SSU Standards (Revised)
advertisement

Standard Clinical Procedures
Guidelines
ORAL DIAGNOSIS
I. Coronal Caries.
Historical perspective. Caries diagnosis by clinical means has traditionally used a combination of visual,
tactile, and radiographic means. The use of a dental explorer for tactile examination has been a
controversial issue over the past few years, because of the possibility of Mutans Streptococcus crosscontamination caused by inoculating a healthy pit and fissure system (Loesche, 1998) and because “routine
use of the explorer…is likely to damage the enamel matrix of noncavitated lesions where remineralization
is taking place (Burt and Eklund, 1999).” In addition, newer diagnostic tools such as the DiagnoDENT
have conflicting results that make their use as a diagnostic tool secondary at best (Kidd, Ricketts, Pitts,
1993). Caries is found to be more prevalent in different teeth, and there are definite demographic and
behavioral risk factors. Teeth most susceptible to dental caries in the general population are (in order):
mandibular first and second molars, maxillary first and second molars, mandibular second biscuspids,
maxillary first and second bicuspids, maxillary central and lateral incisors, maxillary canines and
mandibular first bicuspids, mandibular central and lateral incisors, and mandibular canines (Klein and
Palmer 1941). Demographic risk factors include age (caries risk experience is directly linked to the
presence of early childhood caries [Kaste, Marianos, Change, Phipps, 1992]), gender (females tend to have
higher DMF scores than males of the same age [U.S. Public Health Service, 1971]), socioeconomic status,
familial and genetic patterns, and race and ethnicity. Behavioral variables are well understood by dentists,
and include diet, consumption of fluoridated water or lack thereof, oral hygiene, and, especially in early
childhood caries development, the age of inoculation of M. Streptococcus. In light of all of these factors,
the clinician must use a visual and radiographic examination in combination with an adequate history to
make a diagnosis of coronal caries and, more importantly, the treatment needs of the patient.
Standardization. The Schurz Service Unit Dental Program will employ a comprehensive dental
examination, to include a visual examination, limited tactile examination by dental explorer, radiographic
examination, and dental history and prevention assessment. See A1 – Dental Examination Record – for
correct documentation. The use of the D1-D3 scale (WHO) will be utilized to define treatment needs for
service unit dental patients:
Criteria for Diagnosing Coronal Caries (D1-D3 Scale)
0. Surface sound. No evidence of treated or untreated clinical caries (slight staining
allowed in an otherwise sound fissue).
Treatment modalities. Place a pit and fissure sealant containing fluoride in all
primary and permanent posterior teeth, and, if necessary, the palatal pits of
maxillary lateral incisors. In the Schurz Service Unit, this is to be done
regardless of caries risk classification.
D1. Initial caries. No clinically detectable loss of substance. For pits and fissures, there
may be significant staining, discoloration, or rough spots in the enamel that do not catch
the explorer (if the explorer is used), but loss of substance cannot be positively
diagnosed. For smooth surfaces, these may be white, opaque areas with loss of luster.
This diagnosis includes interproximal caries radiographically confined to the enamel.
Treatment modalities. In our population, this presents the greatest challenge to
us, since we often tend to err on the side of caution and treatment plan operative
dentistry for the incipient lesion. However, the Schurz Service Unit will treat
initial caries, as defined above, by use of both fluoride application (varnish or
rinse) and pit and fissure sealant application. The patient will be recalled at least
every six months for re-evaluation.
1
Note about DiagnoDENT. If the clinic utilizes the DiagnoDENT to aid in
caries diagnosis, it is important to realize that this transillumination tool is most
effective over several readings; in other words, a diagnosis should not be made
on the basis of a single DiagnoDENT score. However, if the DiagnoDENT
score progressively increases at each recall (and is recorded in the Dental
Progress Notes), the DiagnoDENT can be an effective tool in caries diagnosis.
D2. Enamel caries. Demonstrable loss of tooth substance in pits, fissures, or on smooth
surfaces, but no softened floor or wall or undermined enamel. The texture of the material
within the cavity may be chalky or crumbly, but there is no evidence that cavitation has
penetrated the dentin.
Treatment modalities. This diagnosis requires the use of a dental explorer, and,
as previously stated, the explorer should be used less frequently than in the past.
Therefore, if there is visual evidence of loss of tooth substance but the caries
does not extend past the dentin-enamel junction, the treatment of choice is a
preventive resin restoration (unfilled resin) and fluoride application.
D3. Caries of dentin. Detectably softened floor, undermined enamel, or a softened
wall, or the tooth has a temporary filling. On approximal surfaces, the explorer point
must enter a lesion with certainty.
Treatment modalities. Prior to the use of the explorer, there should be clear
visual and/or radiographic evidence of dentinal caries. Treatment of D3 caries is
amalgam or composite restorations.
D4. Pulpal involvement. Deep cavity with probable pulpal involvement. Pulp should
not be probed.
Treatment modalities. See endodontic diagnosis and treatments.
It is important to make a distinction between a dental caries diagnosis and the proposed treatment on the
Dental Examination Record. For example, if only the mesial surface of tooth #8 is caries, the dentist
should not record MFL caries, but only mesial caries, but should clearly mark the treatment plan as an MFL
(or ML or MF) composite, should that be the proposed treatment.
If a dentist uses ADA Code 0150, he/she must fulfill all of the requirements of a comprehensive dental
examination, which include (and should be documented on the Dental Examination Record):
(1) Coronal caries examination
(2) Root caries examination (adults)
(3) Periodontal Screening and Recording (PSR, or CPITN), ages 15 and higher
(4) Soft tissue examination
(5) TMJ evaluation
(6) Fluorosis examination, to include documentation of any enamel defects
(7) Prevention Assessment
(8) A written, signed proposed treatment plan (signed by the patient and dentist)
(9) Radiographs, as appropriate
(10) Review of the patient’s medical history
If all of the above procedures are not performed during the examination appointment, the dentist did not
perform a comprehensive dental examination and must enter an ADA Code of 0140 or 0120.
The Dental Examination Record is an extremely important medico-legal document, and should be
completed fully by all service unit dentists. The Prevention Assessment in the right column must be
completed on each patient at the initial examination and annual recall (see example), and a Periodontal
Screening and Recording (PSR, or, alternatively, the CPITN) should be recorded at each initial and recall
examination. The proposed treatment plan must be completed by the treating dentist, not the dental
assistant, and should list proposed treatment by appointment (i.e., “Appointment 1 – Seal #19, Amalgam
#20, Appointment #2 – Composite #24, 25”). Alternative treatments should be both verbally discussed
with the patient and documented on the Dental Examination Record as well. Most importantly, the patient
and dentist must sign the Dental Examination Record for it to be a valid medico-legal document.
2
II. Periodontal Diseases.
Historical perspective. “Plaque-induced periodontal diseases are mixed infections associated with
relatively specific groups of indigenous oral bacteria (American Academy of Periodontology, 2003).” The
clinical dentist utilizes several objective assessments in making a periodontal diagnosis, including the
presence or absence of clinical signs of inflammation – bleeding upon probing, cyanotic gingival color, a
purulent gingival sulcus, and loss of interdental papilla – a radiographic examination to determine the
percent loss of horizontal bone and possible vertical defects, and assessment of probing depths and
attachment loss (and a PSR). In addition, subjective criteria that aid in the diagnosis of periodontal diseases
arise from the dentist taking a medical history, dental history (to include reasons for previous tooth loss,
current oral hygiene, and tobacco use), and the presence of other signs and symptoms of periodontal
disease, such as pain, observable plaque and calculus, etc. A diagnosis of periodontitis based solely on
periodontal pocket depth, solely on gingival inflammation, or, in some cases even when both are present, is
not always entirely accurate. For example, deeper periodontal pockets without the presence of
inflammation may the result of certain systemic diseases, occlusal trauma, or even previous periodontitis
but now a stable periodontium, or even pseudopockets resulting from hyperplastic gingival or partially
erupted teeth. Gingival inflammation without corresponding pocket depths only indicates gingivitis, when
there is no loss of connective tissue attachment. Finally, in some cases where a patient had a history of
periodontitis and now exhibits gingival inflammation, the clinical dentist must ascertain whether it is
recurrent periodontitis or simply gingivitis superimposed on a stable periodontium.
Standardization. The Schurz Service Unit Dental Program will provide a periodontal assessment on all
patients seeking comprehensive oral health care, through conducting a Periodontal Screening and
Recording (PSR, or alternatively, a CPITN) for patients over 12 years of age, for permanent teeth excluding
third molars, and will schedule and perform a full-mouth periodontal probing for all patients with at least
two sextants of a “3” score or a single sextant with a “4” score, using the guidelines set forth below. In
addition, the service unit dental program will employ the most recent Classification of Periodontal Diseases
and Conditions by the American Academy of Periodontology (1999), which are listed below.
Periodontal Screening and Recording (PSR, using a WHO probe)
Code 0. Health. No clinical evidence of clinical signs and symptoms of gingival
inflammation, and no periodontal pockets greater than 3.5 millimeters (the beginning of
the black band on the WHO probe). This code is not affected by the amount of plaque
evident on the tooth surfaces.
Treatment modalities. Adult prophylaxis (by dentist, dental assistant, or dental
hygienist), customized oral hygiene instructions to include demonstration
models, and 6 month to one year recalls, depending also on caries risk
assessment.
Code 1. Gingivitis. Clinical evidence of inflammation, as evidenced by bleeding upon
skimming or bleeding upon probing, with no pocket measurements greater than 3.5
millimeters (the beginning of the black band on the WHO probe).
Treatment modalities. Customized oral hygiene instructions to include
demonstration models, rubber-cup prophylaxis if desired by dentist or patient
(performed by dentist, dental assistant, or dental hygienist), and 6 month to one
year recalls, depending also on caries risk assessment.
Code 2. Gingivitis, calculus present. Clinical evidence of inflammation, as evidenced
by bleeding upon skimming or bleeding upon probing, with calculus either visually
observed by the dentist or felt by the periodontal probe, with no pocket measurements
greater than 3.5 millimeters (the beginning of the black band on the WHO probe).
Treatment modalities. Adult prophylaxis (by dentist, dental hygienist, or dental
assistant), to include isolated subgingival or supragingival scaling, customized
oral hygiene instructions to include demonstration models, and six-month
hygiene recalls.
3
Code 3. Mild to Moderate Periodontitis. Periodontal pocket depth measurement
greater than 3.5 millimeters but less than 5.5 millimeters on at least one tooth in the
sextant. It is important to note that clinical signs of inflammation nor subgingival
calculus need to be observed in order to assign this code; it is reflective only of the
periodontal probing measurement.
Treatment modalities. The dentist must ascertain whether the patient has
periodontitis (pocket depths greater than 3.5 mm and less than 5.5 mm, with
concurrent signs and symptoms of inflammation and possible calculus) or
whether the probing depth is a result of a pseudopocket, hyperplastic tissue,
occlusal trauma, or partially erupted tooth. If the dentist makes a diagnosis of
periodontitis (see disease classifications), treatment may involve scaling and
root planing by quadrant or half mouth – if scaling and root planning is
indicated, then it should be done with local anesthesia. The treatment plan must
be detailed in the Dental Examination Record by the treating dentist. Scaling
and root planing may be performed by the dentist or dental hygienist, while
other procedures not requiring anesthesia (prophylaxis with isolated supra- and
sub-gingival scaling) may be performed by the dentist, dental hygienist, or
dental assistant. Following periodontal therapy, the patient should be recalled at
3-6 month intervals as determined by the dentist or dental hygienist.
Code 4. Moderate to Advanced Periodontitis. Periodontal pocket depth measurement
greater than 5.5 millimeters (past the first black band on the WHO probe)on at least one
tooth in the sextant. Once a Code 4 is called on a sextant, the dentist need not bother
probing the rest of the sextant. It is important to note that clinical signs of inflammation
nor subgingival calculus need to be observed in order to assign this code; it is reflective
only of the periodontal probing measurement.
Treatment modalities. The dentist must ascertain whether the patient has
periodontitis (pocket depths greater than 5.5 mm, with concurrent signs and
symptoms of inflammation and possible calculus) or whether the probing depth
is a result of a pseudopocket, hyperplastic tissue, occlusal trauma, or partially
erupted tooth. If the dentist makes a diagnosis of periodontitis (see disease
classifications), treatment may involve a gross debridement (with or without
local anesthesia) prior to scaling and root planning, full-mouth periodontal
probing before or after the debridement, and scaling and root planing by
quadrant or half mouth – with local anesthesia. This treatment plan must be
detailed in the Dental Examination Record by the treating dentist. Scaling and
root planing may be performed by the dentist or dental hygienist. Following
periodontal therapy, the patient should be recalled at an individualized recall
based on response to care, no more than 6-month interval (and it can be shorter)
as determined by the dentist or dental hygienist.
Treatment for the diabetic patient. Pursuant to the service unit (and IHS)
protocol for treating the diabetic dental patient, if a diabetic patient has two
sextants of a Code 3 or a single sextant of a Code 4, the patient qualifies as a
“protocol” patient. For those patients that do not qualify as a protocol patient,
treatment modalities are identical to those of the non-diabetic patient as
described above. For the diabetic protocol patient, treatment consists of:
i. Appointment #1 – Comprehensive dental examination, full-mouth
radiographic series, panoramic radiograph if available, preliminary oral
hygiene instructions (brushing, flossing). Prescribe Doxycycline, 100
mg tablets, with instructions to take 1 tablet twice daily beginning on
the day of the second appointment, for 14 days (28 tablets total).
ii. Appointment #2 – Scaling and root planing, utilizing only the Piezon
Master 400 (in other words, very little hand scaling and root planing),
under local anesthesia. This procedure should last no more than one
hour in length, and should consist of two quadrants. At the
4
appointment, a glycated hemoglobin level (HbA1C) should be
ascertained either by referring the patient to the medical department or
reviewing the patient’s medical record (the HbA1C must be no more
than 30 days old). At this appointment, periodontal probing should be
performed and charted on the anesthetized two quadrants, oral hygiene
instructions should be customized to the patient (to include an
interproximal brush, chlorhexidine rinse, and other hygiene aids),
hopeless teeth in the two quadrants should be extracted, and the visit
should be recorded on the Diabetic Data Form. At the conclusion of
this visit, the patient should be scheduled to return to the dental clinic
in two weeks or less (while still under antibiotic coverage).
iii. Appointment #3 -- Scaling and root planing, utilizing only the Piezon
Master 400 (in other words, very little hand scaling and root planing),
under local anesthesia. This procedure should last no more than one
hour in length, and should consist of the remaining quadrants. At this
appointment, periodontal probing should be performed and charted on
the anesthetized quadrants, oral hygiene instructions should be
customized to the patient (to include an interproximal brush,
chlorhexidine rinse, and other hygiene aids), hopeless teeth in the
remaining anesthetized quadrants should be extracted, and the visit
should be recorded on the Diabetic Data Form. At the conclusion of
this visit, the patient should be scheduled to return to the dental clinic
in 6-8 weeks for re-evaluation.
iv. Appointment #4 – Re-evaluation of the patient, to include isolated spot
probing, periodontal maintenance cleaning with the Piezon Master 400,
reinforcement of oral hygiene, and the dentist’s determination as to
whether the patient’s periodontal status has improved or not (and
documented on the Diabetic Data Form). Following this appointment,
the patient should be recalled every 3-6 months, depending on the
stability of the periodontium, patient compliance, etc. If the
periodontal status has improved, the patient can be scheduled for
routine restorative procedures.
v. Appointment #5 – Annual recall of the patient, to include full-mouth
periodontal probing, obtaining a HbA1C measurement (by chart review
or ordering the test), periodontal maintenance visit, and completing the
Diabetic Data Form. If clinically stable with no signs and symptoms of
inflammation, the patient can be placed on a 6-month recall program; if
not clinically stable, the patient should continue to be recalled every 13-6 months until clinically stable. If not clinical stable, the patient
should continue to be recalled every 3-6 months and Periostat or local
antibiotics should be considered, as well as the patient should be
recommended for referral to a periodontist for further treatment.
The Classification of Periodontal Diseases by the American Academy of Periodontology is below. This is
the diagnosis that should be entered into diagnosis space on the Dental Examination Record, and should not
be confused with Case Types (Case Type I – gingivitis, Case Type II – mild periodontitis, Case Type III –
moderate periodontitis, Case Type IV – advanced periodontitis, and Case Type V – refractory
periodontitis).
CLASSIFICATION OF PERIODONTAL DISEASES
Gingivitis (corresponds to PSR/CPITN codes of 1 and 2)
Chronic Periodontitis (corresponds to PSR/CPITN codes of 3 and 4, without other
contributing factors – in other words, rule out other diagnoses first before using this one).
5
Aggressive Periodontitis (corresponds to PSR/CPITN codes of 3 and 4; localized
juvenile periodontitis, generalized juvenile periodontitis, prepubertal periodontitis, etc.)
Periodontitis as a manifestation of systemic diseases (such as leukemia)
Necrotizing Periodontal Diseases (such as acute necrotizing ulcerative gingivitis)
Abscesses of the Periodontium (such as the lateral periodontal abscess)
Periodontitis associated with endodontic lesions (the combined endo-perio abscess)
History of periodontal disease (to complete dental examination record only)
III. Endodontic Diagnosis (from the IHS Clinical Specialties Guide)
Historical perspective. Incomplete diagnosis results in additional clinical visits, continued pain and
suffering, loss of patient confidence, and possible inappropriate treatment. It is imperative that a thorough
diagnosis be performed on each case. Careful attention to the patient's symptoms is required. Once the
tooth is identified, the pulpal, periradicular, periodontal, and restorative status all must be evaluated and
documented. To perform a thorough endodontic diagnosis of a patient, you should perform: (1) a complete
medical and dental history of the patient; (2) a physical examination (to include periapical tests, pulpal
tests, periodontal tests, and a search for cracked and fractured teeth); (3) a radiographic examination; and
(4) special tests as necessary.
Standardization. The Schurz Service Unit Dental Program will adhere to the Indian Health Service Dental
Specialties Guide regarding endodontic diagnosis. All service unit facilities will record an endodontic
diagnosis and treatment plan (with alternatives) in the Dental Examination Record and/or the Dental
Progress Notes, using the terminology described below. In addition, all tests used in determining the
diagnosis – history, examination, radiographic, and special tests – must be entered in the Dental Progress
Notes.
Health History
Medical History. A succinct yet thorough review of the medical history should take place at the beginning
of each visit. If there are any questions about systemic or mental ailments that might affect the treatment
you plan for your patient, you should consult with your patient's physician.
Dental History. To perform a thorough dental history of the patient, you should: (1) review the past dental
history; (2) review the patient's chief complaint; and (3) review aspects of pain
Nature of pain. Identifying the nature of the pain can help to differentiate pain of dental origin
from pain stemming from other tissues. Pain which is very indicative of endodontic pathosis is
irreversible in nature, intense, spontaneous, and continuous.
Referred pain. Referred pain is most commonly manifested in other teeth in the same or opposing
quadrant. It almost never crosses the midline of the head. However, referred pain is not
necessarily limited to other teeth. It may be unilaterally referred to the preauricular area, down the
neck, or up to the temporal region. In these cases the source of the referred pain is almost always
a posterior tooth.
Pain of nonodontogenic origin. Pain of nonodontogenic origin includes pain from a broad range
of sources: organic (e.g., sinus disease and tumor); functional (e.g., myofacial pain dysfunction
and TMJ dysfunction); vascular (e.g., migraine headache); neurological (e.g., trigeminal
neuralgia); psychological
6
Extraoral
Step
1
2
Examination Procedures. Follow these steps to perform a thorough extraoral examination.
Action
Observe the patient's coloring.
Observe for facial asymmetry or distention.
3
Note: These are indicative of swelling of odontogenic origin or systemic disease.
Observe the patient's eyes for dilation or constriction.
Note: These are indicative of systemic disease, premedication, or fear.
Intraoral Examination. Follow these steps to perform a thorough intraoral examination.
Step
Action
1
Perform a soft tissue examination as follows:
Substep
Action
a
Dry each area to be examined.
b
Look for changes in the following:
•
•
•
2
color
contour
consistency
Note: The presence of a sinus tract may indicate that a periapical suppuration
has resulted from pulp that has undergone necrosis in at least one root. All sinus
tracts should be traced with a gutta percha point to locate their source since
occasionally the source can be remote.
Examine the dentition for the following:
•
•
•
•
•
•
discoloration
fractures
abrasions
erosion
caries
large restorations
Note: All of these can be clues to the offending tooth. (For example, a discolored anterior crown
is often pathognomonic of pulpal disease or may be the sequela of earlier root canal therapy.)
Periradicular Tests
Percussion Test. A percussion test does not give an indication of the health or integrity of the
pulp tissue; it only indicates whether there is inflammation around the periodontal ligament.
A positive response to percussion can be caused by a variety of factors:
teeth undergoing rapid orthodontic movement
high restoration
periodontal disease
partial or total necrosis of the pulp (that has inflamed the PDL)
Palpation Test. The index finger is rolled while pressing the mucosa against the underlying bone.
If the mucoperiosteum is inflamed, this motion will reveal the existence and the degree of
sensitivity caused by the periapical inflammation. If a site that feels tender to palpation is found,
its location and extent should be recorded as well as whether or not the area is soft or firm. This
provides important information on the possible need for incision and drainage. A positive
palpation test indicates inflammation in periapical tissues into the bone and mucosa in the apical
region.
7
Pulpal Tests
Thermal Tests. The response to thermal tests often provides information about whether the pulp
is healthy or inflamed. Caution: Response to a stimulus does not guarantee a pulp's vitality or its
health, but only indicates the presence of some nerve fibers capable of carrying sensory impulses.
To obtain reliable information, similar tooth types should be tested and compared.
Additional meaningful information can be obtained when stimuli similar to those that provoke
pain in the teeth are used during the clinical tests. You must carefully explain the procedures
involved and sensations expected during each test to the patient. Teeth to be tested should be
isolated and dried with 2 by 2-inch gauze.
The following responses typically occur:
Thermal testing on a vital tooth usually results in a sharp sensation of pain. This response
may occur regardless of pulp status (normal, reversible, or irreversible pulpitis).
When the response becomes more intense and prolonged, this is indicative of irreversible
pulpitis.
Teeth with necrotic pulps for the most part will not respond to thermal stimulation.
Electric Pulp Test. If the patient's medical history indicates that a cardiac pacemaker has been
implanted, the use of an electric pulp tester is contraindicated. The electric pulp tester is designed
to stimulate a response by exciting the neural elements within the pulp. It does not provide
information about the tooth's vascular supply which is the real determinant of vitality.
Electric Pulp Test responses False positive and negative results often occur.
The main reasons for false positive responses are as follows:
-conductor/electrode contact with large metal restoration or gingiva allows current to
reach the attachment apparatus
-patient anxiety
-liquefaction necrosis (may conduct current to the attachment apparatus)
-failure to isolate and dry the teeth
The main reasons for false negative responses are as follows:
-patient heavily premedicated with analgesics, narcotics, alcohol, or tranquilizers
-inadequate contact with enamel (i.e., insufficient conductor or contact with composite
restoration)
-recently traumatized tooth
-excessive calcification of pulp chamber
-recently erupted tooth with immature apex
-partial necrosis
Periodontal Evaluation,. When the periodontium is involved it must be determined whether the condition
is of endodontic origin, periodontal origin, or a combination of both. In endodontic diagnosis the vitality of
the tooth in question should be determined first. If:
the pulp is vital, then it may be ruled out as the source of the problem
the pulp is necrotic or partially vital, then it is either the cause of the problem or a contributing
source
radiographically, when only a portion of the root is involved or if the furcation is involved
when the mesial and distal crestal bone is intact, an endodontic lesion is suspected
the defect can be probed, it is usually a narrow tubular defect as compared to a wider
periodontal defect, an endodontic origin is suspected
the gingiva is inflamed and bone loss is widespread and present on adjacent teeth, periodontal
disease is suspected
upon probing, plaque or calculus is encountered and the defect is diffuse and crater-like,
periodontal treatment may be indicated. If the defect is of periodontal origin, the tooth will
probably test within normal limits.
Treatment Planning. If both periodontal disease and endodontic disease are present, endodontic
therapy should be completed first followed by periodontal therapy as soon as possible. If
8
periodontal therapy is completed first and the endodontic lesion is not treated, the defect may not
heal. If the endodontic therapy is adequate, the prognosis rests with the periodontal therapy.
Radiographic Evaluation. Multiple diagnostic radiographs, taken from various angles, should be
interpreted carefully. You should not automatically anticipate radiographic change in a tooth when
examining a patient in pain.
Soft tissue changes in the pulp will not appear on a radiograph.
Not all periapical lesions will appear on a radiograph. A lesion must involve the cortical plate
to be detected on a radiograph.
Once a lesion does appear on a radiograph, the actual area involved and the amount of bony
destruction are greater than the extent shown on the film.
Evaluating the Radiograph. For purposes of discussion, consider dividing the radiograph into a
coronal and a radicular segment. Then evaluate their contributions to endodontic diagnosis.
Coronal Aspect Features. Consider the following features when examining the coronal
aspect of the radiograph:
the relationship of the pulp horns to the existing restoration or caries
the presence of prior pulp cap or pulpotomy
the presence of retrogressive changes of the pulp chamber (e.g., recession,
resorption, or pulp stones)
Note: Pulp stones are not always pathologic.
crestal bone levels and the presence of calculus
often canals separate at the coronal root level, so additional canals can be detected
here
Radicular Aspect Features. Consider the following features when examining the
radicular aspect of the radiograph:
separated roots
position of the canal within the root
root pathology (e.g., calcification, resorption, and fracture)
periapical pathology including osteosclerosis and condensing osteitis
intracanal aberrations resulting from previous treatment (e.g., ledging, perforations,
and instrument fragments)
location and type of radiolucency (A lateral radiolucency may indicate a large lateral
canal. A teardrop or "J" shaped radiolucency may indicate a linear fracture.)
Angulated Radiographs. Additional angulated radiographs can be indispensable in
locating additional roots and canals. The following are some examples of their usage:
When a canal disappears abruptly near the apex on a straight-line radiograph, it
should be presumed that the canal is branching into extra canals. This can often be
verified by an additional angulated film.
Normal anatomical landmarks may appear as pathosis when their image is
superimposed on an apex. Additional radiographs at different angles will show that
these landmarks change position. If in fact periapical pathosis does exist, its
radiographic image will not change from its apical position in the various
radiographs.
Special Tests. Occasionally the following tests are indicated to provide additional diagnostic information:
(1) test cavity; (2) caries removal; (3) selective anesthesia; (4) transillumination.
Test Cavity. When other tests are inconclusive (especially on fully crowned or splinted teeth) a
test cavity can be performed without the use of local anesthesia. A small preparation is made into
the lingual surface of an anterior tooth or the occlusal surface of a posterior tooth. If the tooth is
vital, the patient will experience pain as the bur nears the dentino-enamel junction. A necrotic or
inflamed pulp will not yield a comparable response.
Caries Removal. Determining if a tooth is reversibly or irreversibly inflamed may be difficult.
Caries removal should be performed to determine the extent of the disease process (i.e., clinical
9
exposure requiring root canal therapy or extraction or no exposure with placement of a sedative
restoration).
Selective Anesthesia. Selective anesthesia is useful in diagnosing painful teeth particularly when
the patient cannot isolate the offender to a specific arch. To test within the maxillary arch,
anesthesia should be from anterior to posterior because of anatomic distribution of the nerve
fibers. Studies have shown that the PDL injection does not predictably anesthetize a single tooth.
This method should not be used to identify a suspected tooth.
Transillumination. Transillumination with fiber optics is useful in diagnosing cracked or
fractured teeth. Do not use the operatory light during transillumination to increase the contrast and
efficiency of the fiber optic light. Remove the restoration, dry the prep, place the light source on
the buccal and lingual cervical areas, and examine closely for crack lines in the dentin.
Cracked and Fractured Teeth. Searching for cracked and fractured teeth is an important but difficult part
of the patient's physical examination. Structural cracks may result from occlusal or accidental trauma and
restorative procedures. A vertical fracture may result in a periapical lesion that fails to resolve after a root
canal filling and apical surgery.
A structural crack is a break or split in the continuity of the tooth surface without a perceptible
separation. Structural cracks deep in the dentin and close to or involving the pulp are a perplexing
cause of dental pain. The crack cannot be wedged, separated, or seen on a radiograph, although it
may be a precursor to a fracture. Structural cracks by definition involve the dentin approaching
the pulp.
Structural cracks may be symptomatic or asymptomatic with the exact etiology difficult
to establish. Symptoms may include the following:
The pain is erratic, occurring inconsistently on mastication.
The patient is unable to describe the complaint clearly or precisely.
Confirming a Structural Crack. Confirmation tests may include- a bite test
removal of restoration and use of disclosing dye
transillumination
responsive testing (including the use of thermal or electric stimuli and percussion to determine
the need for root canal therapy)
Structural cracks in denting must be removed. If the crack extends into the pulp, endodontic
therapy is indicated. If the crack is noted on the floor of the pulp chamber, the case is usually
hopeless. If you are not sure about the prognosis, perform a complete pulpectomy, reduce the
tooth from occlusion, cement an orthodontic band and observe to determine whether the pain to
mastication resolves. If so, complete the endodontic therapy and restore the tooth with a full
cuspal-coverage restoration (but not a crown). If the tooth remains asymptomatic for several
months, then a crown can be placed, but the patient must understand that the long-term prognosis
is questionable.
Bite Test. Teeth with structural cracks often are not percussion sensitive, but do exhibit pain to
chewing. A bite test with either a cotton-tipped applicator, or a device like the Tooth Slooth, will
produce a positive response. The device should be placed in the central groove area, plus on
individual cusps, and tested for pain during or after biting.
Treatment Planning for a Structural Crack. Emergency treatment: Place a full cuspalcoverage restoration which reduces the occlusal stress in centric and lateral movements. This will
reduce the pain and prevent progression of the crack. Note: Special consideration should be
given during root canal therapy. Excessive condensation forces should be avoided, and the use of
posts is not advised.
Diagnosing Vertical Fractures. If a patient continually complains of pain when chewing or pain
with horizontal tapping of the crown, a vertical fracture should be suspected. These symptoms can
develop at anytime before, during, or after endodontic therapy. A tooth with a periapical lesion
that fails to resolve after proper root canal therapy and apical surgery should be suspected of
having a vertical root fracture.
10
Vertical crown/root fracture should be part of the differential diagnosis when
conventional periodontal therapy does not resolve a sulcular defect. When an isolated sulcular
defect persists in spite of repeated attempts to correct it and while surrounding teeth remain
periodontally sound, a vertical fracture could be implicated.
Reflecting full thickness mucoperiosteal flap with the aid of a strong fiber optic light may
reveal a fracture line. This procedure is especially helpful when the tooth in question has been
covered with a full crown.
Treatment Planning for a Vertical Fracture. Extraction is required if the etiology is a vertical
fracture of a single-rooted tooth or a mesial-distal fracture of a multi-rooted mandibular tooth.
Pulpal Diagnosis. The following terminology is used when discussing pulpal conditions:
(1) normal pulp; (2) reversible pulpitis; (3) irreversible pulpitis; and (4) necrotic pulp. The pulpal diagnosis
must be entered under the “A” (assessment) in the SOAP format of the Dental Progress Notes.
Normal Pulp. The conditions associated with normal pulp are- moderate response to pulp stimuli
response subsides when stimulus is removed
tooth is free of spontaneous symptoms
radiograph shows an intact lamina dura
Reversible Pulpitis. The conditions associated with reversible pulpitis are- sharp thermal response (especially to cold)
asymptomatic unless provoked by external stimulus
most commonly caused by defective restoration, restorative procedures, or by dental caries
Irreversible Pulpitis. The conditions associated with irreversible pulpitis are- prolonged response to temperature change
spontaneous episodes of pain
pain from change in posture
intense throbbing pain
Necrotic Pulp. The conditions associated with necrotic pulp are- the possible result of an untreated pulpitis or trauma
total necrosis usually asymptomatic until the periodontal ligament (PDL) is affected
no response to pulp vitality tests
the crown will darken occasionally with anterior teeth
possible combination of responses from multirooted teeth
Periradicular Diagnosis. The following periradicular conditions can be detected using the periradicular
tests: (1) acute apical periodontitis; (2) acute apical abscess; (3) chronic apical periodontitis; (4) Phoenix
Abscess; and (5) periapical osteosclerosis
Acute Apical Periodontitis. The conditions associated with acute apical periodontitis are- local inflammation of the periapical tissues
tenderness with percussion
disease which may occur with vital and nonvital teeth (pulp tests must be performed.)
periodontal ligament which may appear normal or slightly widened
Acute Apical Abscess. The conditions associated with acute apical abscess are- an advanced form of apical periodontitis from a necrotic tooth
it may appear normal or with a widened PDL radiographically
moderate to severe pain
rapid onset of swelling
some degree of swelling with extreme tenderness to percussion and palpation
patient may be febrile
differential diagnosis--lateral periodontal abscess (vital pulp)
Chronic Apical Periodontitis. The conditions associated with chronic apical periodontitis are--
11
usually asymptomatic but sometimes tender to percussion and palpation
nonresponsive to pulp vitality tests
periapical radiolucency
possibly associated with a sinus tract (if so then this is known as Suppurative Apical
Periodontitis)
Phoenix Abscess. The conditions associated with Phoenix Abscess are- chronic apical periodontitis that becomes acute
symptoms identical to acute apical abscess
periapical radiolucency
possible following treatment of a necrotic tooth
Periapical Osteosclerosis. The conditions associated with periapical osteosclerosis are-
low-grade, relatively asymptomatic inflammation of the periapical tissues
present with varied symptoms sometimes
often found in posterior teeth of young people
well-circumscribed radiopacity around root apices
If periapical osteosclerosis is asymptomatic and it responds to pulp vitality tests, root canal
therapy is not needed.
12
RECORD KEEPING
I. Provider Forms.
Dental Privileges Request Form. Each Schurz Service Unit Dental Provider – full-time employee,
contractor, or volunteer – must complete the Schurz Service Unit Dental Privileges Request Form and
submit this form to the Schurz Service Unit Dental Chief by October 1 st of each year (See Attachment #1).
In addition to this form, each provider must submit:
Copy of dental license (annually, by October 1 st or upon renewal)
Copy of current CPR card (annually, by October 1 st or upon renewal)
Copy of current AED card (annually, by October 1 st or upon renewal)
Indian Health Service, Schurz Service Unit Provider Form (after call to duty or contract approval)
Direct Deposit Sign-Up Form, SF 1199A (contractors only, upon approval of contract)
Copy of dental school diploma (initially, after call to duty or contract approval)
3 professional references (upon application)
Submission of these forms is the responsibility of the employee, and failure to submit these forms as
specified may result in revocation of clinical privileges.
II. Informed Consent.
Dental Examination Record, IHS 42-1. A well-written treatment plan (Part V), accompanied by detailed
notes in the Dental Progress Notes (IHS 42-2), may satisfy most informed consent requirements. It is
imperative that the patient, parent, or guardian sign the Dental Examination Record after the treatment plan
has been thoroughly discussed with the patient (or parent or legal guardian). Components of informed
consent during and after the examination process include:
Discussion of proposed treatment plan with the patient (or parent or legal guardian), including
risks, benefits, and costs – with documentation in the Progress Notes that this was done.
Discussion of treatment alternatives, including no treatment at all, and the risks, benefits, and costs
associated with the treatment alternatives – with documentation in the Examination Record and
Progress Notes.
Signature of the patient, parent, or legal guardian to constitute their acknowledgement of the
proposed treatment, treatment alternatives, and the risks, benefits, and costs associated with all
treatment modalities.
The patient should be clearly informed that the proposed treatment plan may be changed by either the
dentist or the patient during the course of treatment. The proposed treatment plan must be completed by
the treating dentist. See Attachment #2 for an example of the Dental Examination Record that includes a
treatment plan.
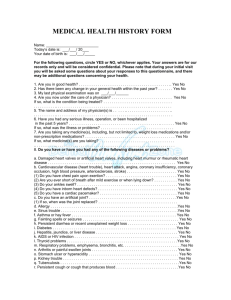
Dental Patient Medical History, IHS 41-1. The Dental Patient Medical History Form contains the
following consent: “I am indicating my consent for routine dental procedures such as x-rays, cleaning,
fillings, crowns, and local anesthesia by signing below.” This form most likely does NOT constitute legal
informed consent since treatment alternatives, risks, and benefits are not clearly written, and the document
contains generalized information rather than specific treatment modalities. Nevertheless, the treating
dentist should obtain the signature of a patient, parent, or legal guardian for “general” consent, and this
form should be updated at least annually, more to obtain an updated medical history than the element of
generalized consent. See Attachment #3 for an example of a properly completed Dental Patient Medical
History.
Child Health Care Record, Form 5, Dental Health (Head Start record). This form (see Attachment #4)
lists all treatment planned for the Head Start patient and is signed by the dentist who screens the patient
(usually in a Head Start center). This form does NOT appear to meet informed consent requirements in that
the treatment plan is not discussed with a parent or legal guardian – or in the very least there is no space for
the parent or legal guardian to sign the document – and the document does not have a place for treatment
alternatives, nor risks, benefits, and costs to the patient or parent. Therefore, this form should be used only
as an adjunct to the Dental Examination Record before treatment is rendered.
13
Patient Consent for Oral Surgery, IHS 513. The revised Oral Surgery Consent Form (Attachment #5)
should be used to obtain informed consent prior to any surgical procedure, including oral surgery or
periodontal surgery. The necessary elements of this form include:
The “Surgical Procedure” should be clearly written in language that the patient can understand.
For example, instead of “Extract tooth #14”, the dentist should write “Extract upper left first
molar.”
The dentist, not an auxiliary member of the dental team, must completely discuss the form with
the patient, to include verbally discussing each element – possible complications of the procedure,
disposal of the extracted tooth (if oral surgery), and risks if the procedure is not performed. As the
dentist verbally discusses each of these things – and it is recommended that the dentist read wordfor-word from the consent form – the dentist should also allow the patient to read the document.
The oral surgery consent form should not routinely be used as a freestanding document. In other
words, it is best to have a signed Dental Examination Record that accompanies the Oral Surgery
Consent Form (understanding, though, that the treatment of dental emergency patients may result
in the dentist using only the oral surgery consent form without the dental examination record).
Upon completion of the verbal discussion of the consent form, the dentist must allow the patient to
ask any questions of the procedure.
After the patient has had an opportunity to ask questions, the patient should sign under “Patient
Consent,” the dentist obtaining the consent should sign, and the dental assistant should sign under
witness – consequently, the dental assistant should be chairside when the dentist is discussing the
informed consent document in order to sign as a witness.
Patient Consent for Root Canal Treatment, IHS 941. . The Root Canal Consent Form (Attachment #6)
should be used to obtain informed consent prior to any endodontic procedure, including root canal therapy,
pulpotomy, pulpectomy, or apexification. The necessary elements of this form include:
Although “Tooth Number” is written, again the dentist should clearly indicate the tooth to be
treated using both the tooth number and the anatomical designation, i.e. “upper right first
bicuspid.”
The dentist, not an auxiliary member of the dental team, must completely discuss the form with
the patient, to include verbally discussing each element – possible complications of the procedure,
treatment alternatives, and risks if the procedure is not performed. As the dentist verbally
discusses each of these things – and it is recommended that the dentist read word-for-word from
the consent form – the dentist should also allow the patient to read the document.
The endodontic consent form should not routinely be used as a freestanding document. In other
words, it is best to have a signed Dental Examination Record that accompanies the Root Canal
Consent Form (understanding, though, that the treatment of dental emergency patients may result
in the dentist using only the root canal consent form without the dental examination record).
Upon completion of the verbal discussion of the consent form, the dentist must allow the patient to
ask any questions of the procedure.
After the patient has had an opportunity to ask questions, the patient should sign under “Signature
of Patient or Legal Representative,” the dentist obtaining the consent should sign, and the dental
assistant should sign under witness – consequently, the dental assistant should be chairside when
the dentist is discussing the informed consent document in order to sign as a witness.
In addition to the above requirements, it is suggested that the dentist use the revised consent form
that states that the “patient understands that root canal therapy takes two or more visits, and the
patient will be responsible for setting up the necessary appointments to complete the procedure.”
The purpose of this line is to hopefully further lessen the liability of the treating dentist – many
dentists have been successfully been held liable for not completing root canal therapy.
In the Dental Progress Notes, or on the endodontic consent form, the dentist should clearly
indicate that he/she has explained the long-term prognosis of the tooth (estimate, based on
Pathways of the Pulp or other sources or experiences) and should clearly dictate (and be
documented) to the patient that long-term success of the endodontically-treated tooth may depend
on the patient receiving coronal coverage (crown) following endodontic therapy, if determined to
be necessary by the treating dentist (such discussion must include the cost of the crown if the
patient is to be liable for laboratory fees).
14
IV. Other Dental Forms
PCC Ambulatory Encounter Record, IHS-803. The PCC is a form widely used in the IHS for medical
procedures, and is used in the dental clinics only to the extent of prescriptions. The PCC form (see
Attachment #7) should be completed by the treating dentist as follows:
1. Date/arrival time/clinic – should be completed by the dentist
2. On the right-hand side, the dentist should put “1” under affiliation, “56” under “Dis.”, and his/her
initials under “Initials/Code.”
3. The dentist should list the chief dental complaint but not necessarily complete the
subjective/objective section of the form (redundant, since this information is included on the
Dental Progress Notes).
4. Under Purpose of Visit, the dentist should list a diagnosis consistent with current ICD-9 diagnoses
under CDT-4, such as “chronic abscess, tooth #14.”
5. The dentist should clearly indicate the medications prescribed, using the following as an example:
Rx: Amoxicillin, 500mg
Disp: 30 (thirty) tablets
Sig: Take 1 tablet t.i.d.
6. The patient’s chart number and name should be in the lower left-hand corner, and the dentist
should sign the PCC.
Once completed, the dentist, dental assistant, dental hygienist, or receptionist may take the PCC, along with
the patient record, to the pharmacy. At no time should the patient be allowed to handle either the record or
the PCC form.
Dental Progress Note, IHS 42-2. The Dental Progress Note (Attachment #8)is the most important medicolegal document in the patient dental record, yet is often the most quickly and imprecisely written document.
The progress note should follow the “SOAP” format for all patients as follows:
“S” – subjective: patient’s chief complaint, in his or her own words
“O” – objective: clinical findings, radiographic findings, vitality test results
“A” – assessment: diagnosis, long-term prognosis
“P” – procedure: procedures performed by the dentist, including diagnostic tests, clinical
procedures, and disposition at the end of the appointment
While the full SOAP note isn’t required on return visits, it is mandatory for all initial visits (anytime code
0000 is to be used, or when a comprehensive dental examination is performed) and for all emergency
encounters. On return visits, the dental provider may simply use only the “P” to indicate the procedure
performed according to the signed treatment plan contained in the Dental Examination Record, IHS 42-1.
The Dental Progress Note should include all of the following for each patient visit:
Procedure code marked (note, for many procedures, the superbill does not contain the exact
procedure code, so the dental provider must use the ADA/IHS “Common Dental Procedure
Codes” to designate a code, such as: 1-surface posterior composite – “23__” changed to “2391.”)
Dental Progress Note written using the SOAP format as described above (the dentist may use the
back of the form if the front side is filled).
At a minimum, the patient name and chart number should be clearly written (or stamped) on the
lower left-hand corner.
The treating dentist or dental hygienist should sign the document, date it, and write the time of the
appointment down.
The patient’s Medical History must be reviewed at each dental visit (and a new Medical History
should be completed at least annually) and the dental provider should indicate the history has been
reviewed by marking the appropriate box on the lower right-hand corner.
Any medications prescribed to the patient should be indicated under the “P” of the progress note.
For every patient, the dental provider must indicate under “NV” (next visit) the anticipated
procedure (although this may change due to the wishes of the patient or provider).
Any anesthesia administered must be entered into the progress note, including the amount. For
example, “1.8 cc 2% Xylocaine with 1:100,000 epinephrine administered.”
15
For endodontically tested teeth, the progress note should indicate the control tooth in the “O”
section of the SOAP note, and should indicate both the pulpal and periapical diagnosis of the
tested tooth.
In addition to the above requirements, the treating dentist may wish to obtain additional consent during
certain procedures, such as removable prosthodontics, and this can be indicated on the Dental Progress
Notes. For example, if a dentist wishes to have the patient approve the wax try-in of a denture, he/she may
ask the patient to sign the Dental Progress Note indicating the patient’s approval. However, this is not a
requirement of the Dental Progress Note and is at the discretion of the treating dental provider.
The Dental Progress Note is a triplicate document. The white copy of the Dental Progress Note (original
copy) should be retained in the patient record, while the yellow copy should be used by the dental provider
to enter data into the Resource Personnel Management System (RPMS) and the pink copy should be
forwarded to the billing department of the tribal health clinic. Once the information from the yellow copy
has been entered into RPMS, the dentist should destroy this copy by paper shredder.
Dental Diabetic Data Form. The Dental Diabetic Data Form (Attachment #9) is a unique document
implemented by the Northern Nevada IHS Diabetes-Periodontal Disease Treatment Model Program Award,
and serves as the primary tracking document for all hygiene services provided to diabetic patients at
participating clinics.
Whenever a diabetic patient is provided a dental examination (initial or recall), or whenever a diabetic
patient receives any hygiene services (including prophylaxis, protocol cleaning, scaling and root planing,
periodontal maintenance procedure, debridement, and periodontal recall), or whenever a diabetic patient
receives a removable prosthesis, this form must be completed and signed by the treating dental provider.
It is not required, but is recommended, that the treating dental provider continue to use the same Diabetic
Data Form throughout the course of a patient’s treatment. Once the form is used, however, the dental
provider should maintain one copy in the patient record and submit one copy to the Project Officer on a
monthly basis as specified.
Periodontal Status Form. The Periodontal Status Form (Attachment #10) was approved by the Schurz
Service Unit in 2000 to replace the Periodontal Examination Record, IHS Form YYY (1993). The
Periodontal Status Form is to be used for any patient requiring full or partial-mouth periodontal probing
(see periodontal diagnosis and treatment modalities). The form charts three periodontal probing periods on
six sextants around each tooth, and should be completed as follows:
In Box A (or B or C), bottom section, periodontal pocket depth should be measured and
documented
In Box A (or B or C), middle section, gingival recession (or hyperplasia) should be measured and
documented
In Box A (or B or C), top section, mobility should be measured and documented
The patient’s name and chart number should be on the document, and the document is part of the
permanent dental record of the patient
The dates of any probings should be written adjacent to Box A, B, or C
A periodontal probing using this form must include the probing depth, recession index, mobility, and
indication of any furcation involvements. Additionally, the dental assistant or hygienist should clearly
mark all missing teeth that are not included in the measurements. If time allows, the dentist or dental
hygienist should indicate areas where there is evidence of bleeding upon probing by circling the pocket
measurement with a red pen or pencil, and, again, if time allows, the dentist or dental hygienist should use
the measurements of probing depth and recession index to draw an approximation of connective tissue
attachment for each tooth (this is very helpful in comparing radiographic and clinical findings, as well as
helping the patient visualize the extent of disease).
16
V. The Dental Record
Arrangement of the record. The written Dental Record should contain the following information, in order
from top of the chart to back:
Most recent Medical History Form (to help remind dentists to inquire about updates to the
patient’s medical history at the beginning of each appointment)
Most recent Dental Examination Record, including a consented treatment plan
Most recent Periodontal Status Form, if completed
Most recent Dental Diabetic Data Form, if completed
Most recent Dental Progress Notes (with procedural consent forms such as oral surgery behind to
the progress note indicating the procedure was performed)
Older Dental Progress Notes
Previous Medical History Forms
Previous Dental Examination Records
Radiographs
While this arrangement does not adhere to previous IHS guidelines, it allows for a logical approach to the
clinician. At the beginning of each appointment, the dentist will update the patient’s medical history,
followed by reviewing the treatment plan and continuing the prescribed course of treatment, followed by
other diagnostic forms, followed by progress notes.
Radiographs. Radiographs taken must be stored in a sealed envelope (to prevent misplacement when the
record is handled) and must meet the following guidelines:
Be properly arranged in a film holder
Contain the date, treating dentist’s name, the dental assistant or hygienist’s initials
For initial examinations, must include a minimum of four bitewing radiographs (if teeth are
present) and two anterior periapical radiographs (if teeth are present), for anyone over 6 years of
age (for younger patients, bitewings are acceptable if the patient complies)
For recall examinations, radiographs should be taken at least on an annual basis, to include
bitewings and anterior radiographs
For periodontal patients, a full-mouth series of radiographs is required
A panoramic radiograph, if available, is indicated for the mixed dentition patient, periodontal
patient, for the orthodontic patient (required prior to treatment in an IHS facility) and when the
dentist prescribes the film for other reasons.
For root canal therapy, the following radiographs are required for all endodontically-treated teeth:
initial radiograph (prior to access), working distance, final apical file, and final fill .
For all teeth requiring oral surgery, an appropriate periapical radiograph
For other complex procedures, as indicated by the treating dentist, an appropriate periapical
radiograph.
Patient Identification on each form. Each form in the patient dental record must contain the patient’s
name and health record number.
17
CLINICAL PROCEDURES
I. Rationale for the public health approach in the provision of dental services.
Public health dentistry is not simply the provision of clinical services in a public health setting (i.e., tribal
facility), but represents a commitment and responsibility of the dentist to provide services to a community
rather than to individual patients. Some of the major problems in our tribal settings include a severe
limitation on access to care for the majority of patients, inadequate staffing, and inadequate resources. The
public health dentist must, each and every day, take into account these problems while at the same time
addressing the historical disparities in oral health care provided to our Native American patients.
Each of our dental facilities in the Schurz Service Unit should operate under the guidelines of the IHS Oral
Health Program Guide, using sound public health principles in increasing access to care for all patients as
well as responsibly allocating the limited resources and staffing we possess. As a result of this strategy, we
may not fully address all of the oral health problems of a particular individual patient, but we will strive to
address many of the oral health problems of a particular community.
What follows are the guidelines for the provision of clinical services in the Schurz Service Unit – standards
of care.
II. Clinical Procedures.
Diagnostic procedures
A Comprehensive Dental Examination (ADA Code 0150) will consist of a hard tissue (caries)
examination, periodontal screening and recording (PSR/CPITN), soft tissue/oral cancer
screening, TMJ evaluation, at least two bitewing radiographs (over age 5, under age 5 if
possible), and a signed treatment plan.
A Limited Dental Examination (ADA Code 0140) will consist of a problem-focused
examination (emergency) and a radiograph (if applicable) of the problem area.
A Periodic Dental Examination (ADA Code 0120) will consist of a recall examination that
includes a caries examination, a periodontal screening, soft tissue/oral cancer screening, TMJ
evaluation, and a signed treatment plan. This code may also be used for an initial
examination when the requirements of a comprehensive dental examination as set forth above
(such as no radiographs taken) are not met.
The dentist should strive to perform at least one annual examination (comprehensive
preferably) on all patients entering the facility – this addresses all oral health needs of the
patient and is documented on the treatment plan. Patients interested in emergency care should
be encouraged to return for a complete evaluation; however, if patients desire only irregular
emergency care, this should be so indicated in the patient record.
If a facility has panoramic radiograph capabilities, a panoramic radiograph should be taken at
least every three years in the mixed and early adult dentition.
Service unit dentists should strive to increase access to care for certain target groups that are
at higher risk for disease development, including patients with diabetes (periodontal disease),
children under six years of age and their mothers (early childhood caries), prenatal moms
(periodontal disease, ECC education), elderly people (at risk for nutritional deficiencies due to
tooth loss), and adolescents (at risk due to traumatic dental injuries from sports or accidents).
This selective targeting can best be done working in collaboration with other clinic entities
such as the public health nurse, well-child clinic, diabetes coordinator, etc.
If a patient has been previously diagnosed with periodontal disease or the periodontal
screening indicates the need for further evaluation, the clinician should prescribe at least two
vertical bitewing radiographs at either the examination or follow-up appointment.
If the clinician performs pulp vitality tests (ADA Code 0460), he/she should record in the “O”
of the SOAP record the results of such tests as well as a control tooth.
18
Preventive procedures
Routine rubber-cup prophylaxes are discouraged, as they have been shown to be ineffective in
significantly reducing plaque. However, if the facility does offer this service as a way of
increasing patient satisfaction, and this procedure (ADA Codes 1110, 1120, 1201, and 1205)
can be done in 15 minutes or less at the examination/recall appointment, then it is within the
established standards of care. Conversely, if the procedure must be scheduled, or the dentist
takes excessive time to perform the procedure, this procedure represents a poor allocation of
resources (staff time, supply costs) and cannot be justified.
The dentist, if at all possible, should perform all routine preventive procedures at the
examination appointment, including prophylaxis, sealants, and any other preventive
procedures. Only in rare circumstances should a patient be scheduled an appointment for
routine preventive services. Note that the dentist or dental assistant should be providing
prophylaxes (some scaling of subgingival and supragingival calculus), and the dental
hygienist (if available) should not be used for these routine procedures. Instead the dental
hygienist should be utilized for more severe adult prophylaxes that require a lot of time, for
scaling and root planing procedures, for the provision of the diabetic periodontal protocols,
and for periodontal maintenance appointments.
Fluoride varnish (ADA Codes 1201, 1203, 1204, 1205) should be routinely applied to
children at moderate to high risk of developing carious lesions (see below) and to adults who
have root exposure or report hypersensitivity. Fluoride varnish will not be routinely applied
to all patients. Fluoride varnish applied to children will be in unit doses.
Fluoride prescriptions (ADA Code 1208) will be given to those patients at high risk of
developing caries and where access to fluoridated water is not available – it is the dentist’s
responsibility to determine fluoride exposure.
All patients reporting a history of tobacco use should be queried as to their interest in tobacco
cessation counseling (ADA Code 1320) and this should be documented in the record.
Pit and fissure sealants (ADA Code 1351) will be applied to patients at moderate to high risk
of developing caries (see below) and will be unfilled resin material (no glass ionomer to be
used). When applying sealants, the entire pit and fissure system on the tooth must be sealed
(i.e., for a mandibular molar, the occlusal surface and buccal pit). Regardless of risk
classification, the dentist should not apply sealants to patients he/she does not feel will return
at regular recall appointments (such as patients who have a history of broken appointments or
a history of frequent moves), due to the expected failure rate of 10-20% per year for sealants.
Although athletic mouth guards are coded miscellaneous (ADA Code 9940/9941), they are
preventive appliances, and should be fabricated for all patients that request them and who are
aged 8-18 and engaged in a sport or recreational activity that puts them at risk of dental
trauma. Additionally, those patients presenting with malocclusion, especially maxillary
protrusion, should be encouraged to wear protective mouth guards.
Risk classification. To be precise, taking into account several different models of caries risk
classification, the standard for the Schurz Service Unit will be as follows:
Very low caries risk – no history of caries
Low caries risk – no current lesions, a possible history of caries but adequate hygiene and
regular appointments.
Moderate caries risk – no current large carious lesions (maybe a small buccal pit), history
of several lesions (or tooth loss due to caries), or inadequate hygiene (moderate to heavy
plaque at the appointment)
High caries risk – one or more current carious lesions, history of several lesions, or
inadequate hygiene (heavy plaque)
For the purposes of standardizing procedures, and of targeting certain risk groups, the
only distinction that will be made is whether the patient is at low risk or moderate/high
risk of developing future caries (see above statements on targeting). If a patient is
determined to be at low caries risk, the use of preventive procedures (sealants, varnish,
etc.) is not recommended as it uses up resources that can be better used on targeting
moderate to high caries risk patients in the community.
19
Restorative procedures
Amalgam restorative materials (ADA Codes 2100 series) will not be used in restoring primary
teeth.
Primary teeth will be restored using primarily glass ionomer materials (Fuji II, Fuji IX, Fuji
Triage), especially if the Atraumatic Restorative Technique (ART) is used in preparing the
tooth.
Either composite resin or amalgam may used in service unit clinics, at the discretion of the
treating dentist. However, no compomer materials (Dyract) may be used at all.
All primary teeth with caries extending interproximally should be restored using a stainless
steel crown (ADA Code 2930).
Stainless steel crowns should be cemented with a glass ionomer cement and not IRM.
Preparing teeth for crowns typically is the most (or 2nd most) time-consuming procedure
performed in our dental facilities. Consequently, crown preparation and delivery, especially if
routinely performed, hinders access to care for other patients. Therefore, crown preparation
will follow these general guidelines:
Crown fabrication solely for the purpose of improving esthetics should not be performed.
Crown fabrication (or coronal coverage of some type) must be done following endodontic
therapy of the permanent dentition.
Crown fabrication may also be performed for other legitimate reasons such as a
removable prosthesis abutment, for fractured teeth, to restore vertical dimension after
diagnosed bite collapse (anterior or posterior), or due to large restorations with a
probability of fracture.
Crown fabrication solely for the purpose of treating temporo-mandibular joint
dysfunction is not recommended.
Before any crown procedure, the dentist must determine the patient’s periodontal status –
it is considered medical malpractice to prepare a crown for a tooth that has periodontal
disease.
In developing a treatment plan, the dentist must use sound reason to determine which, if
any, teeth should be crowned. Factors that play a role in this determination include the
patient load at the particular dental facility, the patient’s past compliance in keeping
appointments, the patient’s oral hygiene status, the overall condition of the mouth, and
the patient’s ability to pay for the crown and/or the follow-up prosthesis (in certain
service unit clinics, the patient must pay for laboratory fees for prosthetics).
The use of prefabricated posts is not recommended, as research has shown that often retention
is poor and the use of these posts predisposes teeth to fracture. However, prefabricated posts
can be used as provisional posts following endodontic therapy.
Temporary crowns may be provided to the patient for fractured teeth (ADA Code 2970), but
only if a follow-up appointment for the patient is made to resolve – extract, restore by another
material, or crown preparation – the problem.
The miscellaneous restorative code (ADA Code 2999) should not be used in the Schurz
Service Unit.
Sedative fillings (ADA Code 2940) are discouraged in the Schurz Service Unit. However,
when used, these materials can provide some relief of discomfort and allow the dentist more
time for an accurate diagnosis. Therefore:
Sedative fillings may be used to cover teeth where caries excavation is within 2 mm of
the pulp, but does not extend into the pulp – additionally the sedative may be used as a
liner for a permanent restorative material.
When a sedative filling is placed, the dentist is responsible for ensuring the patient is set
up for a follow-up appointment for final determination/final restoration.
20
Endodontic procedures
All patients desiring root canal therapy must have the Root Canal Therapy Consent Form
thoroughly explained to them and sign the form prior to the initial access.
It is up to the treating dentist to determine the viability of successful endodontic treatment for
his/her patient.
The dentist, once he/she has initiated root canal therapy, is responsible for completing
treatment – which means that the dentist or dental staff should set the patient up for a followup visit for obturation prior to the patient leaving the clinic that day. If this is not possible, the
dentist should not initiate root canal therapy. Several recent cases of litigation in the IHS
have occurred as a result of the dentist not completing root canal therapy.
The dentist must prescribe, and the dental staff take, a minimum of four radiographs during
root canal therapy – initial radiograph (prior to access), initial file/working distance, final
apical file, and final radiograph following obturation and placement of a provisional
restoration.
If a patient is unable to – for whatever reason, whether it be inability to pay or inability to set
up an appointment – have a crown or onlay fabricated following endodontic therapy for
posterior teeth in occlusion (stress-bearing areas), the dentist is discouraged from initiating
root canal therapy due to the possibility of tooth fracture.
Endodontic therapy will not include second or third molars in the Schurz Service Unit. For
patients requiring root canal therapy on second or third molars, the patient will be given the
option of either having the tooth extracted or receiving root canal therapy on the tooth outside
the service unit dental clinics, in which case the patient will be responsible for payment.
The use of the miscellaneous endodontic code (ADA Code 3999) is prohibited in the Schurz
Service Unit.
All patients receiving root canal therapy must be recalled at least annually, and the annual
exam should include a radiograph of the endodontically-treated tooth, adequate patient history
of the tooth, and clinical evaluation of the tooth.
The dentist should include two additional statements on the endodontic informed consent:
o “I understand that he/she is responsible for setting up a final appointment to complete
root canal therapy, and understands that if an appointment is not set up, the tooth has a
greater chance of root canal failure requiring an extraction in the future”
o {For posterior teeth in occlusion} “I understand that teeth requiring root canal therapy
may require the fabrication of a crown (cap), and that I am required to pre-pay for this
crown before root canal therapy can be completed.”
Periodontal Procedures
The diabetic protocol has been previously outlined (see periodontal diagnosis)
Periodontal surgeries (apically re-positioned flap, osseous surgery, gingivectomies, etc.)
should not be performed with adequate post-surgical flap coverage (PerioPack).
Scaling and root planing (ADA Codes 4341 and 4342) should not be coded unless anesthesia
is given. If anesthesia is not given and subgingival scaling is performed, the correct ADA
Code is 1110/1205 (adult prophylaxis with or without fluoride).
A gross (or general) debridement (ADA Code 4355) is to be used to prepare a patient for full
periodontal services – it is not a replacement for such services. If this code is used, anesthesia
may or may not be given, but at least one follow-up appointment involving scaling and root
planing (see definition previously) must be performed.
Atridox or other chemotherapeutic agents may be used following periodontal treatment or to
resolve a single periodontally-related problem (periodontal abscess).
All periodontally-treated patients should be set up on a recall system as determined by the
dentist. The recall visit should include oral hygiene reinforcement and maintenance with a
Piezon or hand instrumentation, depending on the patient’s condition.
The use of the miscellaneous periodontal code (ADA Code 4999) is not allowed in the Schurz
Service Unit.
21
Removable Prosthodontics
The use of Valplast or Flexite partial dentures, or clinic-fabricated acrylic partial dentures,
may be only of a provisional or temporary nature due to gingival stripping. If a patient elects
to have this type of partial denture fabricated, he/she must be told that it is a temporary partial
denture.
The denture or partial denture codes (ADA Codes 5100 series, 5200 series) may be coded
only at the conclusion (delivery) of the procedure.
The use of the miscellaneous prosthodontic codes (ADA Codes 5899 and 5999) may not be
used in the Schurz Service Unit.
Oral Surgery
Due to the geographic isolation of service unit clinics, third molar extractions, impacted or
not, may be referred on a case-by-case basis through Contract Health Services in the Schurz
Service Unit.
A surgical extraction (ADA Code Series 7200) involves the removal of alveolar bone with the
use of a surgical handpiece to section teeth or remove bone. Removal of alveolar bone using
elevators, Rongeurs, or other means does NOT constitute a surgical extraction.
The biopsy of clinically-observed lesions may be referred to an oral and maxillofacial
surgeon, utilizing Contract Health Services in the Schurz Service Unit.
Oral surgery should not be performed unless a thorough medical history is obtained, the
dentist or dental staff takes radiographs of the involved tooth (teeth), and the dentist has the
capability to provide adequate post-surgical analgesics.
Orthodontics
Comprehensive orthodontics requiring estimated treatment plans in excess of nine months are
not allowed in the Schurz Service Unit.
If a service unit dentist begins an orthodontic program, he/she must realize that he/she cannot
transfer duty stations or relocate without first completing orthodontic treatment on all patients
where orthodontics was initiated – failure to complete treatment may result in medical
malpractice for that provider.
The minimum requirements to begin orthodontics on a patient – whether removable or
brackets – are:
Panoramic radiograph (ADA Code 0330)
Diagnostic casts (ADA Code 8660)
Comprehensive dental examination and treatment plan (ADA Code 0150)
Orthodontic examination using IHS-approved forms (see attached) (ADA Code
0160)
Again, because orthodontics can consume many resources in the service unit dental facilities,
each clinical dentist should make sure he/she wants to start an orthodontic program, that
he/she has adequate training (a minimum of 30 hours of post-dental school training), and that
the program customized for the service unit dental facility allows for equal access to all
patients potentially requiring orthodontic care.
22
THE SCHURZ SERVICE UNIT CLINICAL GUIDELINES – STANDARDS OF CARE – IS A LIVING
DOCUMENT THAT MAY CHANGE PERIODICALLY DUE TO CHANGES IN MISSION,
PERSONNEL, OR INDIAN HEALTH SERVICE GUIDELINES. IF THIS DOCUMENT CONTAINS
CONTRADICTORY INFORMATION TO OTHER PUBLISHED INFORMATION, THE ORDER OF
PRECEDENCE IS:
1. Indian Health Service Oral Health Program Guide
2. Schurz Service Unit Clinical Guidelines – Standards of Care
3. Schurz Service Unit Policy & Procedures Manual
4. Other published information
Published: 29 September 2004
Amended: ________________
________________
________________
________________
(annual review required)
_________________
_________________
______________
______________
Note: For each amendment, the entire document must be reviewed and approved by the service unit dental
chief, service unit clinical director, and the Area dental consultant/director.
The Schurz Service Unit Clinical Guidelines-Standards of Care have been reviewed and approved by:
__________________________________________________________
Timothy L. Ricks, DMD, MPH SSU Dental Chief
_____________________
Date
__________________________________________________________
Stephen Mlawsky, MD, SSU Clinical Director
_____________________
Date
__________________________________________________________
Steven A. Tetrev, DDS, MPH, Phoenix Area Dental Consultant (Acting)
_____________________
Date
AMENDED: _________
The Schurz Service Unit Clinical Guidelines-Standards of Care have been reviewed and approved by:
__________________________________________________________
Timothy L. Ricks, DMD, MPH SSU Dental Chief
_____________________
Date
__________________________________________________________
Stephen Mlawsky, MD, SSU Clinical Director
_____________________
Date
__________________________________________________________
Steven A. Tetrev, DDS, MPH, Phoenix Area Dental Consultant (Acting)
_____________________
Date
23
I acknowledge receipt of the Schurz Service Unit Clinical Guidelines – Standards of Care, and have reviewed the
document:
__________________________________________________________
Name: Marlon A. Brown, DDS, Chief, Fallon Dental Program
_____________________
Date
__________________________________________________________
Name: Susan Wellman, DMD, Chief, Walker River Dental Program
_____________________
Date
__________________________________________________________
Name: Barbara Rosse, Dental Assistant, Walker River Dental Program
_____________________
Date
__________________________________________________________
Name: Pamela Spotted Wolf, Dental Assist, Pyramid Lake
_____________________
Date
__________________________________________________________
Name: Connie Baine, RDH, Contract Dental Hygienist
_____________________
Date
__________________________________________________________
Name: Stacie Swensen, RDH, Contract Dental Hygienist
_____________________
Date
__________________________________________________________
Name: Mark Rosenberg, DDS, MPH, Contract Dentist
_____________________
Date
__________________________________________________________
Name: Ivora Crutcher, Dental Assistant, Ft. McDermitt
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
__________________________________________________________
Name:
_____________________
Date
24
25