Brig Royd Osteoporosis Protocol
advertisement
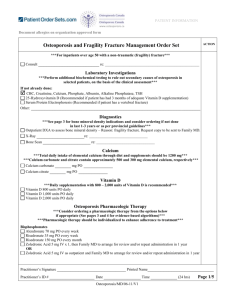
Brig Royd Osteoporosis Protocol (Updated December 2014) Osteoporosis is defined as systemic skeletal disorder, characterised by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture DEXA definition - A ‘T-score’ of ≥ 2.5 standard deviations (SD) below the young adult mean has been classified as osteoporosis by the World Health Organisation (WHO). Overall fracture risk increases two-fold per unit SD decrease in BMD and this relationship is even greater for hip fractures and BMD measured at hip sites. In terms of T scores, a score of -2.5 or less confirms osteoporosis, between -1 and -2.4 confirms osteopaenia. Identifying patients at high risk of osteoporosis Clinical risk factors: Age Gender Low BMD Previous fragility # Parental history of hip # BMI < 19 Hormonal – premature menopause, prolonged amenorrhoea (not related to PCOS or pregnancy), use of depot provera > 5 years. Includes men post-orchidectomy/androgen deprivation/hypogonadism Drugs – oral steroids (any dose of oral corticosteroids for >3/12 OR 1 g Prednisolone or equiv. lifetime dose.) GnRH analogues, arimidex, anticonvulsant therapy, Glitazones, PPIs Lifestyle – smoking and alcohol intake (>3 units/day), immobility, Medical conditions – rheumatoid arthritis, IBD, Malabsorption, cystic fibrosis, hyperthyroidism, hyperparathyroidism, Cushing’s syndrome, vit D insufficiency, COPD, Type 1 DM, Chronic renal and hepatic disease. Consider using Qfracture - http://www.qfracture.org/index.php (or FRAX via systmone) Primary Prevention Women aged < 45 with recent premature menopause = HRT until 52 (unless contraindicated). Not for DEXA unless other risk factors Women aged > 50 and Men aged > 65 who have clinical risk factors: FRAX calculation o Low risk (<10%)– lifestyle advice, consider Qfracture repeat after 5 years unless risk factors change o Higher risk (>10%) – DEXA referral DEXA PIL http://www.patient.co.uk/health/dexa-scan Frail/>75 with clinical risk factors Falls assessment Check Vit D and calcium and consider further investigation if an underlying cause suspected. (e.g FBC, ESR, Electrolytes, Bone profile, TFTs, PTH, ALP, Coeliac screening) Treat without DEXA (as per 2° prevention) PMR Individuals > 65 or hx of prior fragility fracture - DEXA not required use bisphosphonate and calcium & vitamin D Individuals < 65 - Start calcium & vitamin D, DEXA scan and consider bisphophonate if T score less than -1.5 Secondary prevention (1) Women aged > 50 or men aged >65 with low trauma fracture DEXA referral Follow scan report recommendations (2) If abnormal DEXA but no history of # FBC, ESR, Electrolytes, Bone profile, TFTs, PTH, ALP, Coeliac screening, Oestrodiol (amenorrhoeic pre-menopausal), testosterone (men), Vit D Follow scan report recommendations. Treatments in order of preference: (from NOGG and NICE) (1) Alendronate (once weekly) (2) Risedronate (once weekly prep) – n.b ?often better tolerated and now off patent, but still second line as per NICE – (?likely to change with next guidance) (3) Consider ibandronate (once monthly) (4) Strontium (caution re VTE/CVD) – see link below; these patients should be reviewed every 6 months to reassess vascular risks (5) Raloxifene - not licensed for primary prevention, but is for secondary prevention in certain circumstances ( BNF osteoporosis treatment) All plus calcium/vit D – Calderdale formulary recommends generic coleclciferol 400unit/Calcium carbonate 1.5g chewable tablets BD (equivalent of adcal D3) If none of above tolerated – refer to rheumatology for advice. (?denosumab/teriparatide) PIL for patients on different treatments in osteoporosis (National Osteoporosis Society) Repeating DEXA - In line with PACE guidance (&BMJ) patients with osteoporosis should have a scan every 3 years and those with osteopaenia every 5 years. (please create patient alert with date of next DEXA and consider adding reminder to repeat prescriptions) Brig Royd Codes to use. (1) Referral for DEXA = /dexa (2) Fragility fracture = /fracture (3) T score = /dexat (4) Osteoporosis = /osteo QOF 2015/16; unchanged ( but remember to code DEXA results if osteoporotic as well as fragility fracture) OST001 OST002 OST003 The contractor establishes and maintains a register of patients: 1. Aged 50 or over who have not attained the age of 75 with a record of a fragility fracture on or after 1 April 2012 and a diagnosis of osteoporosis confirmed on DXA scan, and 2. Aged 75 years or over with a record of a fragility fracture on or after 1 April 2012 The percentage of patients aged 50 or over who have not attained the age of 75, with a fragility fracture on or after 1 April 2012, in whom osteoporosis is confirmed on DXA scan, who are currently treated with an appropriate bone-sparing agent. The percentage of patients aged 75 or over with a fragility fracture on or after 1 April 2012, who are currently treated with an appropriate bone-sparing agent. links for more info http://cks.nice.org.uk/osteoporosis-prevention-of-fragility-fractures#!scenario http://www.osteoporosis-resources.org.uk/ http://www.shef.ac.uk/NOGG/NOGG_Pocket_Guide_for_Healthcare_Professionals.pdf http://www.nos.org.uk/page.aspx?pid=264&srcid=234 DRUG HOLIDAYS The following guidance is taken from the National Osteoporosis Society and seems to be in line with current practice. Bisphosphonates have a long half-life in bones and their effects continue for some years after stopping. Due to concerns about atypical femoral fractures and osteonecrosis of the jaw a drug holiday should be considered after 5 yrs of treatment. Some patients may require long term treatment ( eg patients with multiple v ertebral fractures, treatment with high dose steroids, or patients with very low BMD at outset).The benefits are likely to outweigh the risks. NOGG guidance suggests a review of patients after 5 years treatment with alendronate or risedronate. This review should include the re-assessment of fracture risk in treated individuals using the FRAX tool, combined with a repeat DEXA as necessary, before deciding if continuing treatment is appropriate. Arrange DEXA after 5 yrs of treatment. If BMD same/improved/>2.5 withdraw treatment for 2-3 years then reassess with DEXA Fracture risk should be reassessed after any new fracture or every 2 years. Consider restarting treatment if fracture risk increases. If fracture risk is still above the intervention threshold; continue treatment for another 5 yrs. DENOSUMAB This is now under shared care scheme and GP responsibilities include Ensure compliance with vitamin D/ calcium Have recall system for 6 monthly injection Early treatment of skin infections/cellulitis which is an increased risk. Delay any invasive dental treatment until just before 6 monthly injection Refer back to specialist after 5 years.