1. How, Where and When To Perform a Bronchial Biopsy? Clinical
advertisement

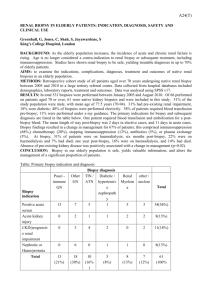
How, Where and When To Perform a Bronchial Biopsy? Clinical Applications. Petr Pohunek*, Katarína Urbanová*, Tamara Svobodová*, Jiří Uhlík**, Ludmila Hornofová*** *Division of Pediatric Pulmonology, Pediatric Department **Department ***Department of Histology and Embryology of Pathology and Molecular Medicine Charles University, 2nd Faculty of Medicine, University Hospital Motol, Prague Czech Republic Supported by the grant No. NT 11444 of the Internal Grant Agency, Ministry of Health, Czech Republic, and the Research Project MZ0FNM2005. Corresponding author: Prof. Petr Pohunek MD PhD FCCP Pediatric Department, University Hospital Motol V Úvalu 84 15006 Praha Czech Republic e-mail: petr.pohunek@LFMotol.cuni.cz Introduction. Sampling of tissue during bronchoscopy has been a long term established method of obtaining information about pathological lesions and processes in the bronchial mucosa. Main role of this technique is in the diagnosis of malignant tumors in adults. In children, bronchoscopic biopsy had been used much less frequently as the indications of bronchoscopy are mostly different to those in adults and tumors of the airways are rather rare. However, understanding of the importance of morphological description and confirmation of pathological processes in the bronchial wall in children with chronic bronchial pathologies has brought bronchial biopsy to an attention. Indications of bronchial biopsy. Flexible bronchoscopy has now been widely used in the diagnostics of respiratory pathologies in children of any age. Assessment of airway patency, excluding of congenital anomalies, stenoses and instability of the airways belong to the most frequent indications. These are usually well described using just visual investigation and anatomical evaluation, while morphological evaluation using a mucosal biopsy is not always necessary. Other indications comprise chronic respiratory symptoms, such as persistent or frequently recurrent pulmonary infiltrations, long-term coughing with or without production of sputum, and wheezing. In these cases, anatomical and visual evaluation is usually not sufficient and other methods are required to describe and diagnose the pathology more accurately. Among these usually the bronchoalveolar lavage and mucosal biopsy are very helpful. Targeted biopsy is extremely useful also in evaluation of abnormal intrabronchial structures or masses. Techniques of bronchial biopsy. Brush biopsy Brush biopsy is an endoscopic technique whose purpose is to sample superficial cells from the pathological lesions or, in diffuse disease, from the affected mucosa. It has been often used in adults for a diagnosis of malignant lesions, in children the indication is usually to sample material for cytological analysis of inflammation, evaluation of infection (e.g. tuberculosis) or to obtain viable cells for ciliary studies. The technique differs according to the size of used bronchoscope and its working channel. A standard protected brush technique can be used with the bronchoscopes with 2.2 mm channel. Thinner pediatric bronchoscopes (e.g. 3.6 and 2.9 mm scopes) are equipped with the 1.2 mm channel, therefore, only unprotected thin brushes can be used. To prevent losing of the sampled material during the withdrawal of the brush through the channel, the unprotected brushing is usually left as a last procedure during bronchoscopy and after sampling the brush is only just withdrawn into the channel and removed together with the bronchoscope. Then the brush can be pushed out again to remove the sampled material for further processing. Endobronchial biopsy Compared to brush biopsy, the aim of bronchial biopsy is to obtain a small piece of tissue that contains all the relevant structures and cells for appropriate histological analysis. In localized pathologies, such as visible endobronchial lesions, nodules or masses, the biopsy must be taken directly from the visible lesion. This may be difficult mainly in lesions that can be approached only with extensive flexion of the instrument or in some mucosal lesions not sufficiently protruding from the mucosa that require a tangential approach. Another technical problem limiting the yield of bronchial biopsy is the size of available forceps. This is not an issue when using bronchoscopes with the 2.2 mm channel. For these instruments, different types of reusable or single-use forceps are available. The most widely used type of forceps for pediatric bronchial biopsy is the fenestrated long oval cup forceps that usually provides sufficiently large sample for an appropriate histological evaluation. More difficult is to obtain an appropriate bronchial biopsy in smaller children while using a bronchoscope with the channel of 1.2 mm in diameter. Only few models of such thin forceps are available and due to their very small sizes, the bioptic samples are often inadequate. Nevertheless, there is a growing number of papers publishing the results of the analysis of sufficient bronchial biopsies in small children what suggests that with proper experience and technique and in a very good co-operation with the histological laboratory, also these small samples can be used for both diagnostic evaluation and research. The site for bronchial biopsy is derived from the expected pathology and visual assessment. In visible localized pathologies, the biopsy has to be taken directly from the lesion. In general pathologies, the site of biopsy is usually a properly accessible site with a possibility of a good grasp by the forceps. This is mostly any of the interbronchial carinas, where the positioning of the forceps and the embedding into the mucosa is better that anywhere else. To avoid distortion of the histological result by possible secondary changes, it has been recommended to avoid sampling from the main carina or from the origin of the right upper lobe bronchus. It is always better to sample more specimens (usually 3-4) to make sure that at least some will be adequate for analysis. Processing of the histological specimen. The sequence of processing depends largely on the purpose of the biopsy and expected staining and analysis. For simple morphological analysis, the sampled tissue can be immediately fixed in formaldehyde and transferred to the laboratory for embedding, cutting and staining. For basic evaluation, the standard hematoxylin-eosin staining is usually sufficient; however, some targeted staining protocols can be used for more detailed analysis. Among these, mainly stainings for collagen and other matrix proteins or stainings emphasizing mucus producing elements can be useful. For research analysis, the immunohistochemistry has been frequently used, mainly for analyzing cell populations of special interest or various extracellular or intracellular proteins (tenascin, fibronectin, metalloproteinases, growth factors). The material intended for the immunohistochemical analysis should be fixed by buffered paraformaldehyde rather than standard formaldehyde and the fixation should not be prolonged (optimum 4 hours). In special indications, such as ciliary structural studies, the specimen can be processed for ultrastructural analysis using electron microscopy. In this case, special protocols and fixatives are used. The yield of bronchial biopsy. Bronchial biopsy is certainly an unique method for evaluation of endobronchial masses and confirming or excluding possible neoplasms. It may help in diagnosing other non-malignant endobronchial pathologies, such as tuberculosis, sarcoidosis, virus-induced lymphoproliferation, granulations etc. In general non-malignant pathologies, most of the recent studies using bronchial biopsies in children have focused upon asthma and analysis of remodeling of bronchial wall in children with asthma of different severity. These studies have confirmed presence of eosinophilic inflammation, deposition of matrix proteins and increased mass of bronchial smooth muscle and vascularity (1 - Barbato). Some of these studies confirmed presence of such changes even before the clinical diagnosis of asthma or in children with only intermittent symptoms (2 Pohunek, 3-Barbato). From purely research approach, this has been now more and more used also in clinical evaluation in differential diagnosis of obstructive symptoms in children. Presence of cellular infiltration and marked signs of remodeling can support the diagnostic and therapeutic decisions in children with atypical symptoms. Inflammation and epithelial damage in the bronchial mucosa can also be detected and assessed in other pathologies, such as recurrent or chronic bronchitis. The quantitative histological data compared with clinical results in a well designed study showed extensive epithelial damage, shedding and edema in children with recurrent bronchitis.(4) This histological finding proved that children with recurrent bronchitis can develop severe bronchial inflammation and have a reduced epithelial integrity and depressed mucociliary function. Safety of bronchial biopsy in children. Safety concerns were apparently the main reason why routine use of bronchial biopsy was slowly accepted as a possible supplemental method in pediatric flexible bronchoscopy. However, growing experience with this method in children proves that correctly indicated and properly performed endobronchial biopsy does not add any significant risk to that inherent in the bronchoscopy itself. In a large safety study by de Blic analyzing more than 1300 flexible bronchoscopies in children, the authors encountered one pneumothorax associated with endobronchial biopsy, which was not reported in another rather large study that analyzed safety of 170 bronchial biopsies in children aged 2.5 to 16 years with chronic respiratory symptoms. In this study the authors did not report any significant complication, such as pneumothorax, bleeding or subsequent fever. The possibility of adverse effect of such procedure should, however, be always on one´s mind. Especially in situations with expected increased fragility and increased vascularization, the risk of bleeding or bronchial perforation might be theoretically higher. On the other hand, performing a routine coagulation screen in patients without clinically apparent bleeding disorders was proven unnecessary when endobronchial biopsy was planned. Taking bronchial biopsy has been shown to prolong flexible bronchoscopy by about 5 minutes; this might be relevant in children with impaired ventilation. References 1. Barbato A et al. Epithelial Damage and Angiogenesis in the Airways of Children with Asthma. Am J 2006; 174: Respir Crit Care Med. 975-981 2. Pohunek P. et al. Markers of eosinophilic inflammation and tissue re-modelling in children before clinically diagnosed bronchial asthma. Pediatr Allergy Immunology, 2005; 16 (1): 43–51 3. Barbato A et al. Airway Inflammation in Childhood Asthma. Am J Respir Crit Care Med. 2003; 168: 798-803 4. Gaillard et al., Airway epithelial damage and inflammation in children with recurrent bronchitis. Am J Respir Crit Care Med. 1994; Sep;150(3):810-7 5. Salva P et al., Safety of endobronchial biopsy in 170 children with chronic respiratory symptoms. Thorax. 2003; 58(12): 1058–1060