Vascular Access - ESRD Network of Texas
advertisement
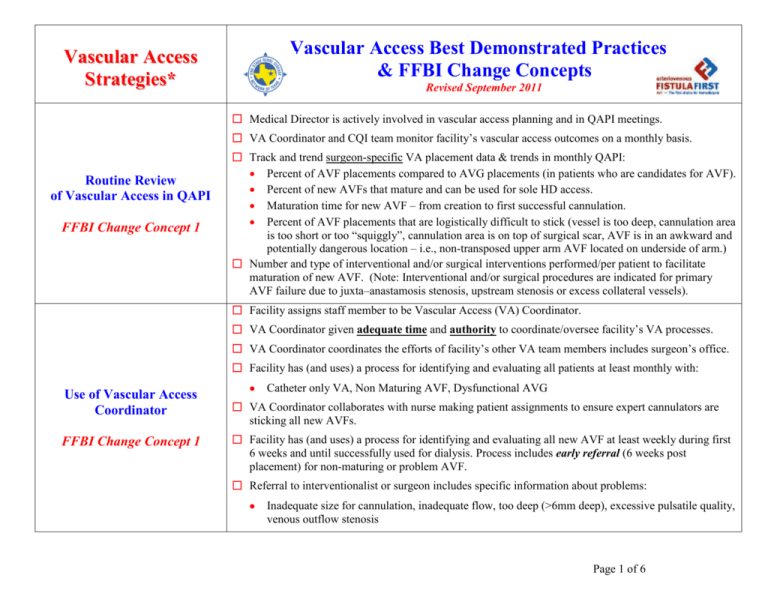
Vascular Access Best Demonstrated Practices & FFBI Change Concepts Vascular Access Strategies* Revised September 2011 Medical Director is actively involved in vascular access planning and in QAPI meetings. VA Coordinator and CQI team monitor facility’s vascular access outcomes on a monthly basis. Routine Review of Vascular Access in QAPI FFBI Change Concept 1 Track and trend surgeon-specific VA placement data & trends in monthly QAPI: Percent of AVF placements compared to AVG placements (in patients who are candidates for AVF). Percent of new AVFs that mature and can be used for sole HD access. Maturation time for new AVF – from creation to first successful cannulation. Percent of AVF placements that are logistically difficult to stick (vessel is too deep, cannulation area is too short or too “squiggly”, cannulation area is on top of surgical scar, AVF is in an awkward and potentially dangerous location – i.e., non-transposed upper arm AVF located on underside of arm.) Number and type of interventional and/or surgical interventions performed/per patient to facilitate maturation of new AVF. (Note: Interventional and/or surgical procedures are indicated for primary AVF failure due to juxta–anastamosis stenosis, upstream stenosis or excess collateral vessels). Facility assigns staff member to be Vascular Access (VA) Coordinator. VA Coordinator given adequate time and authority to coordinate/oversee facility’s VA processes. VA Coordinator coordinates the efforts of facility’s other VA team members includes surgeon’s office. Facility has (and uses) a process for identifying and evaluating all patients at least monthly with: Use of Vascular Access Coordinator FFBI Change Concept 1 Catheter only VA, Non Maturing AVF, Dysfunctional AVG VA Coordinator collaborates with nurse making patient assignments to ensure expert cannulators are sticking all new AVFs. Facility has (and uses) a process for identifying and evaluating all new AVF at least weekly during first 6 weeks and until successfully used for dialysis. Process includes early referral (6 weeks post placement) for non-maturing or problem AVF. Referral to interventionalist or surgeon includes specific information about problems: Inadequate size for cannulation, inadequate flow, too deep (>6mm deep), excessive pulsatile quality, venous outflow stenosis Page 1 of 6 Timely Referral to Nephrologist FFBI Change Concept 2 PCPs utilize ESRD/CKD referral criteria to ensure timely referral of patients to nephrologists. Establish meaningful criteria for PCPs who may not perform GFR or creatinine clearance testing. Nephrologist documents AVF plan for all patients expected to require renal replacement therapy. Designated nephrology staff person educates patient and family to protect vessels, when possible using bracelet as reminder. Nephrologist, VA Coordinator, QAPI team and other members of the facility’s VA team develop and document AVF plan for all potentially eligible patients. Early Referral to Surgeon for: “AVF Only” Evaluation Facility’s VA team and nephrologists work together to ensure that VA physical exam and vessel mapping (using duplex ultrasound) are performed before patient is referred for access surgery. Timely Placement FFBI Change Concept 3 VA surgical referrals for eligible patients state in writing that the preferred access is an “AVF Only”; the Surgeon is asked to notify Nephrologist before placing any other access type. Referral to surgeon/radiologist for VA evaluation includes written vascular access history. Surgeon Selection Based on: Best outcomes Willingness Ability to provide access services FFBI Change Concept 4 Nephrologist collaborates with facility’s Coordinator and QAPI team to evaluate surgeon selection based on willingness to place AVFs and ability to consistently create functional fistula. Patients eligible for AVF placement are referred only to surgeons able to create functional fistulas. Facility VA team and/or Nephrologist communicate preferred vascular access to surgeon. Surgeon provides post-operative access diagram that shows location of access and blood flow direction. Nephrologist refers to surgeons willing to receive/track data on their VA rates and outcomes. Nephrologist refers patients with failing AVG to surgeons skilled in placing secondary AVF’s. Facility trends new AVF patency rates for all of their surgeons. Full Range of Appropriate Surgical Approaches for AVF Evaluation & Placement FFBI Change Concept 5 Facility VA team and Nephrologist collaborate to refer patients for duplex ultrasound vessel mapping (if not already performed) to assist surgeon in determining optimal access type and access location. Ask facility’s surgeons if they have a copy of Surgeon DVD, Placing AVF in All Eligible HD Patients. If “no” – order copies from ESRD Network #14 and ask Nephrologist to give them to surgeons. Encourage acute nursing staff to become more assertive in asking Nephrologists to order vein mapping: Before dismissing new ESRD HD patients who are being dialyzed with a “catheter only”. For inpatient CKD patients who are expected to progress rapidly toward ESRD (i.e., Stage 4 CKD). Refer to catheters as temporary or short-term or bridge access – not as permanent access. Page 2 of 6 Secondary AVF Placement in Patients With AV Grafts FFBI Change Concept 6 In collaboration with nephrologist, examine upper arm veins on forearm AVG patients at least monthly for outflow vein(s) that could be converted to secondary upper arm AVF (“Sleeves Up” protocol): Refer patients with failing AVG for vessel mapping to identify arteries/veins for future access sites. Inform nephrologist and surgeon of findings and collaboratively develop new VA plan for patient. If patient is eligible for AVG conversion to secondary AVF, schedule surgery before AVG clots. Protocol at www.esrdnetwork.org Fistula First Dialysis Staff Resources VA Procedures Complete/review “Checklist of Indications for Hemodialysis Catheter Use” monthly for all catheter patients. To facilitate early catheter removal, develop and implement QI process for tracking catheter patients. AVF Placement in Patients With Catheters (Where Indicated) FFBI Change Concept 7 VA Coordinator and VA team are assertive about catheter removal and permanent access placement. Within the first (3) treatments following admission, Nephrologist, VA Coordinator and Nurse Manager talk to new dialysis patients with “catheter only” about catheter access: Make it clear that even though their catheter is called a “perm-cath”, it is not a permanent access. Discuss need for permanent access placement. Ask about scheduled VA assessment appointments (i.e., vessel mapping, referral to surgeon, etc.). Staff taught to refer to catheters as temporary or short-term access – not as permanent access. Catheter patients with maturing access taught catheter is bridge access to be used only until access matures. Facility’s best, most skilled cannulators are assigned to teach other facility staff how to cannulate AVFs. Categorize staff according to cannulation skills and experience using Staff Skills Checklist. AVF Cannulation Training & Cannulation of a New AVF FFBI Change Concept 8 Only the most skilled staff are assigned to cannulate patients with a new or difficult AVF. Assign same staff member (best cannulator) to cannulate patient with new AVF for entire first month. Use R e c o m m e n d e d P r o c e d u r e f o r C a n n u l a t i o n o f a N e w A r t e r i o v e n o u s F i s t ul a (or a similar break-in procedure) during the first 2-4 weeks a new AVF is being cannulated to minimize VA complications. Procedure should include use of smaller gauge needles and slower blood pump speeds with advancing needle gauge and pump speed, as tolerated and according to procedure. For patients with functioning catheter and a new AVF, follow this cannulation protocol: Cannulate only arterial needle for 3 consecutive treatments (to prevent large venous return infiltration). If no VA complications during above 3 treatments, cannulate both arterial and venous needles. If cannulation is complication-free for 2 weeks – arrange to have catheter removed. Page 3 of 6 Monitoring & Maintenance to Ensure Adequate Vascular Access Function FFBI Change Concept 9 Education for Caregivers FFBI Change Concept 10 Patient Education FFBI Change Concept 10 New AVFs that do not show signs of maturing (primary AVF failure) at 4 weeks post-op are referred to surgeon or radiologist for assessment and, if indicated, surgical/radiological intervention. New AVFs assessed monthly for maturation and suitability for cannulation; assessment is documented and reviewed in QA. Nephrologist and Interventionalist/Surgeon develop criteria for determining allowable degree of intervention on current access, before the access should be “abandoned” and a new access placed. Closely monitor all AVF infiltrations to ensure that protocol for “Infiltration of New AVF” is utilized. Offer frequent in-services and educational programs on vascular access to facility staff. All staff members (licensed and non-licensed) are taught access monitoring/surveillance protocols. Provide routine in-services for staff on AVF cannulation techniques, following the recommendations of the Fistula First Initiative. Consider implementing “button-hole cannulation” in your facility, particularly for patients with AVFs that have limited cannulation sites. Develop mechanism for maintaining current diagram and flow characteristics for each patient’s AVF, for example: Incorporate AVF diagram (provided by surgeon or developed by facility) with location of access and direction of blood flow on daily treatment record. Review access diagram monthly or as necessary to keep information current. Develop a card for each AVF with a detailed picture of the access, location of arterial end and venous end, location of anastamosis, surgeon recommended cannulation areas, cannulation areas to avoid, etc. Card can be laminated and used as cannulation resource by staff. Develop and utilize procedure for treating VA infiltrations that includes giving patient/family easy to read, clearly written instructions on a “take-home” education sheet following each infiltration. Provide education on vascular access for patients and their families. A good source for reliable, professional educator reviewed VA patient education is the Vascular Access Patient Education Electronic Notebook at www.esrdnetwork.org Fistula First. Teach patients about their access – where arterial (pull) and venous (return) needles should be inserted, importance of rotating sites when using traditional cannulation techniques, protecting their access, checking the “buzz” every day, washing access at home and before every treatment, etc. Offer patients the option of learning how to self-cannulate their accesses. Page 4 of 6 Networks work with dialysis providers to give specific feedback to all decision-makers on incident and prevalent rates of AVF, AVG, and catheter use. Outcomes Feedback to Help Guide Facility Practice FFBI Change Concept 11 Review data monthly or quarterly in facility staff meetings. Present and evaluate data trended over time for incident and prevalent rates of AVF, AVG, and catheter use. Document and trend vascular access outcomes over time to identify opportunities for education/re-training: Infiltration rates by staff member. Multiple sticks by staff member. For patients with frequent infiltrations, track number and location of infiltrations to assist in the identification of a potential VA complication that would require interventional/surgical revision. Hospitals develop a comprehensive plan of care for patients at risk or with kidney disease to include: Early identification1 of patients with kidney disease to allow for: o interdepartmental protective measures programs (pharmacy, radiology) to prevent nephrotoxicity and/or further kidney damage. o interdepartmental coordination (dietary, education, social services, case management) for patient and family support. o vessel preservation measures. Modify Hospital Systems FFBI Change Concept 12 Hospital care coordination infrastructure (attending physicians, case management, quality improvement, risk management, infection control, discharge planning, social services): o to assist patients in arranging necessary care during and after a hospital stay to assure that CKD Stage 3B (eGFR 30 – 44) and CKD Stage 4 (eGRF 15 – 29) patients receive appropriate primary care follow-up and nephrology and/or surgical consults as needed. o assists patients during and after a hospital stay in arranging necessary care that ensures CKD Stages 4 (eGFR 15 – 29) and 5 (eGFR <15) patients obtain appropriate vascular access assessment, coordination and placement as well as nephrology follow-up and education regarding renal replacement therapy options. o collaborates with local dialysis centers to develop and implement discharge documentation tools that communicate detailed vascular access placement plans for patients who choose hemodialysis as their renal replacement therapy option. 1 Patients with eGFR <30 - 44 (CKD Stage 3B) Page 5 of 6 Patient Self-Management FFBI Change Concept 13 Helpful Websites Patient achieves optimum treatment outcomes and health status through collaborative knowledgebuilding related to CKD progression and treatment and through effective application of selfmanagement interventions, such as self-monitoring and decision-making. Health care clinicians utilize techniques and strategies for the education of those who participate in vascular access education and management that are designed to encourage, enhance, and support patient self-management. This includes motivational interviewing, health coaching, and other patient empowerment strategies and techniques. www.esrdnetwork.org - ESRD Network of Texas, Inc. Fistula First Project pages www.fistulafirst.org – Fistula First Breakthrough Initiative (formerly NAVII) www.esrdnetwork.org – Professionals – Fistula First – Vascular Access Toolkits Nephrologist Leadership Toolkit Helpful Tools QAPI Toolkit New AVF Toolkit Sleeves Up Toolkit MAC Catheter Reduction Toolkit Contact Information Kelly Shipley, BS, RHIA, QI Director kshipley@nw14.esrd.net 469-916-3803 Angie Wieler, MSN, RN, CNN, CPHQ, QI Coordinator awieler@nw14.esrd.net 469-916-3806 Beverly Sneed, BSN, RN, Quality/Patient Services Nurse bsneed@nw14.esrd.net 972-503-3215 Ext 310 * These Vascular Access Strategies (commonly referred to as the Fistula First Change Concepts) were developed and endorsed by the National Vascular Access Improvement Initiative (NVAII) at the beginning of the project in 2003. To access detailed information on the Fistula First Breakthrough Initiative (FFBI) formerly known as NVAII, Change Concepts and access tools developed for each area of the Change Concepts please visit: www.fistulafirst.org – Professionals – Change Concepts. Page 6 of 6