Electrical-Stimulation
advertisement

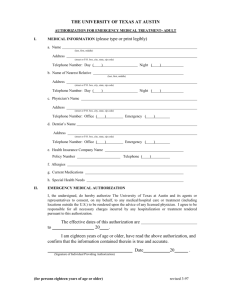
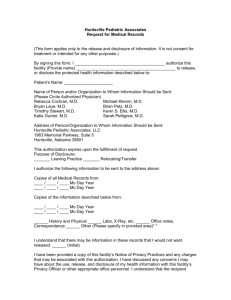
Electrical Stimulation Devices Revised: 12-09-2013 Overview Eligible Providers Eligible Recipients Covered Services Noncovered Services Authorization Billing Overview Electrical stimulation devices are suggested for treating musculoskeletal dysfunction, pain or disease. Electrical or electromagnetic devices for wound care are addressed in the specialized wound therapy section of the MHCP Provider Manual. Transcutaneous electrical stimulation devices are addressed in the TENS section of the MHCP Provider Manual. Eligible Providers Medical suppliers Indian Health Services Federally Qualified Health Center Rural Health Clinic TPL and Medicare Providers must meet any provider criteria, including accreditation, for third party insurance or for Medicare in order to assist recipients for whom MHCP is not the primary payer. MHCP quantity limits and thresholds apply to all recipients unless only Medicare co-insurance or deductible is requested. Eligible Recipients Covered electrical stimulation devices are covered for all eligible MHCP recipients. Covered Services Incontinence treatment systems Codes: E0740: incontinence treatment system, pelvic floor stimulator, monitor, sensor and / or trainer Pelvic floor stimulators are covered with authorization for recipients with stress, urge or mixed incontinence who have undergone a documented trial of pelvic muscle exercises for a period of at least six months with no significant improvement in incontinence. Neuromuscular stimulation for scoliosis Codes: E0744: Neuromuscular stimulator for scoliosis Neuromuscular stimulators are covered for recipients with juvenile or adolescent single or double major idiopathic scoliosis, who are at risk for curve progression and whose curvature is between 25 and 40 degrees. Neuromuscular stimulators may be covered for recipients in the 20 to 25 degree range if there is a documented progression of curvature of at least 5 degrees in the preceding six months. Neuromuscular stimulators Codes: E0745: Neuromuscular stimulator, electronic shock unit Neuromuscular stimulators are covered with authorization for treatment of disuse muscle atrophy where nerve supply to the muscle is intact and where there is a non-neurological reason for the disuse atrophy. Functional electrical stimulators Codes: E0770: Functional electrical stimulator, transcutaneous stimulation of nerve and / or muscle groups, any type, complete system, not otherwise specified Upper extremity functional electrical stimulators (e.g. NESS H200, Handmaster) are covered with authorization when documented improvement has been shown in the supervised rehabilitation setting for patients with upper limb paralysis due to cervical spinal cord injury or chronic upper extremity paresis due to stroke. Noncovered Services Pelvic floor stimulators are considered investigative for recipients who do not have stress, urge or mixed incontinence. Pelvic floor magnetic stimulation devices (e.g. ExMI, NeoControl Pelvic Floor System) are considered investigative. Neuromuscular stimulators for scoliosis are not medically necessary for recipients with curvature less than 20 degrees. Inferential current simulators (e.g. RS-4i) for use in the home are considered investigative for all indications. Cranial electrotherapy stimulation (e.g. Alpha-Stim, CES Ultra) is considered investigative for all indications. Electrical or electromagnetic stimulation for the treatment of osteoarthritis or rheumatoid arthritis (e.g. BioniCare Bio-1000) is considered investigative. Use of neurofeedback/EEG biofeedback devices in the home is considered investigative. Use of an electronic salivary reflex stimulator is considered investigative, not the standard of care and not an effective use of Medicaid dollars. Non-invasive nerve stimulators for treatment of nausea (e.g. ReliefBand, PrimaBella) are considered investigative. Use of the Sympathetic Therapy System (e.g. Dynatron STS) is considered investigative for all indications. Use of electroceutical/bioelectric nerve block is considered investigative for all indications. Use of an upper extremity functional electrical stimulator in the home setting for indications other than specified above is considered investigative. Use of a lower extremity functional electrical stimulator in the home setting (e.g. ParaStep, NESS L300, WalkAide) is considered investigative. Use of functional electrical stimulators designed as ergometers (e.g. StimMaster, ERGYS, REGYS, RT300) is considered investigative and not the prevailing standard of care for any condition. Electrical stimulation devices used for cancer treatment are considered investigative, not the standard of care and not an effective use of Medicaid dollars. Authorization Authorization is always required for pelvic floor stimulators. Documentation must include the type of incontinence and a trial of pelvic muscle exercises for a period of at least six months with no significant improvement in incontinence. Authorization is required for repairs to neuromuscular stimulators for scoliosis if the submitted charge is over $400. Authorization is always required for neuromuscular stimulators. Documentation must clearly show the reason for the disuse atrophy, and must demonstrate that the nerve supply to the affected muscles is intact. Authorization is always required for functional electrical stimulators for the upper extremities. Documentation must clearly show upper limb paralysis due to cervical spinal cord injury or upper extremity paresis due to stroke. There must be improvement shown in the supervised rehabilitation setting when using the functional electrical stimulator device. Submit authorization requests through MN–ITS (Authorization Request 278). Fax the MN–ITS response with the required documentation, physician’s orders and appropriate additional information to the medical review agent. Write the MN–ITS Authorization Request number on each page of each document. Billing Use X12 Batch or MN–ITS 837P Professional electronic claim Report the ordering provider in the Other Provider Types section of the MN–ITS Interactive claim If the recipient has Medicare, MHCP will pay only the deductible / co-insurance on any item for which Medicare made payment, regardless of any MHCP prior authorization. Shipping / delivery/ set-up costs are included in the MHCP maximum allowable payment and may not be separately billed to MHCP or the recipient. When billing labor for repairs, specify the number of units and the hourly rate. Do not bill for setup and delivery, or for service calls that do not involve actual labor time for repairs. When billing for items approved on a prior authorization, make sure the HCPCS codes, modifiers, and descriptions on the claim match the same information on the prior authorization. Enter the authorization number in the authorization field for each line Submit the usual and customary charge for each line, not the approved amount from the authorization letter. Payment will be the balance of the lesser of the billed amount or the approved amount after any primary or secondary payers have made payment.