Cervical Spondylotic Myelopathy Diagnosis And Treatment
advertisement

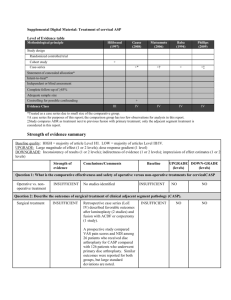
Cervical Spondylotic Myelopathy Diagnosis And Treatment Donald R. Johnson, II, M, D. and Steven C. Poletti, M. D. Introduction Myelopathy or dysfunction of the spinal cord is caused by degenerative processes of the cervical spine. Cervical spondylotic myelopathy is the most common cause of cord dysfunction in patients over 55 years of age. Degenerative changes within the disc and ultimately the osseous and soft tissue structures of the cervical spine cause encroachment and stenosis of the cervical cord. The disc, osteophytes, posterior longitudinal ligament, ligamentum flavum, facet joints, and the uncovertebral joints all contribute to this stenotic process. The typical AP diameter in the mid-cervical spine should measure greater than 15 millimeters, with a critical size for consideration of stenosis defined as being less than 13 millimeters. Additionally, the Pavlovнs ratio of canal diameter divided by the diameter of the adjacent vertebral body should be greater than 0.8. Numerous other measurement guides such as the spondylosis index and the compression ratio have been used to radiographically assess stenosis. Additionally, ligamentous laxity may allow subluxation of the vertebral body creating the so-called "pincher effect". The role of medullary ischemia as well as movement is poorly understood. The diagnosis of cervical spondylotic myelopathy is primarily based on a thorough history and examination. Patients may complain of difficulty walking with loss of balance and a wide-based gait. Often they have loss of dexterity and fine motor control of the hands. They may have, with movement of the neck, sensations of electrical shocks. Physical findings often are subtle. Early findings include mild cionus, decreased proprioception and disc dysdiadochokinesia. The so-called hand myelopathy signs are an important part of the examination. These include the finger abduction sign, hand release sign and Hoffinannнs sign. Late findings include spasticity, marked increased reflexes, gross balance and gain disturbance, and gross motor deficits. Generally speaking, upper motor neuron findings occur below the stenotic level while lower motor neuron findings occur at the stenotlc level. Clinical Materials From January 1991 to June 1995, 32 patients underwent surgery at our institution for cervical spondylotic myelopathy. The mean age was 60 years with a range of 38 to 75 years. Two patients underwent cervical laminectomy. Seven patients underwent anterior cervical discectomy and fusion with allograft iliac crest for a single level. Twenty-three patients underwent multi-level discectomy with one or more corpectomies followed by fibular allografi strut fusion. Additionally, twenty of these patients underwent anterior cervical plating. Surgical Technique ypically, the approach is made from the opposite side of the upper extremity with the most severe symptoms. The patient is placed supine on a doughnut with shoulders taped to the end of the table. An esophageal tube and perioperative Decadron are used. The procedure is done under magnification. A thorough decompression is done with removal of the posterolongitudinal ligament and complete exposure of the dura through all affected levels. Postoperatively, a drain is inserted and an ice pack is placed on the neck. The patient's head is elevated approximately 60 degrees and, by mouth, ice and cold liquids are started as soon as possible. A soft cervical collar is typically used and currently our patients are being treated under a 23-hour protocol for discharge. Fusions are done wholly with allograft bone. Fibular struts are used after corpectomies for more lengthy fusions while patella allograft is used for single level interbody fusions. The Synthes or Danek titanium plate serves as a buttress to prevent graft retropulsion; but, perhaps more importantly in our experience, has prevented the need for the use of a halo. Results Two patients had postoperative hoarseness which resolved within three months. No esophageal injuries, respiratory problems or graft retropulsions have occurred. Our mean follow-up on this group of patients is two years with a range of one to 5-1/2 years. Two patients were not improved but had a cessation of progressive deterioration of their symptoms. Thirty of the 32 patients felt they were significantly improved. All fusions have appeared to heal radiographically. No patients were left immobilized more than twelve weeks. 1 Discussion Historically, the general tendency has been to use anterior approaches for disease processes involving two or less levels and posterior approaches for multi-level disease2. In fact, many have recommended the use of posterior laminectomy or laminaplasty when more than two disc spaces were involved3. No hard statistical evidence exists, however, demonstrating the clear superiority of anterior or posterior surgical approaches. In fact, Graham's 1989 paper established a higher incidence of neurological complications with posterior approaches versus anterior approaches. Certainly, no one surgical approach is best for every situation. The approach should be tailored to the cause of the problem. Obviously, outside factors influence the surgeonнs choice of surgical approach. These may include the training of the surgeon, previous experience, familiarity with the surgical techniques and the surgeonнs general concept of the patientнs pathology. Conclusions Cervical spondylotic myelopathy must be in the differential diagnosis when examining a patient with spinal cord dysfunction, particularly in the elderly. Myelopathy unfortunately is under-diagnosed and under treated. Often, missing the diagnosis leads to increased disability as the spinal cord becomes more dysfunctional4. Multi-level anterior decompression can be done with minimal complications. With established myelopathy, the conservative approach is probably a surgical approach5. References Graham, JJ: Complications of cervical spine surgery. A five-year report on a survey of the membership of the Cervical Spine Research Society by the Morbidity and Mortality Committee. Spine, 1989;10:1046-50. Bibliography 1 Bohlman JBJS, 1999 2 Hardy, Neuroimaging Clin N Am, 1995 3 Law, Yale J Biol Med, 1993 4 Cates, J Manipulative Physiol Ther, 1995 5 Wang, Kao Hsiung I Hsueh Ko Hseuh Tsa Chih, 1997 2