enteral feeds by 20 – 25 cc/kg/day. Slowly build up from continuous feeds to bolus feeds. Increased osmolarity of feeds (TPN/Enteral) causes cellular dehydration. Neuronal dehydration predisposes to IVH and enterocyte dehydration predisposes to NEC Average age at diagnosis < 30 WGA: 20.2 days FT: 2 days MISCELLANEOUS Vitamin K: < 30 WGA 0.5 mg (IM) > 30 WGA 1.0 mg (IM) Do HUS in 1st week of life for babies < 34 WGA (usually on DoL 3, and then repeat 1 week later) Hydrocephalus: < 2kgs: EVD >2 kgs: VPS Indomethacin: 1st dose 0.2 mg/ kg (IV over 30 min; 2nd & 3rd doses ( at 12 and 36 hrs after 1st dose) 0.1 mg/kg/dose (if BW <1250 gms and < DoL 7); 0.2 mg/kg/dose (if BW >1250 gms or > DoL 7) Only if Urine output > 1 cc/kg/hr, BUN < 30, Creatinine < 1, Plts >150, Check these prior to each dose. Must be NPO Glucagon causes calciuria Admitting orders Admit to NICU Diagnosis Condition Under radiant warmer with CR monitor and pulse ox Nursing: Vitals Q2H; Accurate I & O; daily weight IVF NPO Medications Labs (CBC on admission, BMP 12 hrs after delivery; CBG on admission (ABG after central line is placed), CXR now and in morning, blood type and Coomb’s test, Blood Cx Ventilator settings Presentation during rounds: DoL/CGA/ Weight (Up or down)/ Enteral feeds- Type, Rate and calories, IVF/TPN- type, rate and calories, Total intake (cc/kg/day), Total calories-(kcal/kg/day), Urine output (cc/kg/hr), Stools, Residuals, ABD's, Medicines/Abx, CBG, Labs, Radiology, Plan. Dinesh Thekke, MD Page 12 RADIOLOGY TTN is represented on the CXR by a pattern of central pulmonary edema or mildly increased interstitial markings with a normal cardiac silhouette. Radiological changes rapidly clear within 24-48 hrs MAS results in alternating pattern of atelectasis and over inflation. Inflammatory reaction to the meconium results in a progressive increase in interstitial markings. A similar appearance is found in neonatal pneumonia. In BPD, the ground glass appearance of RDS will eventually give way to a coarse cystic pattern. Chronic BPD is characterized by interstitial fibrosis with scattered areas of both atelectasis and hyperinflation. PIE resembles coarse BPD, but is characterized by a sudden dramatic radiographic appearance. There are irregular radiating ‘tubes’ of air that do not taper peripherally (tapioca pudding) Chylothorax in a neonate is invariably right sided A neonate with multiple air-filled cysts in the chest could have CCAM or CDH (when there is no gas in the abdomen). Diaphragmatic hernias are more common on the left (the liver prevents right sided hernias from recurring) NEC: The most common radiographic appearance is a normal appearance of the abdomen. The earliest abnormality noted is bowel distension with bowel wall thickening. Pneumatosis intestinalis is usually first seen in the RLQ and the flanks. Air outlining the falciform ligament gives rise to the football sign of pneumoperitoneum. Decubitus positioning (right side up) can be used to detect small air leaks in the abdomen. The air appears over the liver, and small triangular pockets of air are seen trapped between the flanks and the bowel walls. Eventually air enters the portal system and is seen radiographically as lucency overlying the liver. Meconium ileus: Distant small bowel obstruction in a newborn, accompanied by multiple small bubbles in the RLQ (soap bubble appearance) is pathognomonic of meconium ileus. Diagnosis is confirmed by contrast enema (A hypertonic agent (Gastrograffin) remains preferable because of its tendency to draw fluid into the lumen and lyse the meconium plug. However, dehydration can occur with repeated or prolonged use) A microcolon occurs when a small bowel obstruction is in the distal ileum. Flocculent calcification in the peritoneum is pathognomonic of meconium peritonitis secondary to meconium ileus and resultant perforation. Scrotal calcification may also be seen if the processus vaginalis was patent at the time of the perforation. TEF: A dilated proximal esophagus with air in the stomach is consistent with proximal esophageal atresia with a distal fistula, the most common type of TEF. A nasogastric tube that coils in the proximal esophageal pouch confirms the diagnosis. Intracranial hemorrhage: Grade I: Confined to the subependymal germinal matrix, over the caudate nucleus, and extends posteriorly to the choroid plexus Grade II: Extension of the bleed into the ventricles Grade III: ventricular dilatation Grade IV: Bleeding into the brain parenchyma On ultrasound, blood is echogenic, like the choroid plexus. Marked echogenicity near the lateral ventricles may be secondary to PVL (secondary to hypoxemia). CT is often the only way to differentiate between the two conditions. PVL is almost always peritrigonal and is initially echogenic. Small cysts coalesce to form larger cysts as the brain parenchyma degenerates. Eventually cysts may scar down and irregular ventricular dilatation may be the only residual sign. Dinesh Thekke, MD Page 13