Structuring the consultation
advertisement

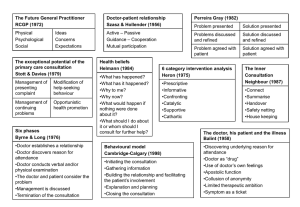
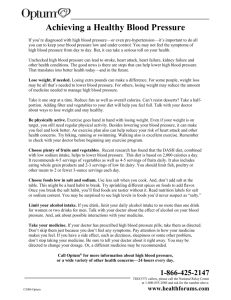
Structuring the consultation 2.1 02-04-2006 A short round of theory Consultations can be quite difficult and stressful for a GP: For instance: -you spend a lot of time in a consultation and apparently the patient is not satisfied at all -you give a lot of energy and at the end of the consultation the patient suddenly drops a bigger, even more complicated problem for which you lack the time and energy -whatever you do, you just don’t seem to understand what the patient wants from you -you are always running out of time The problem very often is, that we are all trained in a medical context. The patient however, even if he asks a medical question, is mostly not primarily interested in this medical context. The patient asks a medical question because he is visiting a doctor; he asks questions that you are supposed to ask a doctor. But behind those questions there is always another question (the reason for encounter). Technically: the patients has questions that originate from his own frame of reference. This is not always easily understood by doctors. We work within our own, medical, frame of reference. If the patient tells us that he has a headache, we tend to think that he wants a painkiller or something else to get rid of the pain. But that is not necessarily what the patient really wants. It is very important for the doctor to know what the reason for encounter is. If you know the reason for encounter you have a powerful weapon to organize your consultation and only then it is really possible to reassure the patient efficiently. You’ll find consultations more rewarding and you’ll feel you are dealing with consultations more professionally. Your patients will also be more satisfied: they’ll feel that the doctor really has listened to his problems, that he has been understood and he’ll be more willing to accept advice and / or reassurance. However to learn the reason for encounter you have to let the patient tell you this and you have to stimulate the patient to talk. This doesn’t go on endlesly of course: at all stages of the consultation you have to be in control. But the first part of the consultation, what is called the intake, is essentially the moment where the patients is stimulated to tell you everything that is important about his complaints. Whenever a consultation goes wrong, you can always find the roots of the problem in the intake. The basic structure of every consultation is as follows: 1. Intake The patient tells the doctor what his problem is and the doctor stimulates the patient to tell him everything about it. The doctor uses stimulating techniques. 2. Medical interview The doctor knows the reason for encounter, has a general idea about the problem of the patient and asks his medical questions (medical anamnesis) to check his hypothesis. The doctor uses directive questioning techniques with more or less closed medical questions. Medical examination might be part of this stage or may follow stage 3. This part poses the least problems. This is what doctors are trained to do. 3. Summarization The doctor sums up how he evaluates the problem and checks with the patient if he agrees. 4. Planning The consultation comes to a conclusion. The problem can be solved (prescription, referral, advice) or further appointments appear to be necessary. The doctor uses negotiation, information and advisory techniques. Intake The intake is that part of the consultation in which the patient tells why he is visiting you. For instance: most people with a headache will not see a doctor for their complaint. When a patient visits you he does so with a reason, for instance: -his neighbour was diagnosed with a brain tumor -his grandmother had a stroke -he is dysfunctioning on his work and he wants some time out -he has a sinusitis -he has a sinusitis and his grandmother had a stroke -he is afraid he has a brain tumor and wants an X-ray -he is afraid he has a stroke and wants to see a neurologist -he read about a new painkiller and wants to try that -he is afraid he has high blood pressure etcetera etcetera The list is endless and there is no way you can tell what the reason for encounter is, unless the patient tells you himself. And only when he told you he is afraid for a brain tumor, you are able to reassure him efficiently he doesn’t have one and you probably can do so without pointless referrals or X-rays. During the intake you use stimulating techniques. Stimulating techniques are for instance: -keeping eye contact -making stimulating sounds like “mmm”, “ I see”, “ oh yes” etcetera. -“parroting”: repeating the words of the patient in a questioning way. Patient: I have a headache. Doctor: You have a headache? -Refrasing: repeating the words of the patient in your own way. Patient: my child doesn’t want to eat and also I get a lot of complaints from the school about him misbehaving. Doctor: I understand your child gives you a lot of problems? -Summarizing: summing up what the patient said or how you feel what the content of the consultation is so far. Doctor: if I understand you correctly, you have this chestpain for over two weeks and it really bothers you in your day to day work, and basically you start to worry about this pain because you are afraid it might have something to do with your heart. Is that correct? -Asking open questions: open questions are questions you can’t answer with a plain yes or no or with straight factual information. Closed question: is this stomach pain on the left or on the right? How long do you have this headache? How much weight did you lose? Open question: could you tell me something more about this stomach pain? -Further questioning: after the first question on a subject you can continue asking in the same line. Doctor: You say you worry aboout the behaviour of your child. How does your husband feel about that? -Final summarization / formulating reason for encounter The intake ends with the finishing summarization and the doctor formulating what he feels is the reason for encounter. After summing up you give the patient time to agree or disagree with your summarization. If he disagrees or has yet to add some more information, the intake apparently is not finished, and you continue in the same line. Doctor: Okay, I think I have the picture clear. You have this headache for over a week and you worry it might be a brain tumor because your neighbour had one and that thought is sort of sticking in your mind. And now you would like to be referred for a brain scan just to be reassured. Is that correct? Patient: Yes, that sort of sums it up. Doctor: Okay. Then I would like to ask you some more questions and do some medical examination. (Doctor proceeds to stage 2: medical interview and examination). If you have any questions about this short round of theory of the intake feel free to ask your trainer. Practice 1. Think of a story to tell your colleague (some minor adventure on a holiday, something funny your children did, anything sort of personal). Tell your colleague this story. Your colleague uses no stimulating conversatioanl techniques whatsoever (doesn’t look you in the eye, doesn’t make stimulating sounds etcetera). Discuss afterwards how the story telling went and how you felt about it. What did the observer see? 2. Tell the story again. This time your colleague uses all the stimulating techniques he can think of. Is there a difference? 3. Role play. Think of a patient that you found sort of difficult (in this stage don’t take a completely deranged or extremely difficult patient). Try to realise for yourself why this patient was difficult. Play this patient in a role play. Your colleague plays the doctor and uses during the intake only stimulating techniques. That means he refrains from closed medical questions. If he doesn’t know anything to ask anymore he can ask for a time out and asks for suggestions from the observers. What sort of questions do you find difficult (“unnatural”, “artificial”) to ask? Can you find other, more natural ways to ask these questions? Play as many role plays as you feel like and change roles frequently. 4. Homework 1 Select two stimulating techniques to practice with. Try them out in your daily consultation and see what the effect is. If these techniques come to you more or less automatically, try some others. In your next group meeting discuss your experiences. Play out your experiences in a role play. Try out new techniques in a role play. Plan new techniques for your homework. 5. Homework 2 If you have come this far, try to formulate a final summarization of the intake and a reason for encounter in every consultation. Give the patient enough time to react on your summarization. If you like practice this in a role play. Discuss how things went in you group meeting.