Gastrointestinal Bleeding – Journal Summaries
advertisement

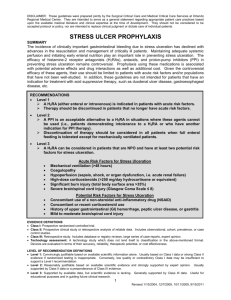
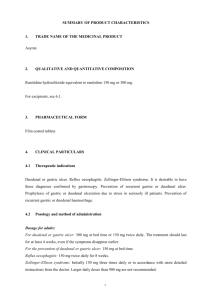
Gastrointestinal – Journal Summaries 22/7/10 VARICEAL BLEEDING Hayes, PC., et al (1990) “Meta-analysis of value of propanolol in prevention of variceal haemorrhage” Lancet 336:153-156 - meta-analysis of controlled trials looking at prevention of primary and secondary variceal bleeding propanolol works for primary prevention endoscopic band ligation for acute bleeding ULCER PREVENTION AND TREATMENT Lay, JY., et al (2000) “Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers” N Eng J Med 343:310-316 - double blind RCT - n = 240 - actively bleeding ulcers or non-bleeding visible vessels after treatment with adrenaline + thermocoagulation - omeprazole 80mg bolus -> 8mg/hr for 72 hours VS placebo - all patients received 20mg PO omeprazole for 8/52 - significant reduction in rate of bleeding within 30 days (most of which happened in first 3 days) in treatment group - no difference in mortality - no difference in number of patient requiring surgery Messori, A., et al (2000) “Bleeding and pneumonia in intensive care patients given ranitidine and sucralfate for prevention of stress ulcer: meta-analysis of randomised controlled trials” BMJ 321:1103-1106 - incidence of pneumonia and bleeding -> thought to be potential adverse effect of gastric acid suppression c/o bacterial overgrowth - small numbers in studies - no benefit from ranitidine vs placebo - no benefit from sucralfate vs placebo - increase risk of nosocomial pneumonia in ranitidine vs sucralfate -> muscosal ischaemia more important than acidity in stress ulcer formation -> despite this evidence use of PPI is widespread in critical care Parsonnet, J. et al (2005) “Clinician-discoverers – Marshal, Warren and H. pylori” N Engl J Med, 353:2421-2423 - acknowledgement of these guys discovery - H.pylori causes: chronic superficial gastritis, chronic active gastritis, peptic ulcer disease and gastric adenocarcinoma Jeremy Fernando (2011) Cook, D et al (1998) “A comparison of sucralfate and ranitidine for the prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation” Canadian Critical Care Trials Group, NEJM, 338:791-7 - MRCT - placebo vs ranitidine vs sucralfate -> GIH: placebo ( ), ranitidine (1.7%), sucralfate (3.8%) – P < 0.05 -> pneumonia incidence: ranitidine (19.2%), sucralfate (16.2%) – P > 0.05 -> no change in LOS or mortality Mariki, P. E. et al (2010) “Stress ulcer prophylaxis in the new millennium: A systematic review and meta-analysis” Critical Care Medicine: Volume 38 - Issue 11 - pp 2222-2228 Background - stress ulceration uncommon (1%) - prophylaxis may be unwarranted if feeding can be established early - prophylaxis may increase risk of hospital-acquired pneumonia and Clostrodium difficile infection - meta-analysis of RCT’s - histamine-2 receptor blockers vs placebo - 17 studies (1836 patients) - primary end point: clinically significant GIH - secondary end points: incidence of HAP and hospital mortality. - sub group analysis performed by grouping studies by enteral nutrition or no enteral nutrition -> significant decrease in risk of gastrointestinal bleeding (OR 0.47, p < 0.02) -> BUT only noted in a subgroup of patients who did not receive enteral nutrition (OR 1.26, CI 0.43-3.7) -> if patients fed, prophylaxis did not alter the risk of GI bleeding -> no increase in risk of HAP overall -> BUT, those who were fed had an increased risk of HAP (p 0.02, or 2.81) -> stress ulcer prophylaxis did not change mortality -> the subgroup who received stress ulcer prophylaxis AND enteral feeding had a elevated HAP rate (? both increasing gastric pH and thus allowing gastric multiplication of bacteria and subsequent aspiration) Internal Validity - clinically significant GIH was defined by each individual study - if there wasn’t a definition of clinically significant bleeding then endoscopic bleeding was used. - used H2 antagonists: cimetidine, ranitidine, famotidine - varying doses - some studies ran infusions - only 3 studies looked at enteral nutrition External Applicability - we use omeprazole - those who were fed may have been sicker than those that weren’t which may explain increase in HAP and death (confounding) Jeremy Fernando (2011) MY APPROACH - feed early unless contraindicated don’t use prophylaxis if feeding established if unable to establish enteral feed, risk assess for GIH: if high risk -> use prophylaxis if develops stress ulcers treat vigilance for the development of hospital acquired pneumonia may need to take ulcer prophylaxis of FASTHUG sticker! Jeremy Fernando (2011)