Chan, Andrew - American Academy of Optometry
advertisement
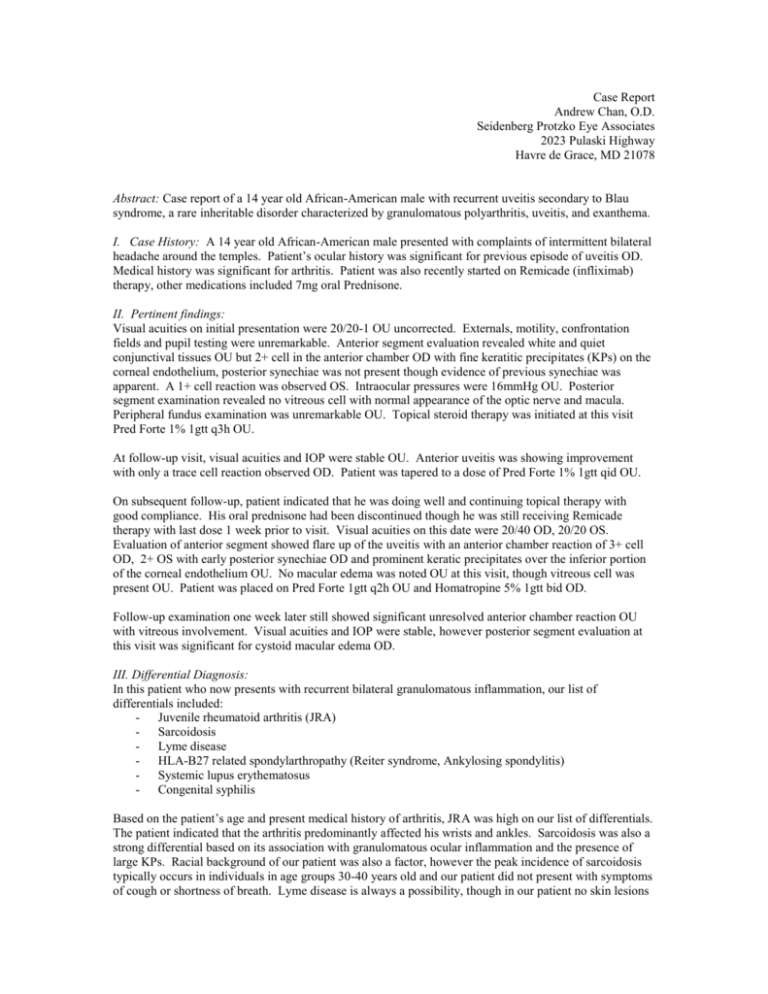
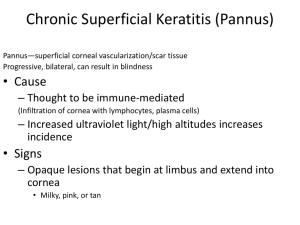
Case Report Andrew Chan, O.D. Seidenberg Protzko Eye Associates 2023 Pulaski Highway Havre de Grace, MD 21078 Abstract: Case report of a 14 year old African-American male with recurrent uveitis secondary to Blau syndrome, a rare inheritable disorder characterized by granulomatous polyarthritis, uveitis, and exanthema. I. Case History: A 14 year old African-American male presented with complaints of intermittent bilateral headache around the temples. Patient’s ocular history was significant for previous episode of uveitis OD. Medical history was significant for arthritis. Patient was also recently started on Remicade (infliximab) therapy, other medications included 7mg oral Prednisone. II. Pertinent findings: Visual acuities on initial presentation were 20/20-1 OU uncorrected. Externals, motility, confrontation fields and pupil testing were unremarkable. Anterior segment evaluation revealed white and quiet conjunctival tissues OU but 2+ cell in the anterior chamber OD with fine keratitic precipitates (KPs) on the corneal endothelium, posterior synechiae was not present though evidence of previous synechiae was apparent. A 1+ cell reaction was observed OS. Intraocular pressures were 16mmHg OU. Posterior segment examination revealed no vitreous cell with normal appearance of the optic nerve and macula. Peripheral fundus examination was unremarkable OU. Topical steroid therapy was initiated at this visit Pred Forte 1% 1gtt q3h OU. At follow-up visit, visual acuities and IOP were stable OU. Anterior uveitis was showing improvement with only a trace cell reaction observed OD. Patient was tapered to a dose of Pred Forte 1% 1gtt qid OU. On subsequent follow-up, patient indicated that he was doing well and continuing topical therapy with good compliance. His oral prednisone had been discontinued though he was still receiving Remicade therapy with last dose 1 week prior to visit. Visual acuities on this date were 20/40 OD, 20/20 OS. Evaluation of anterior segment showed flare up of the uveitis with an anterior chamber reaction of 3+ cell OD, 2+ OS with early posterior synechiae OD and prominent keratic precipitates over the inferior portion of the corneal endothelium OU. No macular edema was noted OU at this visit, though vitreous cell was present OU. Patient was placed on Pred Forte 1gtt q2h OU and Homatropine 5% 1gtt bid OD. Follow-up examination one week later still showed significant unresolved anterior chamber reaction OU with vitreous involvement. Visual acuities and IOP were stable, however posterior segment evaluation at this visit was significant for cystoid macular edema OD. III. Differential Diagnosis: In this patient who now presents with recurrent bilateral granulomatous inflammation, our list of differentials included: - Juvenile rheumatoid arthritis (JRA) - Sarcoidosis - Lyme disease - HLA-B27 related spondylarthropathy (Reiter syndrome, Ankylosing spondylitis) - Systemic lupus erythematosus - Congenital syphilis Based on the patient’s age and present medical history of arthritis, JRA was high on our list of differentials. The patient indicated that the arthritis predominantly affected his wrists and ankles. Sarcoidosis was also a strong differential based on its association with granulomatous ocular inflammation and the presence of large KPs. Racial background of our patient was also a factor, however the peak incidence of sarcoidosis typically occurs in individuals in age groups 30-40 years old and our patient did not present with symptoms of cough or shortness of breath. Lyme disease is always a possibility, though in our patient no skin lesions or symptoms consistent with Lyme disease were noted. Patient denied urethritis and lower back pain, he also did not exhibit any signs of malar rash which placed HLA-B27 related conditions and SLE lower on the differentials. Congenital syphilis was also a possibility but the absence of correlating peripheral retinal findings and negative history from mother made this diagnosis less likely. IV. Diagnosis and discussion Following correspondence with the patient’s primary care physician and obtainment of his previous hospital records, it was concluded that the patient had Blau syndrome (BS), a congenital form of early onset sarcoidosis (EOS), which was confirmed by skin tissue biopsy. Clinically both (BS and EOS) feature the same triad of symptoms of arthritis-uveitis-exanthema, with the one being inherited and the other acquired. In this particular patient, evaluation of his two brothers also showed that they shared similar characteristics, showing familial inheritance of the condition. Blau syndrome was first described by Edward Blau and also Douglas Jabs in 1985. Genetic analysis has shown that this condition has autosomal dominant inheritance and a number of specific mutations on chromosome 16q in codon 334. Both BS and EOS are now known to share a mutated form of caspase recruitment domain-15 (CARD 15), a protein involved in activation of nuclear factor kappa B which is in turn an up-regulator of pro-inflammatory cytokine transcription. Current prevalence of Blau syndrome among the US population is estimated at 2,000. EOS and JRA can be difficult to distinguish particularly in early stages, skin biopsy is typically most useful in differentiating the two. While EOS shares certain characteristics with the adult form of sarcoidosis, it rarely affects the lungs and other parenchymatous organs of the body. Chest imaging in our patient showed no pulmonary pathology. Ocular pathophysiogy of this condition is also unique to this subtype as patients with the adult-form of sarcoid who present with uveitis do not share the mutated form of the CARD15 gene. V. Treatment, management On the latest follow-up visit, our patient exhibited 3+ cell reaction OD, 2+ OS with keratitic precipitates and vitreous cell OU. Additionally, most concerning was the CME OD. As inflammation was responding poorly to topical steroid therapy, periocular repository was then necessary to control the ocular inflammation. 40mg/cc of Kenalog was then administered via posterior subtenon injection OD without complication. Topical therapy was maintained OU. Follow-up s/p subtenon Kenalog one week later showed visual acuities of 20/20 OU. Anterior chamber reaction was now only trace OD, 1+ OS. Vitreous cell was still present however was likely not from active inflammation. CME OD had subsided and patient was feeling well. Based on the timing of the patient’s latest Remicade infusion (patient is on a 7 week cycle) and the recent discontinuation of his Prednisone, the flare up of his uveitis may have resulted from a nadir of his immunosuppressive therapy. Future management of this patient will require consideration of his systemic treatment as well as managing the side effects of frequent long term steroid use (orally and topically) and changes to the anterior segment structures from the recurrent bouts of inflammation leading to a negative impact on vision. VI. Conclusion Blau syndrome and early onset sarcoidosis, although rare, can be a differential when evaluating young patients who exhibit recurrent or bilateral uveitis. A history of arthritis and external examination of patient for rash or dermatitis (exanthema) can be useful in determining the core triad of features which is characteristic of this condition. References: Alonso, D.; Elgart, G. W.; Schachner, L. A. Blau syndrome: a new kindred. J. Am. Acad. Derm. 49: 299302, 2003. Becker ML, Rose CD. Blau syndrome and related genetic disorders causing childhood arthritis. Curr Rheumatol Rep. 2005 Dec;7(6):427-33. Blau, EB. Familial granulomatous arthritis, iritis, and rash. J. Pediat. 107: 689-693, 1985 Jabs, DA.; Houk, JL; Bias, WB; Arnett, FC. Familial granulomatous synovitis, uveitis, and cranial neuropathies. Am. J. Med. 78: 801-804, 1985. Kanazawa, N.; Okafuji, I.; Kambe, N.; Nishikomori, R.; Nakata-Hizume, M.; Nagai, S.; Fuji, A.; Yuasa, T.; Manki, A.; Sakurai, Y.; Nakajima, M.; Kobayashi, H.; Fujiwara, I.; Tsutsumi, H.; Utani, A.; Nishigori, C.; Heike, T.; Nakahata, T.; Miyachi, Y. :Early-onset sarcoidosis and CARD15 mutations with constitutive nuclear factor-kappa-B activation: common genetic etiology with Blau syndrome. Blood 105: 1195-1197, 2005. Martin TM, Doyle TM, Smith JR, Dinulescu D, Rust K, Rosenbaum JT. Uveitis in patients with sarcoidosis is not associated with mutations in NOD2 (CARD15). Am J Ophthalmol. 2003 Nov;136(5):933-5 Milman N, Byg KE. Blau syndrome--a chronic granulomatous, genetic disease. Ugeskr Laeger. 2006 Oct 16;168(42):3612-4 Simon JW, Buckley EG, Drack AV, Hutchinson AK, Plager DA. BCBS Section 6: Pediatric Ophthalmology and Strabimus. American Academy of Ophthalmology 2004-2005, p 292-297.