SURGICAL TECHNIQUES - Materials Technology
advertisement

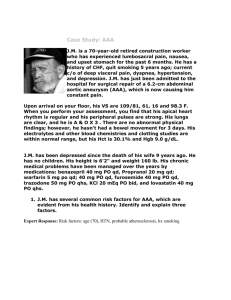
Chapter 3 Surgical Techniques ___________________________________________________________________________ CHAPTER 3 Surgical Techniques 3.1 Introduction Aneurysmal dilatation of the aorta is an irreversible pathological finding: the norm is further expansion, except in some individuals where slow growth is visible by imaging. Fascinating studies from Japan suggest that aortic aneurysms might grow biphasically, i.e. slow initially, then rapidly and that the growth curve can be expressed as a bi-exponential equation. These studies reiterate that an aneurysm may rupture at any time and at any size: there is currently no exact measurement that can precisely predict when this might occur. Size appears to be the best predictor of rupture [Don F. du Toit, 1999]. Aneurysm formation and danger of rupture are illustrated by Laplace’s Law Expansion of an aneurysm is demonstrated by the following equation: T = Pr. The larger is the vessel radius (r), the larger is the wall tension (T) required to withstand a given internal fluid pressure (P). As an aneurysm expands, the tension on the aortic wall increases. Studies have also shown that aortic aneurysms grow faster shortly before rupture. Surgery for abdominal aortic aneurysms is recommended if patient’s aneurysm is larger than 5 cm, nowadays there are two kinds of surgical techniques, one referred as “open surgery” and the other as “endovascular surgery”. 27 Chapter 3 Surgical Techniques ___________________________________________________________________________ Although the former is a much older treatment than the latter (the first open surgery treatment of AAA dates back to the fifties, whereas the less-invasive endovascular treatment was performed for the first time in 1991), both of them are widely adopted to treat the AAAs, this because the surgery team is often forced to chose rather one than the other. For endovascular repair (EVR) the aneurysm should have suitable anatomy. If certain anatomic characteristics are not met, open surgery is the only option. Endovascular treatment may seem always a better choice than the open surgery; unfortunately only 15-30% of aneurysm patients are candidates for endograft placement. Anatomic limitations for the placement of a common stent-graft include aneurysms that involve the renal arteries, aneurysms with extremely short necks, iliac vessels that are less than 7 mm or greater than 13.4 mm in diameter, densely calcified vessels, very small femoral vessels, and severe angulations of the aneurysm neck. These limitations make preoperative measurement and evaluation of the aneurysm very important; consequently, both conventional angiography and CT angiography need to be performed. These imaging procedures can be performed on an out-patient basis. In summary, endograft placement allows 15-30% of abdominal aortic aneurysms to be treated by a less invasive procedure that means with a decrease in morbidity when compared to open surgical repair. 3.2 Open surgery This method has been performed exclusively for almost 50 years and is one of the most successful and durable operations. At operations the diseased part of the aorta is replaced with a Dacron or Teflon graft that carefully matches to the normal aorta and sutured in place by the surgeon. While ultimately curative, this is an operation that requires a major abdominal incision and general anesthesia, and the hospital stay averages 7-10 days for most patients. Even after uncomplicated surgery, it is often 6-8 weeks before patients can return to a full and normal life. 28 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.1 Differences between incisions for the open surgery (on the left) and for the endovascular one (on the right). The length of the incision in surgery has a great relevance for the risk of infections during the surgery itself. On this point of view the open surgery has a completely different approach. Fig. 3.2 This is how an aneurysm appears to the surgeon just before clamping the proximal part of the aorta. It is possible to see how much the sac is stretched, the diameter is more than 5 cm and the risk of rupture is high. 29 Chapter 3 Surgical Techniques ___________________________________________________________________________ Surgery to remove an aneurysm is one of the most common vascular procedures; the operation is usually completed in less than two hours. General anesthesia is given, so the patient will not be awake and will not feel anything. First the surgeon exposes the aneurysm via an incision in the abdomen of about 17 to 25 cm long (fig. 3.1, 3.2). The aorta is clamped above and below the aneurysm to prevent bleeding. The aneurysm is then opened (fig. 3.3). Any clots and fatty deposits that have lodged in the aneurysm are removed. A synthetic graft-usually a straight, Dacron woven tube is sutured to the aorta above and below the aneurysm (fig. 3.4). Fig. 3.3 Fig. 3.4 30 Chapter 3 Surgical Techniques ___________________________________________________________________________ After the aortic graft has been sewn in place and all bleeding spots controlled, the aneurysm sac, which has been opened along its length, is sewn back up loosely over the new graft. This prevents the new graft from rubbing against the intestine, which can damage the intestinal wall. When the graft is in place, the clamps are removed, allowing blood to flow through the graft and to the legs. Patients are usually hospitalized for seven to ten days. With the open surgery it is possible to choose among quite a large class of suitable stent, this because the surgeon always tries to find the stent that better fit for a particular patient; the last choice about the kind of stent to be used is often made at the moment of the opening of the sac. Advantage of conventional surgery compared to EVR of AAA Efficacy: elective aneurysmectomy and Dacron prosthetic engraftment is a definitive and “one-off” operation for abdominal aneurysms despite the dangers of surgery. The procedure is durable and the problems of symptomatic aneurysms are cured. Endoleaks: this problem is a specific drawback of EVR of AAA and does not occur after following conventional, open surgery. Proximal endoleaks following the endovascular approach result in expansion of the stented aneurysm sac, with eventual rupture and death of the patient Prosthesis: in the event of conventional surgery, the procedure can be easily be accomplished by use of either woven or knitted Dacron prostheses. A PTFE prosthesis is also highly suitable. Tissue incorporation and perigraft healing are far superior with the use of knitted Dacron. Wound healing and mechanical incorporation are retarded with the use of devices, as woven Dacron is used. Endoleaks simply do not occur, as back bleeding from the lumbar and the inferior mesenteric arteries are suture ligated and thus sealed. 31 Chapter 3 Surgical Techniques ___________________________________________________________________________ Prosthetic fabric: Dacron prosthesis used during open surgery has had an excellent track record. Knitted grafts have to be preclotted because of the high porosity before use. Woven fabric is less porous and is therefore the fabric of choice for stent device. Costs: although this aspect has been intensely debated, it does appear that uncomplicated surgery is cheaper than EVR of AAA in the long run. Despite reduced hospital stay and the need for intensive care facilities, EVR of AAA has the following hidden costs that must be taken into account: 1. Multiple secondary interventions will be needed in 5-10% of patients to seal persisting endoleaks 2. Expensive imaging is needed for post-stent surveillance 3. Conventional aortic prostheses used for surgical repair are less expensive than stent devices. Remodeling of the aneurysm sac: following the conventional surgery, this phenomenon has little effect on the long-term results of operation or graft patency. May et al. of the University of Sidney, Australia, and others have reported on the late changes in endograft and aneurysm morphology after stent-graft treatment. Remodeling of the aneurysm sac may contribute to prosthetic distortion following a reduction in the length of the aneurysm sac [Don F. du Toit, 1999]. This may involve changes in the shape and position of the device which could predispose to thrombosis in the endograft or endoleak formation. 32 Chapter 3 Surgical Techniques ___________________________________________________________________________ 3.3 Endovascular treatment Endovascular repair (EVR) of abdominal aortic aneurysm offers the advantage of a minimally invasive technique, a hospital stay of one to two days, a rapid return to normal physical activity, and a reduction in the mortality and complication rate when compared with the conventional surgical procedure. EVR is well tolerated by elderly patients and many are able to undergo AAA repair this way, with a reduced need for general anesthesia and blood transfusions. As EVR of AAA is still in the investigation phase, long-term results are eagerly awaited as regards the incidence of late endoleak formation. However, it is estimated that the introduction of the newer, second-generation stent devices will allow between 7080% of aneurysms to be treated this way [Don F. du Toit, 1999]. Endovascular repair of abdominal aortic aneurysm utilizes access to the vascular system, through the femoral artery(-ies). A graft of appropriate design is positioned and deployed in the abdominal aorta in order to exclude the aneurysm from the pathway of blood flow and thus eliminate the risk of rupture (fig. 3.5 and 3.6). This technique uses the same graft material, woven polyester, as that used for conventional aneurysm repair. A selfexpanding stent with hooks that engage the wall of the aorta and iliac arteries become a substitute for suture material and is called the attachment system. Fig. 3.5 The insertion of the stent with the delivery system (on the left) and an endovascular stent-graft used for AAA repair(0n the right), showing the two self-expanding Z-stents sutured to each end of the Dacron tube graft. 33 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.6 This picture shows the operative field prepared for the usage of the delivery system. In this case two accesses have been opened using both femoral arteries (it is possible to see the two guide-wires), but if the aneurysm does not involve the iliac bifurcation it is enough only one of the two accesses to deploy the stent. When the operation is completed, there is essentially the same reconstruction as would have been achieved with conventional open repair with the exception of the fact that a major abdominal incision is avoided with the substitution of one or two small incisions over each femoral artery in the groin. For patients with an abdominal aortic aneurysm that is limited to the aorta, and in whom there is both a neck between the renal arteries and the aneurysm as well as a neck between the lower portion of the aneurysm and the iliac bifurcation, a graft of tubular configuration is available (fig. 3.7 and fig. 3.8). 34 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.7 A detail of the structure of a tubular stent. Fig. 3.8 Tubular stent partially opened. The stent design shown in fig. 3.7 is just one of the available configurations, The scientists are continually looking for the best design in order to obtain an optimal adaptability of the prosthesis to the aorta, therefore different kinds of frame are available: zigzag, fishing net configuration, spiral frame etc. For those patients in whom the abdominal aneurysm extends to the iliac bifurcation, a bifurcated or Y-shaped graft is available (fig. 3.9). For those patients who have both an abdominal aortic aneurysm as well as an aneurysm of one or both iliac arteries, the third option is a tapered tube graft that excludes both the aortic aneurysm and one iliac aneurysm. 35 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.9 AneurRx® modular endovascular bifurcated prosthesis showing components (A) The entire operation is executed without any chance to observe and complete construction alignment (B). the aneurysm directly. The surgeon works for the whole time on the basis of an X-ray image, just looking at a screen. The images he can refer to are 2-D, so it is often difficult to know the exact position of the stent-graft. The only reference upon which the surgeon can count is a system of radiopaque markers on the vascular prosthesis, which are visible in the Xray image. The markers are usually three, one at the proximal part of the stent, one at the distal part and another in the middle of the prosthesis. When radio-opaque contrast solution is injected via a catheter an angiogram image is seen on the X-ray screen (fig. 3.10). 36 Chapter 3 Surgical Techniques ___________________________________________________________________________ B A C D Fig. 3.10 The four images show the screen and the images used by the surgical team during a typical operation. In fig. 3.10b and fig. 3.10c the arrows indicate the aneurysmatic parts of the aorta and it is possible to see the guide-wire that is used to insert the delivery system and to measure the length of the aneurysm. In fig. 3.10d it is clearly visible the fabric of the prosthesis after the deployment and the markers on the proximal part. In aorto-uni-iliac endografting, the contralateral iliac artery aneurysm is secondarily excluded, and blood flow to the contralateral leg and pelvic circulation is accomplished with the placement of a subcutaneous crossover graft between the two femoral arteries. The patient comes to the hospital in the morning of operation and is taken to the operating room. 37 Chapter 3 Surgical Techniques ___________________________________________________________________________ Using either general anesthesia or regional anesthesia, one or both femoral arteries are exposed depending upon the type of reconstruction that is required. A needle followed by a guide wire is then placed in the femoral artery, and the guide wire is extended up the aorta. An angiogram is obtained in order to provide a roadmap image for placement of the device. The patient is then anti-coagulated with Heparin and the femoral artery is clamped. A small transverse opening is then made in the femoral artery through which a working sheath is inserted. The sheath then provides a bloodtype roadway for placement of the graft/catheter delivery system. If a bifurcated graft is required or an aortoiliac with femoral-femoral crossover, the contralateral femoral artery is also exposed. In the case of the bifurcated graft, the contralateral femoral artery is accessed with a needle puncture followed by the placement of a sheath with a catheter that has a snare system. In the case of a tube graft, the graft catheter delivery system is passed up through the sheath, over the guide wire, and positioned across the aneurysm. Using remote release levers, the graft is deployed with the upper attachment system immediately below the renal arteries. Both prostheses, self-expandable and with a balloon (fig. 3.11), are available. In particular, the self-expandable technology is based on the use of shape memory alloys (generally Nitinol). Fig. 3.11 Balloons on top of catheters, the balloons are inflated with physiologic liquid in order to avoid air outflow in the case of rupture. 38 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.12 Some models of stents available on the market. The choice of the one to use is a matter of the experience of the surgeon; nowadays a little has been written about the best configuration for the stents and the research is in the hands of the manufactures that try to differentiate their own products (fig. 3.12). Nowadays, this kind of prostheses are made by shaping a Nitinol wire to remember what will be its final shape in the aorta, than the stent-graft is deformed to fit into the delivery system. When the prosthesis is in place, the delivery system is opened gradually and the graft is so exposed to the body temperature and due to this it recovers the shape that was previously given (fig. 3.13). Fig. 3.13 A detail of the upper part of a delivery system. After the hooks are opened by the surgeon and the hooks on the proximal part of the graft are seated into the wall of the aorta there is no chance to change the position of the prosthesis. 39 Chapter 3 Surgical Techniques ___________________________________________________________________________ In the prosthesis with balloon (fig. 3.14) the balloon is coaxial with the graft within the delivery system, it is positioned across the attachment site and inflated by the surgeon to expand the stent against the aortic wall. The lower attachment system is then deployed immediately proximal to the bifurcation of the iliac arteries. The balloon is positioned across that attachment site, and the hooks are seated at that point. Fig. 3.14 Two steps of the inflating procedure of a stent with balloon; configuration of the stent at the moment of insertion (left), inflated configuration (right). It is even possible to find prostheses that use both shape memory alloys and balloons; the latter to better adapt the stent-graft to the aortic wall in the attachment sites. A completion angiogram is then obtained to make certain that the graft is properly seated and there is no evidence of flow between the graft and the aneurysm. In the case of the bifurcated graft, initially a wire that is connected to the contralateral limb of the graft is passed up the ipsilateral side, captured with a snare, and drawn into the contralateral side. The graft/catheter delivery system is then advanced over a guidewire, and a jacket that covers the graft is retracted, thus allowing the two limbs of the graft to separate. The graft is then brought down and appropriately positioned with the proximal attachment system immediately below the renal arteries and each iliac graft limb in their appropriate ipsilateral and contralateral iliac arteries. The attachment systems are then sequentially deployed, and each attachment system is seated with inflation of a balloon catheter. Once completed, the opening of the femoral artery(-ies) is repaired. 40 Chapter 3 Surgical Techniques ___________________________________________________________________________ The femoral incision sites are closed, and the patient is returned to the recovery room for initial observation. Following that, the patient is sent to a regular hospital bed for an overnight stay. The following morning the patient is discharged from the hospital. A return visit is accomplished within the first week, when a repeat CT scan and plane abdominal films are obtained in order to make certain that the graft is functioning properly. The femoral incisions are usually well healed within one to two weeks, and the patient returns to normal physical activity. Step by step EVR procedure Here a step-by-step explanation of the implantation of a stent-graft is given. The example is based on the use of the AneuRx stent-graft, but with the exception of few details (for instance the configuration of the radiopaque markers) the procedure is absolutely general. 1. Insertion of the primary stent graft delivery catheter into the vessel, maintaining continual fluoroscopy for proper positioning above the renal arteries. Traction or a slow pull on the wire is essential to facilitate device tracking. 41 Chapter 3 Surgical Techniques ___________________________________________________________________________ 2.This kind of stent has a special cone shaped part to help the surgeon during the deployment. The catheter’s nose cone has to be placed at, or immediately above, the renal arteries. The crosshole of the nose cone should appear fully round when aligned. The top three radiopaque markers have to be positioned towards the contralateral side. 3. In this phase the graft cover is retracted 2-3 cm until it is possible to see the four proximal radiopaque markers. It is essential to watch for possible movement via fluoroscopy. 42 Chapter 3 Surgical Techniques ___________________________________________________________________________ 4. Small rotational adjustments with the delivery catheter can still be made in this phase to align the radiopaque markers. An angio check via the contralateral straight catheter should be performed in order to confirm the position of the stent graft relative to the lowest artery. After the adjustments the straight angiographic catheter has to be pulled back into the abdominal aortic aneurysm. 5. The retraction of graft cover continues until this is just below the distal radiopaque marker. This position is crucial and must be carefully checked with fluoroscopy to assure safe deployment. 43 Chapter 3 Surgical Techniques ___________________________________________________________________________ 6. Insertion of the cotralateral delivery catheter into the sheath. This phase requires good experience, actually the delivery catheter has to be inserted well into the gate area and this is an area that is perpendicular to the images’ plane (the area is seen as a line on the video). 7. The delivery catheter must be aligned within the four radiopaque markers of the pant leg in the mid- or upper portion of the gate. 44 Chapter 3 Surgical Techniques ___________________________________________________________________________ 8. The deployment of the stent graft has to be executed under continuous fluoroscopy, watching carefully for any position changes. Deployment of the iliac leg continues until the graft cover is just below the distal radiopaque marker on the iliac leg. 9. Deployment completed. Accurate and secure proximal and distal attachment must be ensured to prevent endoleak formation. 45 Chapter 3 Surgical Techniques ___________________________________________________________________________ 3.4 Drawbacks and follow up Open surgery The main drawbacks of the classic operation are the need for laparotomy, general anesthesia, a hospital stay of 7-10 days, intensive care facilities and blood transfusions. Despite the use of risk-factor determination, surgical repair of AAA is still associated with unexpected peri- and post-operative complications. Some of the reasons why the classical operation of resection and prosthetic engraftment are associated with a significant morbidity in high-risk patients include the following: Aortic aneurysmectomy is a major surgical intervention requiring extensive retroperitoneal dissection Blood loss may be significant during the procedure Access is needed through a full-length laparotomy incision extending from the xiphisternum to the pubis. This predisposes to important fluid losses and hypothermia during the procedure Clamping and declamping of the aneurysm neck result in hypo tension associated with major haemodynamic disturbances Respiratory problems associated with general anesthesia and major surgery. The results of conventional surgical repair of AAA are durable and the danger of rupture is eliminated, these aspects are fundamental to understand why this kind of operation is still performed and is often preferred to the endovascular procedure. Moreover EVR of AAA is currently still considered an investigational technique under validation worldwide and results of long-term studies and outcome are slowly becoming available. 46 Chapter 3 Surgical Techniques ___________________________________________________________________________ EVR The Achilles heel of EVR is the development of procedural, peri-procedural or late endoleaks and endotension (when aneurysms grow even in absence of any detectable endoleak) due to anatomical factors. An endoleak refers to incomplete sealing of the stent allowing back bleeding into the paraprosthetic space. The incidence varies from 7-10% in major series, unfortunately the need for additional interventions to seal the leaks increases the cost \ benefit ratio of EVR of AAA [Don F. du Toit, 1999]. Before analyzing these important drawbacks of the endovascular procedure, it is useful to distinguish four different types of endoleak. Endoleak Type I: flow between the stent-graft and the wall of the aneurysm related to the graft device itself (fig. 3.13). Endoleak Type II: retrograde flow from collateral branches, this leak appears to have a greater tendency to seal by spontaneous thrombus (fig. 3.14). Endoleak Type III: due to fabric tears, graft disconnection or disintegration (fig.3.15). Endoleak Type IV: flow through the graft presumed to be associated with graft wall “permeability\porosity” (fig. 3.16). Type Ia Blind end to end Type Ib With drainage Fig. 3.13 Perigraft-leaks 47 Chapter 3 Surgical Techniques ___________________________________________________________________________ Type IIa Type IIb Blind end to end With drainage Fig. 3.14 Collateral leaks Type III Fig. 3.15 Mid-graft leak Type IV Fig. 3.16 Graft-porosity leak Endoleaks The definition of initial technical success with endovascular techniques in the management of aneurysms includes complete exclusion of the sac, reduction of intraaneurysm pressure, restoration of normal blood flow and prevention of rupture. The 48 Chapter 3 Surgical Techniques ___________________________________________________________________________ fixation points at the ends of a stent-graft must be in complete apposition with the normal vessel wall without thrombus interposition to achieve these goals. If this is not achieved, sealing at the fixation points will be incomplete or temporary [J. C. Parodi et al., 2001]. Endoleaks have been reported in 7% to 37% of endovascular aortic aneurysm repair [B. Marty et al., 1998]. An endoleak involves the failure of complete exclusion of the aneurysm with the persistence of elevate pressures within the aneurysm sac. The flow due to an endoleak may be caused by an incomplete seal at the graft ends or, between segments, by thrombus interposition, by incomplete deployment, or by inappropriate sizing. Finally, endoleaks that are not graft related may be seen with retrograde flow from patent lumbar or inferior mesenteric arteries. The presence of endoleaks without enlargement and, conversely, enlargement without demonstrable endoleaks allow us to justify the concept of aneurysm sac pressurization as a real cause of enlargement, ultimately leading to aneurysm rupture [J. C. Parodi et al., 2001]. Two factors produce pressurization inside the sac: 1. pressure inside the endograft that is transmitted by pulsation inside a semi- rigid container (the aneurysm sac); 2. the intra-abdominal pressure. The presence of an endoleak causes a significant increase in aneurysm pressure (mean pressure and diastolic pressure), the extent of which is directly proportional to the endoleak size, even a small size endoleak causes considerable pressure in the sac, which in the clinical settings could lead to aneurysm rupture. La Place’s law dictates that the wall stress of an artery is proportional to the radius and intraluminal pressure and inversely proportional to wall thickness. This concept predicts that increasing blood pressure or sac diameter should increase wall tension and also the risk of rupture. 49 Chapter 3 Surgical Techniques ___________________________________________________________________________ Endoleaks are usually situated at the proximal stent attachment site and produce a small perigraft channel with outflow through a partially thrombosed aneurysm sac [J. C. Parodi et al., 2001]. The pressure in the thrombus remains low, but at the distal end, the pressure level suddenly increases up to systemic level and pulsatility immediately. The addition of extra human fibrinogen into the aneurysm sac prohibits the formation of thrombus inside the aneurysm. An open endoleak produces a mean pressure inside the aneurysm identical to that in the systemic circulation. This level of aneurysm pressure is independent of the size of the endoleak. As soon as the endoleak thromboses, the mean aneurysm pressure declines to zero. The belief that large endoleaks are more dangerous than small ones might be explained not by the higher pressure but by the presence of pulsatile pressure [G. W. H. Schurink et al., 2000]. In conclusion, an open endoleak results in systemic mean pressure inside the sac. If the aneurysm is not thrombosed, pulse pressure is present within the sac, but the magnitude depends on the diameter of the endoleak. Pulse pressure is absent within the sac when it is completely or partially thrombosed. A thrombosed endoleak (endoleak in presence of thrombus that occludes the bleeding) results in a decrease in mean pressure and the absence of pulse pressure in the sac. The pressure decrease is more evident for small endoleaks. Successful embolization of an endoleak by Histoacryl glue or Gelfoam reduces the mean pressure in the sac and may be a useful therapeutic option when there is progressive aneurysm growth [G. W. H. Schurink et al., 2000]. Endotension Endotension has been recently described and defined as a persistent or recurrent pressurization of the aneurysm sac after endovascular repair. Transmission of pressure through thrombus or artheroma at the proximal attachment site is a possible mechanism of endotension. 50 Chapter 3 Surgical Techniques ___________________________________________________________________________ It has been proposed that endotension may account for cases of aneurysm rupture in the absence of endoleak and that aneurysms that enlarge or fail to decrease in size may remain pressurized [C. S. Skillern et al., 2002]. Although the concept of endotension seems logical, it has not yet been shown experimentally. The mechanism for the endotension appears to be the transmission of aortic pressure to the aneurysm sac through the attachment site failure. The presence of endotension within the aneurysm sac after endovascular AAA repair may signify treatment failure and risk of aneurysm rupture. Rupture may not lead to catastrophic haemorrhage if the proximal and distal stent graft attachment sites remain secure. However, endotension may also be the result of a sealed Type I endoleak, and rupture could have disastrous consequences in that situation. Pressure transmission may be related to porous graft fabrics. Also, graft materials have previously been responsible for the local production of serous fluid by transudation through a polytetrafluoroethylene (PTFE) graft used at open AAA repair. The mechanism for aneurysm enlargement remains unclear, but it is postulated to be due to pressure transmission through thrombus after endoleak thrombosis [C. S. Skillern et al., 2002]. Anatomical factors Because of peculiar aneurysm anatomy detected in 70-80% of cases [Don F. du Toit, 1999], not all aneurysms can be safely treated by the elective endovascular route. Moreover, the requirement to customize the device to specific aneurysm dimensions precludes the use of current devices to large extent in the urgent or emergency situation. In order to obtain a leak-free attachment, besides a correct sizing of the prosthesis, it is important to ensure a secure anchorage; two are the critical landing zones: the proximal and the distal necks. In fig. 3.17 and 3.18 the different geometrical limitations are shown [Don F. du Toit, 1999]. 51 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.17 Neck region. (A): Renal ostia originating at different levels. (B): Aneurysmal dilatation at the neck wit suprarenal extension. (C): Short conical neck. (D): Short neck. (E): Reverse conical neck. (F): Aberrant renal arteries. (G): Angulated neck and aberrant arteries. (H): Concomitant renal artery stenosis. (I): Juxtarenal aneurysm formation. (J): Juxtarenal thrombus formation. (K, L, M, N, O, P): Degree of angulations. (Q): Large aneurysm with intramural thrombus. (R): Posterior plaque. (S): Ulceration. (T): Thrombus. 52 Chapter 3 Surgical Techniques ___________________________________________________________________________ Fig. 3.18 Distal region. (A): Stenosis. (B): Hypoplastic segment. (C): Ipsilateral occlusion. (D): Intraluminal thrombus, tortuosity. (E): Bilateral angulations. (F): Thrombus. (G): Unilateral iliac ectasia. (H): Unilateral stenosis, contralateral estasia. (I): Bilateral common iliac aneurysms. (J): Aorto-iliac stenosis and angulations. (K): Hypogastric artery occlusions and stenosis. (L): Unilateral short iliac segment and contralateral angulations. (M): Concomitant iliac aneurysms. (N) : Common iliac aneurysm and contralateral angulations. (O): Isolated internal iliac artery aneurysm. (P): Catheter perforation of iliac vessel during intubation. 53