FAQ - why-iba | Proton Therapy
advertisement
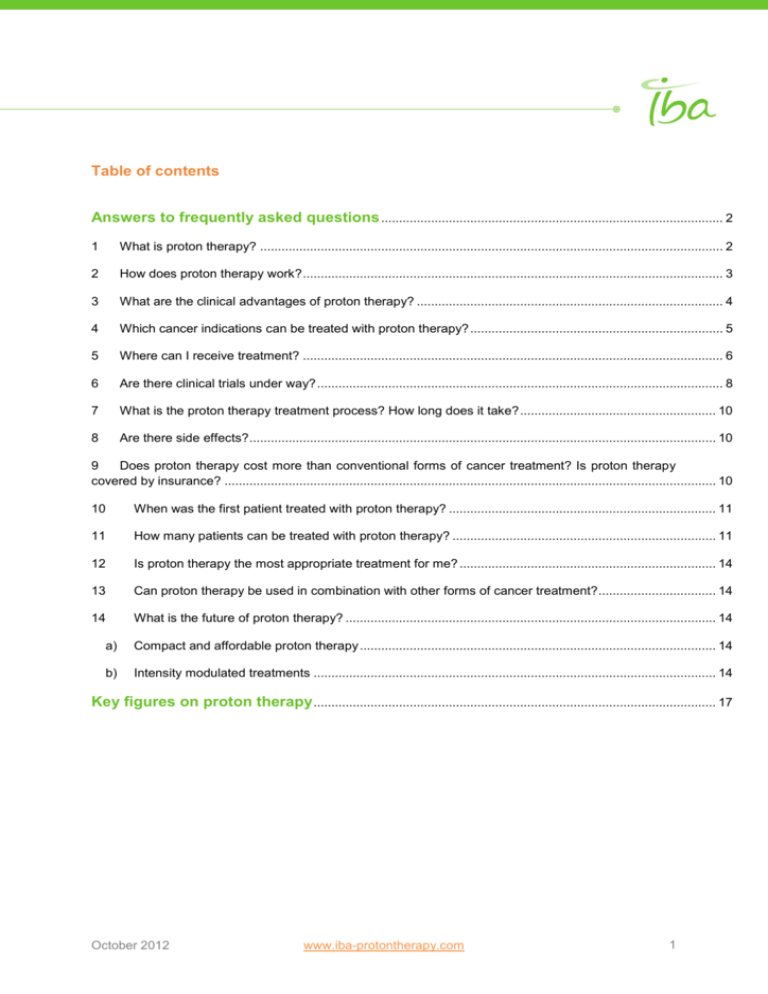
Table of contents Answers to frequently asked questions ................................................................................................ 2 1 What is proton therapy? .................................................................................................................................. 2 2 How does proton therapy work? ...................................................................................................................... 3 3 What are the clinical advantages of proton therapy? ...................................................................................... 4 4 Which cancer indications can be treated with proton therapy? ....................................................................... 5 5 Where can I receive treatment? ...................................................................................................................... 6 6 Are there clinical trials under way? .................................................................................................................. 8 7 What is the proton therapy treatment process? How long does it take? ....................................................... 10 8 Are there side effects? ................................................................................................................................... 10 9 Does proton therapy cost more than conventional forms of cancer treatment? Is proton therapy covered by insurance? .......................................................................................................................................... 10 10 When was the first patient treated with proton therapy? ........................................................................... 11 11 How many patients can be treated with proton therapy? .......................................................................... 11 12 Is proton therapy the most appropriate treatment for me? ........................................................................ 14 13 Can proton therapy be used in combination with other forms of cancer treatment? ................................. 14 14 What is the future of proton therapy? ........................................................................................................ 14 a) Compact and affordable proton therapy .................................................................................................... 14 b) Intensity modulated treatments ................................................................................................................. 14 Key figures on proton therapy ................................................................................................................. 17 October 2012 www.iba-protontherapy.com 1 ANSWERS TO FREQUENTLY ASKED QUESTIONS 1. What is proton therapy? Proton therapy is an advanced form of radiotherapy that uses a high-energy proton beam for cancer treatment. These protons damage the DNA of cancer cells, ultimately inducing cell death. Cancerous cells are particularly vulnerable to such attacks. While conventional X-ray radiation can damage healthy tissues, proton beams deliver their maximum energy within a precisely controlled range, known as the Bragg peak, thereby reducing adverse effects to adjacent healthy tissues. There is virtually no energy deposition past the Bragg peak as the proton has delivered all its energy to the tumor. X-ray radiation releases much of its energy quickly after penetrating the skin, disrupting the cells of healthy tissues and organs. The unnecessary dose of Xrays (photons) is shown in purple. The Bragg peak can be precisely calculated as a function of the beam’s initial energy. Proton beams release the majority of their destructive energy within a small range inside the tumor, depositing lower entrance dose and no exit dose. This unique characteristic of the proton beam enables it to treat tumors with unequaled precision, safety and efficiency. Proton therapy advantages include: • precise delivery of an optimal radiation dose to the tumor; • safely escalating the dose within the tumor, with minimal exit dose; • reducing the probability and/or severity of side effects on healthy surrounding tissues; • an increase of long-term, progression-free survival rates for certain types of tumors. October 2012 www.iba-protontherapy.com 2 2. How does proton therapy work? Proton therapy uses the protons from hydrogen atoms that remain after the electrons are removed. In proton therapy centers equipped by IBA, the cyclotron accelerates protons to an extremely high speed, generating a controlled beam. The IBA Energy Selection System (ESS) makes it possible to transform the fixed energy generated by the cyclotron into the exact energy needed for a particular treatment. This proton beam travels through a beam transport system to individual treatment rooms. The beam is then delivered through a nozzle to the targeted tumor. As each proton enters the body, there is a low dose of radiation released at the surface, followed by a sharp burst released as the proton hits its target. The proton beam can be contoured to the shape of the tumor, further decreasing the exposure of healthy cells to radiation and limiting side effects. The IBA isochronous cyclotron is today the simplest and most effective way to produce 230 MeV protons. A. October 2012 www.iba-protontherapy.com 3 3. What are the clinical advantages of proton therapy? Proton therapy offers the same tumor-killing properties as traditional radiation treatment, but with decreased side effects and complications. The difference in the effectiveness of proton therapy versus radiation treatment is determined by what takes place before and after the radiation reaches the tumor. Radiation releases much of its energy quickly after penetrating the skin, disrupting the molecules of healthy tissues and organs. Proton therapy allows most of its energy to be released only when it reaches the tumor. And unlike radiation, which passes completely through the body, protons do not go further than the tumor thus sparing surrounding healthy tissues. Key advantages of the proton beam in cancer treatment: • high-energy radiation doses delivered directly to the tumor; • little or no radiation beyond the tumor; • compassionate cancer treatment with fewer side effects on surrounding healthy tissues and vital organs, hence allowing a better quality of life during and after treatment. October 2012 www.iba-protontherapy.com 4 4. Which cancer indications can be treated with proton therapy? Proton therapy is used today to treat many cancers and is particularly appropriate in situations where treatment options are limited and conventional radiotherapy presents unacceptable risks to patients. Because proton therapy targets tumors better than traditional treatments, it is ideal for the treatment of tumors that are located near a vital organ. These situations include eye or brain cancers, tumors close to the brain stem or spinal cord, head and neck cancers, prostate cancers, and pediatric cancers. Recent phase II studies have also shown the key impact proton therapy can have on lung tumors, a medical condition that is today poorly treated with conventional radiation therapy. October 2012 www.iba-protontherapy.com 5 5. Where can I receive treatment? IBA has designed and installed the majority of clinically operating proton therapy centers in the world. Today, numerous reference centers all over the world are treating patients with IBA equipment. [Link to document Proton Therapy Facilities list of the Press Kit] The National Association for Proton Therapy displays the map of existing proton therapy centers on the following link: http://www.proton-therapy.org/map.htm October 2012 www.iba-protontherapy.com 6 Number of proton therapy centers worldwide: Source: PTCOG, Press Releases of manufacturers. October 2012 www.iba-protontherapy.com 7 6. Are there clinical trials under way? Over the years it has become increasingly clear that the strength of proton therapy lies in the reduced side effects of the superior dose deposition efficiency (i.e. the Bragg peak). Protons have a significant advantage over more traditional therapies when the tumor lies adjacent to an organ at risk. This is not so much because of the better penumbra with respect to high energy X-rays but due to the reduced dose that protons deliver outside the target volume. In addition, when the target volume is wrapped around a sensitive organ, proton will offer the best treatment. Due to the sharp distal fall-off (protons have a finite range), the dose distribution can be shaped to create complexly shaped dose distributions. At the Francis H. Burr Proton Therapy Center, linked to Massachusetts General Hospital in Boston (USA), the medical staff can rely on almost 40 years of proton therapy practice at the Harvard Cyclotron Laboratory. The equipment designed and installed by IBA started treating patients in November 2001. To date more than 5600 patients have received proton treatment there. Table 1 gives a list of conditions which can be treated at the Francis H. Burr Proton Therapy Center. Table 1: Proton beams at the Francis H. Burr Proton Therapy Center that will be used for the following treatment sites: (* Sites already treated at Harvard Cyclotron Laboratory) Chordoma and chondrosarcoma* Craniopharyngioma* Meningioma* Thoracic and lumbar spine tumors* Pediatric tumors* Prostate tumors* Choroidal melanoma* Retinoblastoma* Age related Macular Degeneration* Malignant tumors of the orbit* Arteriovenous malformations (AVMs)* Pituitary tumors* Paranasal sinus* Nasopharynx Carcinoma of the rectum Medulloblastoma Non small cell lung cancer (NSCLC) Hepatocellular carcinoma Pediatric soft tissue sarcomas Good long-term follow-up data is available for several clinical sites. Five-year survival rates for chordomas and chondrosarcomas of the base of the skull are approximately twice as high with proton therapy compared to conventional X-rays. Good results are obtained for choroidal melanomas (tumors of the eye), which are often treated by surgically removing the eye. Protons have also been shown to be very effective in the treatment of arteriovenous malformations, prostate and paranasal sinus. October 2012 www.iba-protontherapy.com 8 Clinical trials for several treatment sites are in progress at different centers in the world, and cover multiple indications, as can be seen below: Hodgkins Lymphoma 1% CNS 2% Clinical Trials Repartition AVM 2% Spine Cervix Bladder 1% 1% 1% Colorectal 2% Eye 3% Nasopharynx/Sinus 4% Head & Neck 20% Sarcomas 5% Liver 6% Prostate 12% Others/General 7% Lung 11% Pancreas 7% Breast 7% Pediatrics 8% Source: ClinicalTrials.gov - Over a total of 110 clinical trials - Accessed on May 2nd 2012 The clinical benefits of proton therapy over conventional radiation therapy can be summarized as follows. Increased tumor control, due to the ability of depositing a higher dose in the targeted volume. Reduced occurrence of treatment-related side effects due to the precision of the dose delivery and the resulting limited amount of radiation delivered to healthy tissues adjacent to the treatment volume. Increased long-term disease free survival rates for many types of tumors, due to the superior local tumor control rate in proton therapy. Several articles have been published and an extensive list of clinical references can be provided upon request. Moreover, OncoLink offers a free, confidential, personalized service that quickly searches for clinical trials that match specific cancer diagnosis and treatment history: http://www.oncolink.org/treatment/trials.cfm October 2012 www.iba-protontherapy.com 9 7. What is the proton therapy treatment process? How long does it take? Radiation oncologists use advanced imaging techniques to determine the exact location of the tumor to be treated. Proton therapy sessions may take anywhere from one day to several weeks. Over time, practitioners will be able to deliver heavier doses thereby decreasing the length of treatment. Because treatments are noninvasive, patients are able to continue with their daily activities. The actual proton beam time is about one to two minutes, but total treatment time may last up to an hour, due to the time spent positioning the patient. 8. Are there side effects? Depending on the patient’s age, medical history and condition, he or she may experience minor side effects such as fatigue, skin irritation, or slight hair loss. 9. Does proton therapy cost more than conventional forms of cancer treatment? Is proton therapy covered by insurance? Given the advanced technologies of proton therapy, the reimbursement rate has been planned accordingly. Some countries plan reimbursement on a given number of indications (usually Uveal Mellanoma Pediatric Cancers, Head and Neck, Non Small Cell Lung Cancer and Hepatocellular Carcinoma) while others plan reimbursement of proton therapy with a general rate (as is the case, for example, in the United States where MediCare reimburses proton therapy at around 1100$ per fraction and makes the distinction between “simple” and “complex” cases). Source: Various government agencies, IBA internal. October 2012 www.iba-protontherapy.com 10 10. When was the first patient treated with proton therapy? In 1946 Robert Wilson proposed that proton beams would provide superior dose distributions and should be considered for clinical radiation treatment. First tests were directed at intracranial targets and used single fractionation. The first treatments using proton or helium ion beams were carried out at the University of California in Berkeley, USA (1955), University of Uppsala, Sweden (1957), Massachusetts General Hospital, USA (1961), Physics Research Institute, Dubna, Russia (1964) and the Institute for Experimental and Theoretical Physics, Moscow, Russia (1969). Today about 39 clinical proton treatment centers are established worldwide, while approximately 25 research centers have some proton therapy related activities. The Particle Therapy Cooperative Group (PTCOG)1 is collecting valuable information about the total number of patients receiving particle therapy, i.e. protons and heavy ions. According to the most recent information, more than 100,000 patients have received treatment by particle therapy. 11. How many patients can be treated with proton therapy? As proton therapy is an emerging technology, a difference can be made between Essential Indications for which this technique is today the standard of care and Potential Indications, for which proton therapy has been demonstrated superior in treatment planning terms and over a smaller cohort of patients, and for which clinical studies are currently ongoing. As reported in the UK National Radiotherapy Advisory Group 2, Essential Indications for proton therapy can be found for pediatric cancers and head & neck chordomas, and amount to 31.5 patients / million inhabitants. In a city of 7 million inhabitants, this would equate to 220 patients treated per year, or one treatment room. As reported in the Dutch Gezondheidsraad report on Proton Therapy 3, Potential Indications would amount to 411 patients / million inhabitants, equating to about 2880 patients a year in a city of 7 million inhabitants, which would necessitate around 10 treatment rooms. Furthermore, with future developing technologies (such as Intensity Modulated Proton Therapy (IMPT) or different uses of these particles such as mild hypo-fractionation), both the effectiveness and the cost per treatment will decrease, indicating that proton therapy could be used for up to 30% of radiation therapy patients, which would mean in excess of 900 patients/million inhabitants. Today, the total number of treatment rooms ordered worldwide amounts to more than 160 with approximately 96,000 patients treated in all facilities, as illustrated in the tables below. 1 Particle Therapy Cooperative Group (PTCOG), http://ptcog.web.psi.ch/. 2 http://www.cancer.nhs.uk/documents/nrag_files/proton%20subgroup%20report%20-%20fin.pdf 3 http://www.gezondheidsraad.nl/sites/default/files/proton%20radiotherapy200917E_0.pdf October 2012 www.iba-protontherapy.com 11 Number of treatment rooms ordered - Number of patients treated per year: Source: PTCOG and various company websites. October 2012 www.iba-protontherapy.com 12 Patient Statistics (for the facilities in operation end of 2011): Source: “Hadron Therapy Patient Statistics (data received per March 2012)”, Martin Jermann, March 2012, Particle Therapy Cooperative Group (PTCOG) Secretary, http://ptcog.web.psi.ch/patient_statistics.html, visited on May 2012. October 2012 www.iba-protontherapy.com 13 12. Is proton therapy the most appropriate treatment for me? This question must be answered by your doctor. He is the one who can identify the most appropriate treatment based on the cancer diagnosis. Further information on this subject is provided by international organizations such as oncolink.com. Patients are encouraged to read as much as possible about treatment options and discuss the question thoroughly with their doctor. 13. Can proton therapy be used in combination with other forms of cancer treatment? Yes, in multiple cases proton therapy can be used in conjunction with other forms of treatment. Depending on the situation, proton therapy may be used in combination with traditional radiation, chemotherapy and/or as a follow-up to surgery. 14. What is the future of proton therapy? A. Compact and affordable proton therapy Although the first discoveries about the use of the proton beams in cancer treatment date from 1946, it was only in 1990 that the world's first hospital-based proton therapy center was built. Since then, IBA has installed 12 proton therapy centers worldwide and 10 more are in various stages of development. Today, the number of proton therapy facilities worldwide is still relatively limited. Existing proton therapy facilities therefore attract patients from around the world, in addition to treating patients from their region. While the potential number of patients that could benefit from proton therapy is large, the heavy investment required for this technology has limited access up until now. This is the reason why IBA is dedicated to making proton therapy more available to patients, as well as more affordable to healthcare systems. For example, IBA is currently designing ProteusONE 4 , a smaller, more affordable proton therapy system. This new single-room system substantially reduces the cost, space and installation time required to build a proton therapy center. The first ProteusONE solution installed by IBA will be at a proton facility being developed by Willis-Knighton Cancer Center in Shreveport, Louisiana. IBA is committed to making proton therapy the most precise cancer treatment available worldwide. B. Intensity modulated treatments Technological advances in conventional external beam radiotherapy have led to a new approach of Intensity Modulated Radiation Therapy (IMRT). While IMRT is certainly a large improvement over conventional radiotherapy and given the fact that some medical professionals may estimate that photon IMRT and its recent developments make proton therapy redundant, we need to evaluate some of the physics aspects. While IMRT may come close to the dose distribution achieved in passive scattering methods with protons, a recent comparative study between IMRT and Intensity Modulated Proton Therapy (IMPT) shows the advantage of protons in terms of its reduced dose burden outside the target volume. Looking at the treatment plans for the different approaches, as shown in Figure 1 below, it takes 9 photon fields to construct a highly conformal dose distribution with good sparing of the brain stem for the treatment of a nasopharyngeal tumor. The availability of large degrees of freedom in the beam delivery and the strength of the mathematical methods make it possible to produce very satisfying dose distributions, shaped in all 3 dimensions to conform precisely to the target volume. 4 Subject to review by Competent Authorities (FDA, European Notified Bodies, et al.) before being put on the market. October 2012 www.iba-protontherapy.com 14 Figure 1: An example of intensity modulated treatment planning with photons. Through the addition of 9 fields it is possible to construct a highly conformal dose distribution with good dose sparing in the region of the brain stem Protons are charged particles and narrow beams can be magnetically scanned onto any target volume. In Figure 2, using the same patient as in 1, a very high degree of conformity with target volume is shown using only four dose fields with protons. Figure 2: Example of intensity modulated proton therapy (IMPT). A high degree of conformity is achieved using a low number of dose fields. The advantage compared with photons is the general reduction of dose burden outside of the target volume. Another important comparison point is the integral dose delivered during the course of the treatments in the different treatment modalities. While IMRT may come close in target conformity to standard methods of delivering proton therapy, the total dose delivered in the treatments is substantially higher. The possibility of also delivering proton in an intensity modulated treatment will allow a small reduction of the integral dose while increasing substantially conformity to the target volume. Figure 3, illustrating these principles was presented by Dr. J. Loeffler from the NPTC at the ASTRO conference in 2001. October 2012 www.iba-protontherapy.com 15 Conformity IMPT 3D PT IMXT 3D-XRT LOW Integral Dose HIGH Figure 3: Illustration of the expected integral dose versus tumor conformity in the different treatment modalities. October 2012 www.iba-protontherapy.com 16 KEY FIGURES ON PROTON THERAPY5 5 • Cancer is a leading cause of death worldwide. • There are more than 100 types of cancers; any part of the body can be affected. • In 2008, 7.6 million people died of cancer, representing 13% of all deaths worldwide. • By 2020, 1/3 of the population will be affected by cancer. • In 2020, 19 million patients will be newly diagnosed with cancer every year. • Today, we have identified 3 ways to fight cancer: chemotherapy, surgery and radiation therapy. Depending on the cancer diagnosis, doctors identify the most appropriate treatment. • Proton therapy is an advanced form of radiation therapy that uses a micro-precision proton beam for cancer treatment. While conventional X-ray radiation can damage healthy tissues, proton therapy delivers the beam very precisely, thereby treating without harming healthy surrounding tissues. With proton therapy, there is significant potential to reduce side effects, improve overall outcomes in cancer treatment and improve the quality of life for patients. Depending on the case, proton therapy can be used stand-alone or in combination with traditional radiation, chemotherapy and/or as a follow-up to surgery. • With the use of proton therapy, 10-year cure rates for patients with tumors at the base of their skulls have increased from 35 percent to 75 percent. • The overall disease-free survival rate of patients with prostate cancer who received proton therapy has reached 89 percent. And patients are experiencing fewer side effects than with traditional treatments. • Thanks to its precise dose distribution, proton therapy reduces the severity of radiotherapy late effects, which is extremely beneficial in the treatment of children. • In the case of pediatric tumors, conventional radiation has a major effect on growth and IQ development, and can produce side effects such as undesired lung diseases. With proton therapy, the risk of growth abnormality is reduced from 100% to 20%. • It is estimated that more than 50% of cancer patients will receive radiation therapies during the course of their treatment. • Today, the key indications for PT represent up to 30% of all cancers treated in conventional radiation therapy. • This corresponds to more than 700.000 potential patients per year for proton therapy. • When it comes to treatment options, patients naturally seek the best possible cancer treatment. • However, to date less than 1% of them have benefited from proton therapy given the limited number of centers equipped with appropriate equipment. • Today, the potential of patients being treated with proton therapy is huge, however the access is limited. This is why IBA is dedicated to making proton therapy more available to patients, as well as more affordable to healthcare systems. • IBA has designed and installed the majority of clinically operating proton therapy centers in the world with 12 proton therapy centers treating patients and 11 more in various stages of development. • Benefiting from more than 25 years of experience, IBA is developing proton therapy systems that are smaller, more affordable, easier to install and easier to operate. Sources : World Health Organization, http://www.who.int/cancer/en/index.html, visited on May 2012. OncoLink, http://www.oncolink.org/treatment/article.cfm?id=322&s=27&c=5, visited on April 2012. Particle Therapy Cooperative Group (PTCOG), http://ptcog.web.psi.ch/, visited on April 2012. October 2012 www.iba-protontherapy.com 17 • With IBA, protons are possible for more patients worldwide. October 2012 www.iba-protontherapy.com 18