CritupdateISOMarch2009Temlate (4) (2)
advertisement
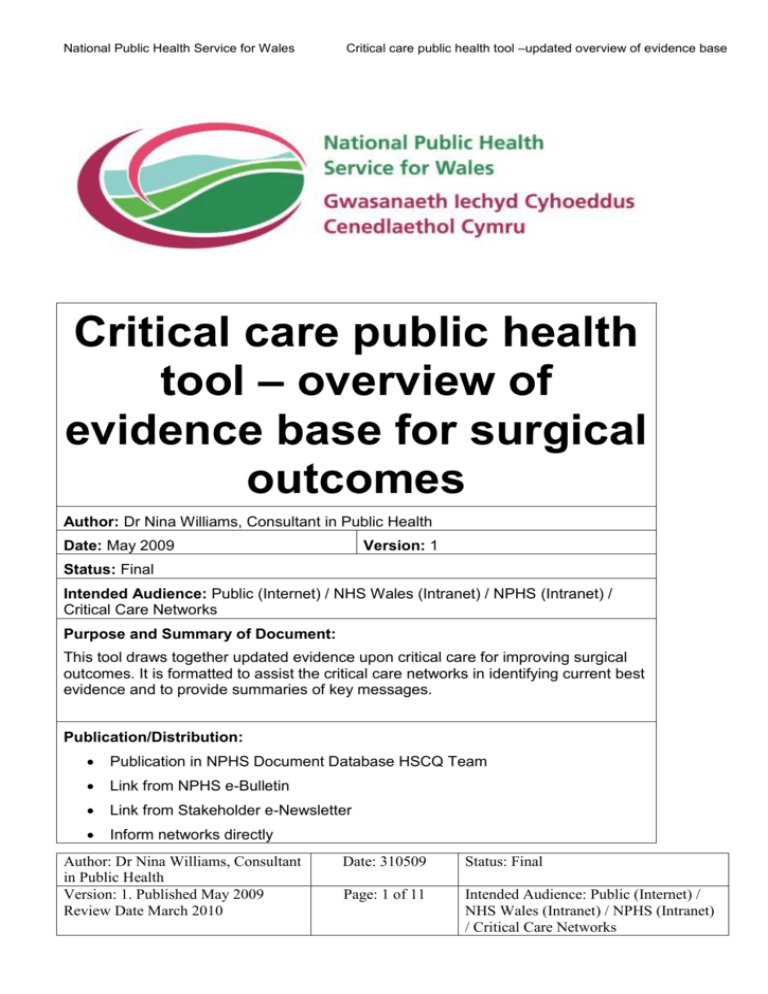
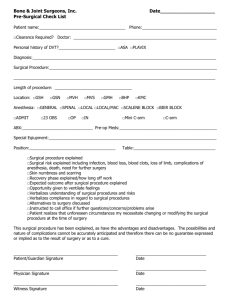
National Public Health Service for Wales Critical care public health tool –updated overview of evidence base Critical care public health tool – overview of evidence base for surgical outcomes Author: Dr Nina Williams, Consultant in Public Health Date: May 2009 Version: 1 Status: Final Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Purpose and Summary of Document: This tool draws together updated evidence upon critical care for improving surgical outcomes. It is formatted to assist the critical care networks in identifying current best evidence and to provide summaries of key messages. Publication/Distribution: Publication in NPHS Document Database HSCQ Team Link from NPHS e-Bulletin Link from Stakeholder e-Newsletter Inform networks directly Author: Dr Nina Williams, Consultant in Public Health Version: 1. Published May 2009 Review Date March 2010 Date: 310509 Status: Final Page: 1 of 11 Intended Audience: Public (Internet) / NHS Wales (Intranet) / NPHS (Intranet) / Critical Care Networks Critical care – evidence update: Improving surgical outcomes Critical care - overview of the evidence base for improving surgical outcomes This is one of series of regular evidence updates, which are undertaken by LKMS as part of NPHS support to the All Wales Critical Care Advisory Group. The aim is to “research and identify the evidence base for the best practice and new technology for the management of critically ill patients based on a strong national and international evidence base.” 1 A systematic search methodology is followed so the results are easily updated and reproducible. Details of full methodology, search results and literature review are available from LKMS.2 The initial searches identified very few papers of high quality evidence (systematic reviews, RCTs and meta-analyses). Most are single centre primary research studies. The focus is on outcomes in terms of ICU quality measures like average length of stay, ICU mortality, patient/family satisfaction, sub optimal pain management, effectiveness and cost effectiveness, care bundle compliance e.g, prevention of ventilator associated pneumonia, rate of infections related to instrumentation. Intervention Reference Comment Improving surgical outcomes 1. Improving Surgical Outcomes Group. Modernising care for patients undergoing major surgery: improving patient outcomes and increasing clinical efficiency. London: ISOG; 2005. The Improving Surgical Outcomes Group [ISOG] reports1,2 were reviewed and selected as key documents as they identified three key areas for improved outcomes, which were indicated as having the most impact on patient outcomes in terms of numbers and effective use of 1 Designed for Life: Quality requirements for adult critical care in Wales. EH/ML/008/08 2 LKMS, National Public Health Service for Wales, NPHS, 36, Orchard St, Swansea. 01792 607331 Email : LKMS Author: Dr Nina Williams, NPHS 2 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Type III evidence 2. Improving Surgical Outcomes Group. Modernising care for patients undergoing major surgery: implementation guide. London: ISOG, 2007. Type III evidence Comment critical care. Further searches were undertaken to focus and update the evidence on more specific questions. These were limited to papers published 2004-2008, updating evidence cited in the ISOG reports. The three areas are: 3. National Confidential Enquiry into Perioperative Deaths. The 2002 report of the National Confidential Enquiry into Perioperative Deaths. London: NCEPOD; Author: Dr Nina Williams, NPHS 3 Improved pre-operative assessment including lifestyle improvement’ such as, smoking cessation Improved peri-operative care Improved post –operative care Summary of the main evidence for improving outcomes for patients undergoing major surgery May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference 2002. 4. National Confidential Enquiry into Perioperative Deaths. The 2003 report of the National Confidential Enquiry into Perioperative Deaths. London: NCEPOD; 2003. Type III evidence Pre-operative Author: Dr Nina Williams, NPHS Comment “Many patients die within 30 days of surgery do so in general wards without being admitted to critical care. Of these, the vast majority have significant comorbidities at time of surgery like a coexisting cardiovascular or respiratory pathology. About 42 % of patients who died following surgery had pre-operative assessment scores recorded as ASA (American Society of Anaesthesiologists Score) of 3 or less which suggests that the severity of the illness and actual risk of death was not fully appreciated in the preoperative assessment.3,4 Subjective assessment underestimated the risk of death for patients undergoing surgery where the surgeon’s assessment was compared to physiological and operative severity scores5” 5. McCullogh P. Mortality and morbidity in Improved Pre-Operative Assessment, gastro-oesophageal cancer surgery. BMJ Triage and Preparation 2003;327:1192-196. 4 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Comment Objective evaluation of individual risk e.g. Cardio-pulmonary exercise 6. Lee J, Chaloner E, Hollingsworth S. The (CPX) testing has been shown to role of cardiopulmonary fitness and its determine pre-operative fitness and genetic influences on surgical outcomes: correlates well with post-operative review. Br J Surg 2006;93:147-57. survival Use of CPX enables triage of patients to general ward, HDU or ICU for immediate post-operative period CPX testing can identify those patients unfit for major surgery or should undergo a less risky operation In addition to above report: central to post-operative outcome is the ability to increase cardiovascular output in response to increased oxygen demand associated with major surgery. Genetic factors can influence by increasing oxygen demand further. Both CPX testing and identification of such genetic predisposition may have a role6. Author: Dr Nina Williams, NPHS 5 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Comment Optimisation Haemodynamic optimisation – avoids preoperative dehydration and poor perfusion to major organs through use of standardised fluid and electrolyte replacement regimes Smoking cessation 7. Moller A, Tonnensen H. Risk reduction: perioperative smoking intervention. Best practice and research. Clinical Anaesthesiology 2006; 20:237-48. 8. Theadom A, Cropley M. Effects of preoperative smoking intervention on incidence and risk of intraoperative and post operative complications in adult smokers: a systematic review. Tob Control Author: Dr Nina Williams, NPHS 6 Nutritional supplementation Short period on ICU for very high risk patients to obtain pre-operative cardiovascular optimisation Exercise In addition Smoking Cessation - longer periods of smoking cessation e.g. 6-8 weeks before surgery can reduce post– operative complications and improves wound healing7,8 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference 2008; 10:407-12. Comment Type I evidence Furlong C. Preoperative smoking cessation.A model to estimate potential short term health gain and reductions in length of stay. London: LHO; 2005 Peri-operative care Improved Peri–Operative Care Author: Dr Nina Williams, NPHS This report builds on the literature review published in early 2005 on the impact of preoperative smoking cessation on the outcomes of surgery. It models the effects of a systematic preoperative smoking cessation intervention for elective surgical patients for all London PCTs and for all London acute hospital trusts. 7 Haemodynamic optimisation (accurate fluid intervention) guided by a cardiac output algorithm can significantly reduce both rates of complications, mortality and significantly reduces length of hospital stay Patient warming during surgery, May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Comment beta blockade, higher supplemental inspired oxygen and optimised administration of blood products also show benefit Post-operative care Improved Post–Operative Care Author: Dr Nina Williams, NPHS 8 Level of post-operative care appropriate to patient’s assessment and current condition e.g. overnight intensive recovery unit (OIRU), separate post—operative critical care facility 2 Improvements in intra-operative care and increasing planned critical care admission for those at increased risk of complications reduces ICU and HDU bed days Outreach critical care focused on monitoring and providing care for surgical patients and HDU where it does not already exist May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Work in progress Reference 9. Intensive Care Society. Perioperative critical care criteria in adults. (Unpublished, work in progress) Comment Progress on guidance for appropriate elective surgical admissions to level 2 and level 3 critical care Further work in this area is being taken forward by the Intensive Care Society in “Perioperative Critical Care Criteria in Adults”9 which is still draft and not ready for publication. The document has been commissioned by the Standards Committee of the Intensive Care Society. The aim is to produce a set of objectives, easily applied, clinical criteria to provide guidance for clinicians and to increase standardisation of provision. Example of local practice guideline Author: Dr Nina Williams, NPHS Hope D. Suggested current elective These guidelines are intended to cover admissions to critical care units – a local most planned admissions. Individual cases view. may need to be discussed with the Critical Care Consultant if admission is thought to be of benefit. 9 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Comment Appropriate elective surgical admissions to critical care: evidence briefing for AWCCG. Swansea: NPHS; 2009. Surgical Factors o o o o o Major vascular surgery e.g. Abdominal Aortic Aneurysm Repair, major vessel grafting Major head and neck surgery e.g. neck dissection, laryngectomy, glossectomy, mandibulectomy Major Gastrointestinal surgery e.g. gastrectomy, pancreatectomy, obesity surgery Major neurosurgery e.g. craniotomy, aneurysm clipping, evacuation intracerebral haematoma Major thoracic surgery e.g. thoracotomy. Medical Factors Patients with severe co-morbidities at high risk of deterioration in the peri-operative Author: Dr Nina Williams, NPHS 10 May 2009 Review date: March 2010 Critical care – evidence update: Improving surgical outcomes Intervention Reference Comment period e.g. acute or chronic respiratory or renal disease. heart, Pain Control Patients who are likely to benefit from epidural/spinal analgesia and who cannot be cared for safely on general wards. CONCLUSION There is still ongoing work in this area but there is evidence behind assessing the risk to patients and improving outcomes for patients undergoing surgery that requires a combined multi-disciplinary approach between surgical and anaesthetic teams which is more than just saying which types of surgery require what level of care. The development of guidance for appropriate surgical admission to level 2 and level 3 critical care should take this evidence into account. Author: Dr Nina Williams, NPHS 11 May 2009 Review date: March 2010