Teaching Strategy for QSEN Rubrics
advertisement

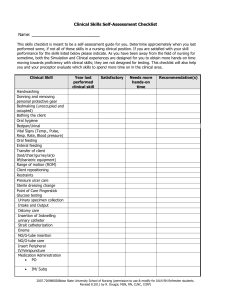
Teaching Strategy for QSEN Rubrics Setting: Clinical Facilities Learner Level: Nurse Preceptors assessing nursing students at intermediate level of QSEN competency. Strategy: Competency demonstration in the clinical setting and reflective journaling assignments. Strategy Overview: Students work with a consistent preceptor in a clinical setting two days/week during a seven week time period. The students come to clinical 6 of these weeks with a QSEN Competency Rubric after relevant materials have been presented in lecture and lab. The rubrics are completed by the preceptor and student working together. The course faculty assess reflective journaling assignments for demonstration of knowledge at the intermediate level of QSEN competency using the appropriate rubric. Remediation involves completion of the assignments until the student achieves a score of 4 or higher on each rubric. Evaluation: Scores above 4 on each of the six competency rubrics. Documentation in reflective journaling completed after each of the clinical assignments Safety: 1. The preceptor finds an opportunity for the student to participate in the universal protocol including: pre procedure verification, surgical site marking, and performing a time out. The preceptor communicates the expectation that the student will be an active participant in these initiatives. The preceptor can provided the student with a simulated experience if the student requests assistance. The preceptor evaluates the student’s participation in the universal protocol and safety initiatives with the rubric. 2. The preceptor demonstrates the 2014 National Patient Safety Goals in care of the patient. The student verbalizes the following goals: a. Improving patient identification: the preceptor and student use a minimum of two patient identifiers when checking in the patient in the preoperative area. b. The student includes the patient in the pre-procedure verification process 3. The student is included as a team member by the surgical team and preceptor as an active member in the surgical time out prior to the prep and surgical safety checklists. The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical setting. Teamwork and Collaboration: 1. The preceptor demonstrates and describes effective communication behaviors used in operating rooms during the clinical experience of the student. These include but are not limited to: a. Active listening b. Eye contact c. Respect d. Open Ended Questioning 2. The student is able to identify or describe disruptive communication not limited to: a. Noise pollution b. Verbal outbursts c. Physical outbursts 3. The preceptor teaches the student the roles and responsibilities of the circulating and scrub nurse in the perioperative setting. The student verbalizes knowledge of the role by describing roles and responsibilities of each member of the surgical team. a. Circulating Nurse b. Scrub Nurse or Surgical Technologist c. Surgeon d. Anesthesiologist e. Residents f. Medical Students The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical settings. Evidence Based Practice: Prior to this clinical experience, the student attends sterilization and disinfection lectures and has completed required readings. 1. The preceptor assists the student in finding sterilization and disinfection policies and procedures at the clinical site. 2. The student demonstrates event related sterility competency in the operating room when opening sterile supplies. 3. The student identifies correct packaging and incorrect packaging to the preceptor. 4. The student obtains one best practice evidence based article in the current literature and presents this to the students and course faculty in the lab setting. The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical setting. Patient Centered Care: Prior to the clinical assignment the student is able to verbalize the objective of patient centered care and knowledgeable of the value of assessing the care of patients through the perspective of individual perioperative patients. 1. The preceptor assists the student with using the electronic health record and patient assessments in the preoperative phase to find out patient preferences and characteristics. 2. The student documents and communicates cultural assessment findings to the surgical team members caring for the patient. The preceptor assists the patient in interviewing the patient and family members. 3. The student designs one patient intervention using findings from cultural assessment that can be used in the patient’s plan of care. The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical setting. Informatics and Technology: Prior to this assignment, each clinical site should provide orientation to perioperative documentation systems. The student has had lecture regarding the Perioperative Nursing Data Set, electronic health records, and incidence reports. 1. The student is able to verbalize three times a patient incident report should be used in the perioperative setting 2. The student demonstrates knowledge of PNDS and how it is used by operating rooms to improve and evaluate patient care and outcomes. 3. The student is able to access the electronic health record with the assistance of the preceptor and identify how it impacts patient safety and outcomes. 4. The student actively participates in counting in the circulating and scrub roles in the operating rooms. The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical setting. Quality Improvement: 1. The student can identify quality outcomes in surgical populations in the clinical area. 2. The student can identify SCIP Initiatives a. Antibiotic within one hour of incision b. Thrombolytic Prophylaxis c. Clipping (not shaving) of hair prior to prep and incision 3. The students can identify episodes which require event reporting a. Incorrect surgical counts b. Injury to patient c. Specimen issues d. Medication Errors e. Death in the operating room f. Arrests The student is assessed on the rubric by the clinical instructor and course instructor. Reflective journaling assignments are assessed for student comprehension of safety behaviors in the operating room. If the student scores below 4 on the rubric, the student must redo the assignment in the clinical setting.