MOD_SCHILLACI_Phys Med prostate
advertisement

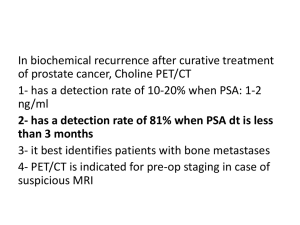
Role of nuclear medicine in the initial staging of prostate cancer. O. Schillaci, R. Danieli, L. Filippi, P. Nicolì, C. Manni, G. Simonetti Department of Biopathology and Diagnostic Imaging, University “Tor Vergata”, Rome, Italy For correspondence please contact: Orazio Schillaci,Viale G. Mazzini 121, 00195 Rome, Italy; e-mail: oschil@tiscali.it ABSTRACT The functional information provided by nuclear medicine imaging can be of value in staging patients with newly diagnosed prostate cancer. In fact, conventional imaging studies have demonstrated not very accurate in assessing the presence of regional lymph nodes and distant metastases. Bone scintigraphy is the most sensitive diagnostic tool for detecting bone metastatic lesions: however, it is not recommended for initial staging when PSA is below 20 ng/ml. Lymphoscintigraphy with sentinel node identification is a feasible and promising technique for preoperatively mapping the route of lymphatic drainage of prostate cancer. In111 capromab pendetide has been till recently used to assess lymph-node involvement, without reaching an elevated accuracy. Further studies are needed for confirming the potential role of Tc-99m bombesin in detecting node metastases. The role of PET in initial staging of prostate cancer is still under investigation: FDG demonstrated a low accuracy; therefore, other radiopharmaceuticals (i.e. acetate and choline) have been used, with very interesting preliminary results. Key Words: prostate cancer; nuclear medicine; initial staging. 1 INTRODUCTION Conventional imaging studies, including ultrasound, radiographs, CT and MRI have played a rather limited role in staging patients with newly diagnosed prostate cancer. Likewise, up to 40% of patients undergoing radical prostatectomy for presumed clinically organ-confined disease are found to have extraprostatic extension upon further pathologic staging [1]. Accurate staging before treatment is of the utmost importance because it permits the appropriate selection of therapy and increases the likelihood of a favourable treatment outcome. Nuclear medicine examinations can play an useful clinical role in staging lymph nodes (N-stage), and distant metastases (M-stage), using both SPECT (bone scan, lymphoscintigraphy, capromab pendetide and bombesin) and PET imaging. BONE SCAN Bone scintigraphy is based on the principal that actively metabolizing bone incorporates radiopharmaceuticals like Tc-99m diphosphonate, whose distributions is dependent on the rate of bone turnover and blood flow. This technique shows exquisite sensitivity for the detection of skeletal abnormality, therefore it is important in the initial evaluation of patients with malignancy, as the knowledge that metastases are present or not can alter subsequent management; the major limitation is that bone scan appearances are nonspecific. There is a remarkable affinity between prostate cancer cells and bone, which leads to this predominant pattern of metastasis, that are the most significant cause of morbidity and mortality in this disease, with an estimated 28,900 men die annually [2]. A recent review of literature data (23 articles) on bone scan in staging newly diagnosed prostate cancer has reported that bone metastases were detected in 2.3%, 5.3% and 16.2% of patients with PSA levels less than 10 ng/ml, from 10.1 to 19.9 and from 20 to 49.9 ng/ml, respectively [3]. Scintigraphy detected metastases in 6.4% organ confined cancer and 2 49.5% with locally advanced disease. Detection rates were 5.6% and 29.9% for Gleason scores 7 or less and 8 or greater, respectively. Therefore, considering this results, patients with low risk prostate cancer are unlikely to have metastatic disease documented by bone scan, and this investigation should not be standard practice. However, patients with PSA 20 or greater, locally advanced disease, or Gleason score 8 or greater are at higher risk for bone metastases and should be considered for bone scan. LYMPHOSCINTIGRAPHY AND SENTINEL NODE Questioning lymph nodes that drain areas of cancer is becoming standard practice in staging patients with neoplasms, and lymphoscintigraphy is an useful technique for mapping the route of lymphatic drainage of a tumour. The concept of sentinel lymph node relates to the fact that the tumour drains in a logical way through the lymphatic system, from the first to upper levels. A sentinel node is any lymph node that receives direct lymphatic drainage from a primary tumour. Therefore, the sentinel node will most likely be the first to be affected by metastasis, and a negative sentinel node makes it highly unlikely that other nodes are affected. The presence of pelvic lymph-node metastasis influences both the treatment and the prognosis of prostate cancer. Normograms only indicate a certain likelihood for organconfined disease, but they do not provide exact staging information in the individual patient. Lymph-node size both at CT and MRI does not correlate with the presence of metastases [4]. Therefore, no non-invasive diagnostic test could reliably differentiate patients with organconfined disease from those with metastatic lymph-nodes. In prostate cancer, because it is not known preoperatively which part of the organ the metastatic spread is originating from, the main aim of lymphoscintigraphy is the identification of all primarily draining lymph-nodes, inevitably comprising a single or more sentinel nodes. Wawroschek et al. [5] proposed the sentinel node concept in prostate cancer: the day before 3 lymphadenectomy, Tc-99m nanocolloids were transrectal injected into the prostate under ultrasound guidance, with one to 2 applications per prostate lobe; scintigraphic images were acquired 15-20 min and 2-4 h postinjection; sentinel node were intraoperative identified with a gamma-probe, and standard pelvic lymphadenectomy were performed after sentinel nodes’ removal. In a series of 117 patients [6], they found an average of 4 sentinel nodes per patient; a third of the sentinel nodes were located in the hypogastric, pararectal or presacral regions. Lymph-node metastasis were present in 28 patients: sensitivities of sentinel node identification and modified pelvic lymphadenectomy were 96% and 81%, respectively; in 64% of patients only sentinel node were positive. Moreover, this study showed individual variability in lymphatic drainage of the prostate and limited sensitivity for detecting lymphnode positive cases when the pelvic dissection area is limited. These data were confirmed in group of 350 patients (average PSA 12.7), 86 of whom had lymph-node metastases: only in 2 cases (false-negatives) metastases in non-sentinel nodes were found without at least one sentinel node being affected [7]. CAPROMAB PENDETIDE In–111 capromab pendetide makes use of a murine immunoglobulin monoclonal antibody, that recognizes the intracellular epitope of prostate-specific membrane antigen (PSMA), a 100-kd transmembrane glycoprotein almost entirely specific to human prostate epithelial cells. The sensitivity and specificity to detect lymph-node metastases are 60% and 70%, respectively; the major drawback is non-specific binding and high blood pool activity causing a low target to background ratio; therefore, it requires significant expertise in imaging interpretation [8]. BOMBESIN 4 Bombesin is a specific growth factor for prostate cancer, whose cells overexpress its receptors. Scopinaro et al. have labelled bombesin with Tc-99m, and they have used it in a small group of patients to evaluate lymph-node involvement with very promising results [9]. PET PET imaging with F-18 2-fluoro-D-deoxy-glucose (FDG) in tumours is based on the increase in glycolytic flux in cancer cells. FDG was found to have a low accuracy in primary staging of prostate cancer [10]. In particular, the limited sensitivity for prostate cancer lesions is probably due to fact FDG may selectively detect only more aggressive tumours, which depend on higher glucose metabolism [11]. Moreover, urinary excretion of FDG is the main drawback. So, other PET tracers, in particular choline and acetate, have been evaluated in patients with prostate cancer. Acetate uptake in tumour cells is related to lipid synthesis; it has been labelled both with C-11 and F-18. The lack of urinary excretion makes acetate suitable for prostate cancer PET: in fact, C-11 actetate resulted more sensitive than FDG in visualizing both nodal and bone metastases [12]. Also choline, which is needed for the synthesis of phospholipids in cell membranes, has been labelled both with C-11 and F-18. Intense bowel uptake can be observed with all choline compounds and so it can be difficult to accurately evaluate pelvic and abdominal lymph nodes involvement; moreover, the F-18 choline tracers show an early urinary appearance. Nevertheless, the first clinical data suggest that choline can detect more metastatic lymph nodes and bone metastatic lesions from prostate cancer than FDG [13-14]. In a study on 67 patients C-11 choline yielded a higher accuracy in the preoperative staging of pelvic lymph-nodes when compared to MRI/CT: 93% vs 86% [15]. The role of PET/CT in initial staging of prostate cancer is still under investigation. 5 REFERENCES [1] Karam J Karam JA, Mason RP, Koeneman KS,et al. Molecular imaging in prostate cancer. Cell Biochem. 2003; 90: 473-483. [2] Singh AS, Figg WD. In vivo models of prostate cancer metastasis to bone. J Urol 2005; 174: 820-826. [3] Abuzallouf S, Dayes I, Lukka H. Baseline staging of newly diagnosed prostate cancer: a summary of the literature. J Urol 2004; 171: 2122-2127. [4] Schoder H, Larson SM. Positron emission tomography for prostate, bladder, and renal cancer. Semin Nucl Med 2004; 34: 274-292. [5] Wawroschek F, Vogt H, Weckermann D, et al. The sentinel lymph node concept in prostate cancer - first results of gamma probe-guided sentinel lymph node identification. Eur Urol 1999; 36: 595-600. [6] Wawroschek F, Vogt H, Weckermann D, et al. Radioisotope guided pelvic lymph node dissection for prostate cancer. J Urol 2001; 166: 1715-1719. [7] Wawroschek F, Vogt H, Wengenmair H, et al. Prostate lymphoscintigraphy and radioguided surgery for sentinel lymph node identification in prostate cancer. Technique and results of the first 350 cases. Urol Int 2003; 70: 303-310. [8] Lange PH. PROSTASCINT scan for staging prostate cancer. Urology 2001; 57: 402-406. [9] Scopinaro F, De Vincentis G, Varvarigou AD, et al. 99mTc-bombesin detects prostate cancer and invasion of pelvic lymph nodes. Eur J Nucl Med Mol Imaging 2003; 30: 13781382. [10] Jana S, Blaufox MD. Nuclear medicine studies of the prostate, testes, and bladder. Semin Nucl Med. 2006;36: 51-72. [11] Agus DB, Golde DW, Sgouros G, et al. Positron emission tomography of a human prostate cancer xenograft: association of changes in deoxyglucose accumulation with other measures of outcome following androgen withdrawal. Cancer Res 1998; 58:30093014. [12] Oyama N, Akino H, Kanamaru H, et al: 11C-Acetate PET imaging of prostate cancer. J Nucl Med 2002; 43:181-186. [13] DeGrado TR, Baldwin SW, Wang S, et al. Synthesis and evaluation of (18)F-labeled choline analogs as oncologic PET tracers. J Nucl Med 2001; 42:1805-1814. [14] Price DT, Coleman RE, Liao RP, et al. Comparison of [18F] fluorocholine and [18F]fluorodeoxyglucose for positron emission tomography of androgen dependent and and androgen independent prostate cancer. J Urol 2002; 168: 273-280. 6 [15] de Jong IJ, Pruim J, Elsinga PH, et al. Preoperative staging of pelvic lymph nodes in prostate cancer by 11C-choline PET. J Nucl Med 2003; 44: 331-335. 7