choosing of ideal sealant for tract closure after tubeless
advertisement
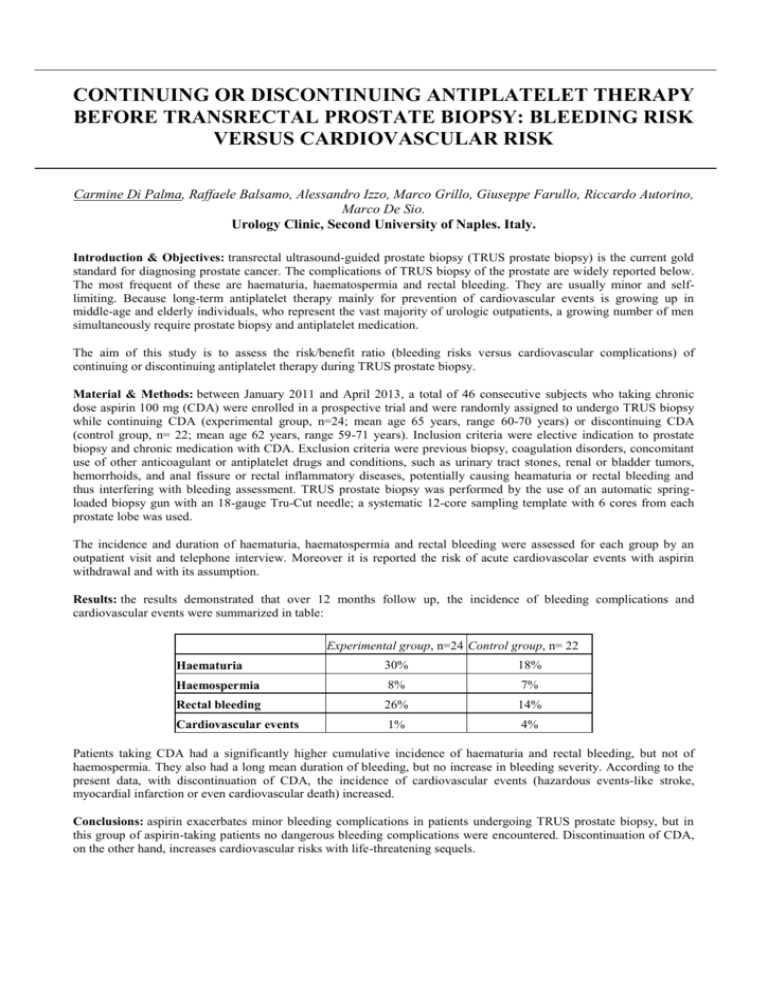
CONTINUING OR DISCONTINUING ANTIPLATELET THERAPY BEFORE TRANSRECTAL PROSTATE BIOPSY: BLEEDING RISK VERSUS CARDIOVASCULAR RISK Carmine Di Palma, Raffaele Balsamo, Alessandro Izzo, Marco Grillo, Giuseppe Farullo, Riccardo Autorino, Marco De Sio. Urology Clinic, Second University of Naples. Italy. Introduction & Objectives: transrectal ultrasound-guided prostate biopsy (TRUS prostate biopsy) is the current gold standard for diagnosing prostate cancer. The complications of TRUS biopsy of the prostate are widely reported below. The most frequent of these are haematuria, haematospermia and rectal bleeding. They are usually minor and selflimiting. Because long-term antiplatelet therapy mainly for prevention of cardiovascular events is growing up in middle-age and elderly individuals, who represent the vast majority of urologic outpatients, a growing number of men simultaneously require prostate biopsy and antiplatelet medication. The aim of this study is to assess the risk/benefit ratio (bleeding risks versus cardiovascular complications) of continuing or discontinuing antiplatelet therapy during TRUS prostate biopsy. Material & Methods: between January 2011 and April 2013, a total of 46 consecutive subjects who taking chronic dose aspirin 100 mg (CDA) were enrolled in a prospective trial and were randomly assigned to undergo TRUS biopsy while continuing CDA (experimental group, n=24; mean age 65 years, range 60-70 years) or discontinuing CDA (control group, n= 22; mean age 62 years, range 59-71 years). Inclusion criteria were elective indication to prostate biopsy and chronic medication with CDA. Exclusion criteria were previous biopsy, coagulation disorders, concomitant use of other anticoagulant or antiplatelet drugs and conditions, such as urinary tract stones, renal or bladder tumors, hemorrhoids, and anal fissure or rectal inflammatory diseases, potentially causing heamaturia or rectal bleeding and thus interfering with bleeding assessment. TRUS prostate biopsy was performed by the use of an automatic springloaded biopsy gun with an 18-gauge Tru-Cut needle; a systematic 12-core sampling template with 6 cores from each prostate lobe was used. The incidence and duration of haematuria, haematospermia and rectal bleeding were assessed for each group by an outpatient visit and telephone interview. Moreover it is reported the risk of acute cardiovascolar events with aspirin withdrawal and with its assumption. Results: the results demonstrated that over 12 months follow up, the incidence of bleeding complications and cardiovascular events were summarized in table: Experimental group, n=24 Control group, n= 22 Haematuria 30% 18% Haemospermia 8% 7% Rectal bleeding 26% 14% Cardiovascular events 1% 4% Patients taking CDA had a significantly higher cumulative incidence of haematuria and rectal bleeding, but not of haemospermia. They also had a long mean duration of bleeding, but no increase in bleeding severity. According to the present data, with discontinuation of CDA, the incidence of cardiovascular events (hazardous events-like stroke, myocardial infarction or even cardiovascular death) increased. Conclusions: aspirin exacerbates minor bleeding complications in patients undergoing TRUS prostate biopsy, but in this group of aspirin-taking patients no dangerous bleeding complications were encountered. Discontinuation of CDA, on the other hand, increases cardiovascular risks with life-threatening sequels. 30 25 20 15 Experimental group 10 Control group 5 0 Haematuria Cardiovascular events