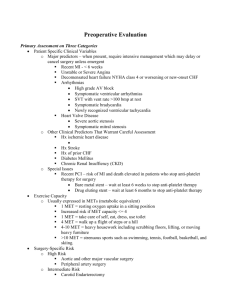
Univariate preoperative predictors of walking capacity, symptom
advertisement

Appendix 3 A. High quality studies (n=7) B. Randomized controlled trials (n=1, HQ one) C. Low quality studies (n=13) A. 'High quality' -studies including predictors for postoperative outcome of operated LSS Abbreviations: Superscript “a”= quality percent. N=number of patients. F=latest follow-up. LSS=lumbar spinal stenosis. HNP=herniated nucleus pulposus. q=amount of questions (in used questionnaire). mo=month(s). Details of each study are presented as above ____________________________________________________________________________________________________________________________________________ Author (year)a i) = study design ii) = intervention iii) = outcome measures Reported prognostic factor(s) Influence on outcome Study title, N, F Objectives ____________________________________________________________________________________________________________________________________________ Frazier (1997)62% i) Observational study ii) Laminectomy, medial facetectomy when necessary. 23% had concomitant arthrodesis with or without instrumentation iii) Questionnaires by Stucki et al. 1996 including back/leg/overall pain, and difficulty ambulating using Likert-scale from 1 (best) to 5 (worst); walking capacity (5q); satisfaction (6q) Greater preoperative scoliosis Associated with back pain (p<0.05, r= -0.29 (6 mo), Associations between spinal deformity To examine associations r= -0.25 (24 mo)), not with satisfaction, leg pain and outcomes after decompression for between radiographic or walking capacity spinal stenosis parameters (scoliosis and The extent of preoperative spondylolisthesis Iversen (1998)62% N=90 olisthesis) and outcomes of F=2 years surgery for degenerative LSS NS i) Observational, multicenter study ii) Decompressive surgery for LSS (23% one-level, 33% two-level, 44% ≥3 levels; arthrodesis for 29%) iii) Functional status (Sickness Impact Profile), walking capacity (4 q), pain (6-point scale), postoperative resource use; satisfaction with pain relief (4q) and physical function (2q) Preoperative expectations (e) The prognostic importance of patient To a) relate patient expectations -greater number of e:s Associated with improved global function (p=0.003) preoperative expectations of surgery for of surgery to baseline -more e:s with pain relief Associated with more pain (p=0.009) lumbar spinal stenosis. function and pain N=257 b) determine how patients F= 6 months expectations and preopera- Higher baseline pain Associated with more pain (p=0.003) Baseline depression -"- (p=0.003) Better baseline global function Better global function Fewer comorbidities Better walking capacity -"- (beta=0.5, p=0.0001) predict postoperative (beta=0.06; p=0.005) outcome Better walking capacity (p=0.0001) Younger age -"- (p=0.0006) Male gender -"- (p=0.003) Higher baseline walking capacity tive function interact to Better satisfaction with walking capacity (p=0.0001) Female gender -"- (p=0.025) More ambitious expectation of physical function -"- (p=0.043) Javid (1998)62% i) Observational study ii) Decompressive laminectomy; bilateral laminectomy and medial facetectomy for LSS (n=86; fusion for nine patients) and LSS with HNP(n=61). 23 patients had lateral stenosis iii) Pain, satisfaction, clinical examination, employment. Diagnoses as predictive factors: LSS vs. LSS+HNP NS (6week; 6mo; 1 yr; and 1-11year follow-ups) Long-term follow-up review of patients To evaluate long-term Lateral stenosis vs. (LSS+HNP, LSS) NS (lat. stenosis: a trend with inferior result) who underwent laminectomy for lumbar results (of surgery) in Obesity and sex NS (at 1-year follow-up) stenosis: a prospective study patients with symptomatic N=170 spinal stenosis F=11 years Jönsson (1993a)62% i) Observational, consecutive study ii) Decompression without fusion in secondary operation iii) Neurological examination, pain back/leg (4-scale), effect of work, consumption of analgesics, walking capacity In previous operation, 28 lumbar spinal stenosis patients had had decompression (two had also arthrodesis); Repeat decompression of lumbar nerve To find prognostic factors 65 discectomy; diagnosis at the repeat operation were: central LSS (cent) in 20, lateral LSS (lat) in 19, roots; a prospective two year evaluation which could be applied for disc herniation (DH) in 19 and periradicular fibrosis (PRF) in 35 patients F=2 years second surgical procedure Limitation : Diagnoses are based partially on operative findings, being thus peroperative predictors of spine; to report Diagnosis of reoperation Significant better results in patients, who had prolapse epidemiology of recurrent or LSS versus PRF (p=0.0001) or residual pain in study Single root affection (due to DH/lat) population vs. central LSS Better results in single root affection (P=0.0006) Age, gender, type of work NS Jönsson (1994b)85% i) Observational, consecutive study ii) Lumbar nerve root decompression iii) Pain (back/leg separately; 4-grade scale), walking capacity, neurological examination, employment Long preoperative duration of Worse long-term results (p=0.036) Decompression for lateral lumbar Surgical results and impact on low back pain and sciatica in lateral stenosis stenosis - Results and impact on sick leave and working conditions (subjective evaluation excellent/good/fair/poor ) sick leave and working conditions in patients who underwent surgery N=100 for lateral spinal stenosis were F=2 years evaluated in prospective, Type of work No influence on surgical outcome (sedentary/moderate/heavy) More sedentary workers returned consecutive study to their previous work (p=0.013) Jönsson (1997)77% i) Observational consecutive study ii) Laminectomy (20% one level, 45% two-level, more 35%; no fusion) with a facet-preserving technique; operation procedure extended laterally to identify each nerve root iii) Patient´s opinion of the outcome, with opinions regarding back and leg pain separately (4 grade scale); walking ability estimation (improved/not improved); pain at rest/night Pronounced stenosis of the spinal Significant correlation with a favourable outcome canal (ant-post diameter 6mm) Comorbid disorder affecting Significantly worse outcome walking ability Duration of sciatica-claudication symptoms <4 years Tendency toward better outcome (not significant) Insignificant lower back pain Age, gender -"NS A prospective and consecutive To evaluate the result after study of surgically treated lumbar surgical decompression for LSS, spinal stenosis - Five year follow at regular intervals after surgery, up by an independent observer and to correlate these results with N=105 values for preoperative parameters; F=5 years special interest was focused on the results in relation to the degree of constriction of the spinal canal Katz (1999)69% i) Observational study ii) Laminectomy with or without arthrodesis for degenerative LSS iii) Walking capacity, symptom severity, satisfaction measured by multi-item questionnaire (Stucki et al. 1996) Multivariate model (B=standardized beta coefficient) Better self-rated health Less cardiovascular comorbidity Better walking capacity _ Better walking capacity (B 3.8; p=0.002) Predictors of surgical outcomes in To identify outcome predictors of Less severe symptoms (B 3.6; p=0.0005) degenerative lumbar spinal stenosis surgery for degenerative LSS Better satisfaction (B 3.3; p=0.001) N=199 Better walking capacity (B 2.7; p=0.008) F=2 years Less severe symptoms (B 2.6; p=0.01) Better satisfaction (B 3.7; p=0.0002) Better walking capacity (B 2.5; p=0.01) No values for symptom severity and satisfaction Better mental health (3-item scale) Less severe symptoms (B 2.3; p=0.02) Better satisfaction (B 1.9; p=0.05) No values for walking capacity Higher income Better walking capacity (B 2.2 (0.03) Less severe symptoms (B 2.4; p=0.02) Better satisfaction (B 1.9; p=0.05) Univariate preoperative predictors of walking capacity, symptom severity and satisfaction 24months after surgery___________________________ (NS=not significant; SP=Spearman correlation; Wc=walking capacity; Sy=symptom severity; Sat=satisfaction) Continuous predictors and outcomes Age NS (SP=0.06-0.14 in Wc, Sy and Sat) Walking capacity Wc:SP=0.30, p<0.0005; Sy: SP=0.20, p<0.005; Sat NS, SP=0.08 Symptom severity Wc:SP=0.24, p<0.0005; Sy: SP=0.25, p<0.005; Sat NS, SP=0.08 Overall comorbidity Wc: SP= 0.33, p<0.0005; Sy:SP=0.27, p<0.0005; Sat: SP=0.23, p<0.005 Cardiovascular comorbidity Wc: SP=0.30, p<0.0005; Sy:SP=0.0.24, p<0.005; Sat: SP=0.25, p<0.0005 Musculoskeletal comorbidity NS (SP=0.13-0.17) Social support scale NS (SP=0.01-0.03) 3-item depression scale Wc:SP=0.19, p<0.005;Sy:SP=0.29, p<0.0005;Sat:SP=0.25, p<0.0005 Mean outcomes associated with categorical predictors (Outcomes: 0=the best, 100=the worst)_______________________________________________ Baseline predictor Male/female NS No college/some college education NS Income< $15,000 $15,000-50,000 NS $>50,000 NS Leg pain>back pain NS Back painleg pain NS Pinprick sensation normal or abnormal NS Lower extremity weakness NS Normal strength NS Radiological findings -scoliosis<15 NS -scoliosis15 NS -spondylolisthesis5mm NS -spondylolisthesis<5mm NS Wc Sy Sat (p<0.0005) (p<0.005) NS Self-rated health: -Excellent -Good, fair, poor (p<0.0005) NS (p<0.0005) (p<0.0005) B. Randomized controlled trial (HQ) including predictors for postoperative outcome of operated LSS (n=1) Abbreviations: Superscript “a”= quality percent. N=number of patients. F=latest follow-up. LSS=lumbar spinal stenosis. HNP=herniated nucleus pulposus. q=amount of questions (in used questionnaire). mo=month(s). _____________________________________________________________________________________________________________________________ _______________ Author (year)a i) = study design ii) = intervention iii) = outcome measures Reported prognostic factor(s) Influence on outcome Study title, N, F Objectives ____________________________________________________________________________________________________________________________________________ Amundsen (2000)69% i) 19 patients with severe symptoms were selected for surgical treatment, and 50 patients with moderate symptoms for conservative treatment; 31 patients were randomized between conservative (n=18) and surgical (n=13) treatment groups ii) Surgical treatment: standardized for the purpose of nerve decompression by partial/total laminectomy, medial facetectomy, discectomy, and/or removal of osteophytes from the vertebral margins or facet joints. One-level 8%, two-level 52%, three-level 29%, four-level 11%. No fusions. Postoperatively, a hyperextension thoracolumbar orthosis was used and after 1 week, the patients were transferred to the rehabilitation department for a period of 1 month. Sitting was not allowed during this period. No specific physiotherapy was given except instructions and “back school”. Conservative treatment: The same type of orthosis as above was fitted, and transfer to the rehabilitation department for 1 month was done. The orthosis was worn during the day for all activities, and patients were encouraged move around normally. No specific physiotherapy was given except instructions and “back school”. The patients were observed daily by the physiotherapists and three times a week by a physician. After 1 month (both groups), the patients were discharged from the hospital. Further treatment was identical for both groups consisting of wearing the orthosis for 2 more months. After that, physiotherapy started which consisted of general physical training. No attempt was made to improve mobility of the spine, and the patients were instructed to try holding the back in a slightly kyphotic position iii) Pain (verbally, visual analogue scale); claudication distance, effect of bending forward/backward; employment status; neurological examination; subjective evaluation (better/worse/unchanged); the changes were recorded. The overall result was summarized according to the aforementioned data (excellent/fair/unchanged/worse) Clinical predictors Predictors for the final outcome were not found Lumbar spinal stenosis: Conservative or surgical treatment? To identify the short and long-term - physical findings - Lasegue's sign N(surgical)=32 conservative treatment and - level of spinal protein N(conservative)=68 followed for 10 years F=10 years Radiologic predictors (see text for details) NS - multilevel afflictions NS - advanced degenerative changes NS Advanced age NS Gender NS Married/not married NS Type of work NS Physical loading NS Satisfaction at home and work NS Duration of pain NS Length of sick listing NS Level of physical activity NS Smoking habits NS results after surgical and C. 'Low quality' prospective studies including predictors for postoperative outcome of operated LSS (n=13). Abbreviations: Superscript “a”= quality percent. N=number of patients. F=latest follow-up. LSS=lumbar spinal stenosis. HNP=herniated nucleus pulposus. q=amount of questions (in used questionnaire). mo=month(s). ____________________________________________________________________________________________________________________________________________ Author (year)a i) = study design ii) = intervention iii) = outcome measures Reported prognostic factor(s) Influence on outcome Study title, N, F Objectives _____________________________________________________________________________________________________________________________ _______________ Gunzburg (2002)38% i) Observational consecutive study ii) Partial laminectomy/arthrectomy iii) Functional status: Waddell Disability Index, (Low Back Outcome Score); VAS; reduction of pain during walking, reduction of leg pain. Also, the satisfaction of hospital stay, operation, and the wish to have the same operation again was asked Illness behaviour Gender was concluded to play an important role in surgical outcome Clinical and psychofunctional Conclusion was based on higher-than-expected-rate of non- measures of conservative The aim of the study was to organic signs -score pre- and postoperatively decompression surgery for lumbar evaluate short-term psychometric spinal stenosis: A prospective cohort study. and functional outcomes after conservative decompression No statistically differences between subgroups Operative age (with respect to satisfaction/wish to have same N=40 Stenosis classification operation again) F= 1.7yrs (mean; range 1-2.6) Herkowitz (1991)46% i) Comparative, consecutive study ii) Decompressive laminectomy (n=25), or decompressive laminectomy+bilateral lateral intertransverse-process arthrodesis with bone graft; postoperative management was same for both groups; progressive walking (ten to twenty minutes, twice daily) during the first 4-6 weeks; exercises on a stationary bicycle or in water were begun at 6-8 weeks, and exercises for gentle flexion of the spine and strengthening of the abdominal muscles were added at eight to twelve weeks; no brace or corset was used iii) Back/leg pain measured separately with scale 0-5 (0=no pain; 5=severe pain); operative result measured with 4-grade scale (excellent = unrestricted activity and/or complete pain relief in back/legs; good=occasional discomfort (back/leg) necessitating non-narcotic medication, major improvement with preoperative condition, and resumption of unrestricted activity; fair=intermittent discomfort; improvement compared with preoperative condition; restrictions of activity, and occasional need for non-narcotic medication; poor=major discomfort, nonnarcotic or occasional narcotic medication; no improvement, major restrictions of activity Age NS Degenerative lumbar spondylolisthesis with To determine if concomitant intertransverse- Gender NS spinal stenosis - A prospective study comparing process arthrodesis provided better results Height of disc NS decompression with decompression and inter- than decompressive laminectomy alone transverse intertransverse process artrodesis N= 50 F= 3 years (range 2.4-4) Jönsson (1993b)31% i) Observational, consecutive study ii) Decompressive operation for central (N=80), lateral (n=80) LSS and HNP (n=120) iii) 4-grade scale (pain free, almost pain free, improved but significant residual pain, unchanged compared to preoperatively, and worse than preoperatively) Regular consumption of analgesics in Associated with unfavourable outcome (pain) central stenosis Patient related factors predicting the outcome of decompressive surgery Long preop. duration of sciatica in lat. stenosis Associated with poor outcome (pain) N=280 Long preop. duration of back pain NS F=2 years Age NS Gender NS See study title Jönsson (1993c)31% Time off work NS Work load NS Walking distance (reported) NS i) Observational consecutive study ii) Resection of processus spinosus, the laminae and maximally half of the facet joints using the undercutting technique (one-level 22%, two-level 55%, three-level 18%, four-level 5%) iii) Sagittal vertebral slipping (listhesis) in millimetres according to Wiltse and Winter, and slip exceeding >2mm was regarded as true Limitation: Preoperative predictor is operation-dependent No preoper. degenerative olisthesis (2mm), Postoperative vertebral slipping was avoidable and facet sparing technique utilized Jönsson (1994a)46% Vertebral slipping after decompression for Not defined. The increase spinal stenosis of postoperative vertebral Preoper. degenerative olisthesis 2mm 30% risk of progressive slip, but without associated N=60 slipping and its relation and facet sparing technique utilized clinical problems in the short term F= 1 year to outcome reported i) Observational, consecutive study ii) Decompression with facet-preserving technique in spinal stenosis (central LSS n=40; lateral LSS n=3) and conventional open disc excision for HNP (n=4) iii) Amount of complications; 4-grade subjective pain scale (excellent=almost/totally pain free; fair= improved but residual pain; unchanged; worse (compared to preoperative condition)) All patients were over 70 years, no control group Lumbar spine surgery in elderly- Diagnosis, postoperative compli- Age >70 years Results were on par with those of decompressive complications and surgical results cations, and surgical result in surgery in younger patients(compared to literature) N=50 patients over 70 years old who More favorable results concerning sciatica (results F=2 years underwent surgery for lumbar included all the patients) Limitation: study population had nerve root compression of a no control group (younger patients), degenerative origin were evaluated thus the conclusion concerning age in a prospective, consecutive study No back pain preoperatively age was not based on the actual population Jönsson (1995)38% i) Observational consecutive study ii) For LSS: decompression with facet-preserving technique; for HNP: open conventional or microscopic disc excision; no fusions were performed iii) Extensor hallucis longus power (3-grade scale): normal, reduced, severely reduced Katz (1995)38% Prognostic factors of the recovery of L5-root syndrome (extensor hallucis longus(EHL) -power severely reduced): Motor affliction of the L5 nerve root in The incidence, diagnosis Diagnosis (p=0.02, Kruskal-Wallis) lumbar nerve root compression syndromes and recovery after - central spinal stenosis The prognosis of EHL-power recovery was poor (0%) F= 4 month; 1- and 2 years surgery of patients with - lateral spinal stenosis 80% improved, no total recovery -5 spinal stenosis patients L5 root compression - disc herniation 56% total recovery, 28% improved -10 lateral stenosis patients syndromes and a severely reduced Age NS -20 disc herniation patients or absent power before surgery of Duration of preoperative symptoms NS the big toe extensor was evaluated i) Multicenter observational cohort study ii) Decompressive laminectomy for LSS (one-level 25%, two-level 36%, three-level 26%, four-level 13%; no fusion 70%; bony fusion 15%, bony fusion with instrumentation 15%) iii) Global 4-grade satisfaction score (1=very satisfied to 4=very dissatisfied) Multivariate analysis of patient satisfaction with the results of surgery Clinical correlates of patient To identify correlates of patient (Sat=satisfaction; B=beta coefficient; SIPS=sickness impact profile score) satisfaction after laminectomy satisfaction with the results of Back pain for degenerative lumbar spinal surgery Significant association for lesser Sat (B=0.17, p=0.005) Functional disability (SIPS) -"- (B=0.02, p=0.006) stenosis Greater medical comorbidity -"- (B=0.08, p=0.03) N=194 Age No association with satisfaction Gender -"- Depression score -"- F= 6 months Overall severity of pain in back, buttocks or legs Kleeman (2000)38% -"- i) Observational consecutive study ii) Decompression technique included complete excision of the ligamentum flavum through a modified laminotomy iii) 3-grade scale (good-excellent: absent or occasional mild back and leg pain; to be able to ambulate >1 mile or 20 minutes, no restriction of usual activities; fair= persistent mild back/leg pain, ambulation endurance < 1 mile or 20 minutes; some mild restrictions in their customary physical activity; poor= little to no pain relief from surgery, major activity limitations, or both. A repeat operation for any reason was considered a poor result, regardless of the ultimate level of the function Degenerative spondylolisthesis in NS; slight tendency to less favorable outcome Patient outcomes after minimally destabilizing To determine whether decompression lumbar spinal stenosis (p=0.11 at 2.5- and 0.08 at 4-year follow-up lumbar stenosis decompression - could be achieved without subsequent The "Port-Hole" -technique fusion for spinal stenosis with and N=54 ; F(mean)= 30 and 48 months McGregor (2002a)31% without degenerative spondylolisthesis i) Observational study ii) Posterior decompression for LSS (83% bi-,17% unilateral; fusion in 6%; 77% had ≥2 levels and 23% one level decompressed; 7 patients chose conservative treatment) iii) Visual analogue scale (worst and usual pain over the past week); Oswestry Disability Index, SF-36 General Health Questionnaire; psychological measures as mood, depression, anxiety and helplessness Subjective disability (Oswestry disability index) Outcome could not be reliably predicted The evaluation of the surgical management To investigate the Physical function (SF-36 general health questionnaire) from presurgical measures of function, of nerve root compression in patients with outcome of lumbar Pain (leg and back pain studied separately) disability, pain and psychological well- low back pain - Part 1:The assessment of outcome decompressive surgery Psychologic variables being N=84 patients undergoing LSS surgery in the initial post- Age No influence on outcome F = 6weeks, 6mo and one year operative year period Gender -"- in terms of function Preoperative duration of symptoms -"- disability, general Smoking -"- health and Earlier surgery McGregor (2002b)15% Was associated with many outcome measures, but psychological no consistent pattern was observed well-being i) Observational study (same population as in McGregor 2002a) ii) Posterior decompression for LSS (83% bi-,17% unilateral; fusion in 6%; 77% had ≥2 levels and 23% one level decompressed; 7 patients chose conservative treatment), iii) the patient were asked to rate the percentage of improvement they expected after surgery at 6 weeks, 6 months, and 1 year on a 5-point Likert scale (range 0=no improvement, 100%=full improvement) with respect to function, general health, pain and life satisfaction; in addition, they ranked how satisfied they expected to be, how confident they were in achieving a satisfactory outcome, and how important such an outcome was to them (5-point Likert scale based on percentage improvement); Oswestry Disability Index (function), SF-36 General Health Questionnaire (leg and back pain separately with visual analogue scale, general health) and Cantril Life Satisfaction scale were measured at every review stage and the actual and expected score was compared Preoperative expectations of outcome measured by Patients frequently had unrealistic expectations The evaluation of surgical management of nerve To investigate patient -General health (SF-36 General Health Quest.) and as a consequence tended to have lower root compression in patients with low back pain expectations of - Subjective function (Oswestry) levels of satisfaction N=84 surgery and short- and F=1 year long-term satisfaction - Life satisfaction (Cantril Life Sat. Scale) with the outcome of decompression in terms of pain, function, disability and general health Sato (1997)38% i) Observational consecutive study; 81 LSS patients with or without degenerative spondylolisthesis were divided into two groups; one level stenosis (n=53) and two-level stenosis (n=28); ii) In 2-level stenosis, the responsible level was determined with gait load test and selective nerve root block; all patients underwent selective decompression at the neurologically responsible level only iii) Assessment of Treatment for Low Back Pain made by the Japanese Orthopaedic Association Gait load test and selective nerve Used together, were helpful in determining responsible Clinical analysis of two-level compression To clarify the clinical features root block level in two-level stenosis (and improving results; no the cauda equina and the nerve roots in of two-level stenosis regarding the control group) lumbar spinal canal stenosis neurologic level responsible for the N=81 symptoms, neurogenic intermittent F=4.6 years (range 1-8) claudication and the outcome of selective decompression Spratt (2004)46% i) Consecutive cohort study - was designed to develop predictive models for surgical outcome based on information available prior to lumbar stenosis surgery ii) Partial laminectomy/arthrectomy iii) Functional status: Waddell Disability Index, (Low Back Outcome Score); VAS; reduction of pain during walking, reduction of leg pain. -Chi-squared automatic Predicted 90.1% of successful outcomes; A predictive model for outcome after interaction detection preliminary model conservative decompression surgery -More Waddell´s OR=0.648, 90% CI=0.362-0.991, p=0.08) for lumbar spinal stenosis non-organic signs NS trend toward inferior outcome Age NS Gender -"- Stenosis class -"- -acquired -mixed Minimal or mean canal diameter -"- at oper. site ( mm) Yukawa (2002)46% Flexion:extension velocity ratio -"- Continuous pain -"- Aorta calcification -"- Smoker -"- Comorbidities -"- Duration of symptoms -"- i) Observational study See above i) ii) Decompressive surgery for LSS; all patient had neurogenic claudication (74% underwent also posterolateral arthrodesis with instrumentation because of instability) iii) Visual analogue scale, Oswestry Disability Index, and neuroradiological imaging Cross-section of dural-tube <70mm2 Patients with dural tube <70mm2 had A comprehensive study of To evaluate patients undergoing vs. >70mm2 better postoperative reported functional ability (Oswestry) patients with surgically treated surgery for LSS and intermittent Multilevel central stenosis Shorter walking distance (with treadmill) pre- and lumbar spinal stenosis with neurogenic claudication with postoperatively (p<0.05) neurogenic claudication functional testing, quantitative No association with pain (VAS) N=62 imaging, and patient self- No association with functional ability (Oswestry) F= minimum 2 years assessment