20639 - Sage Products Inc.
advertisement

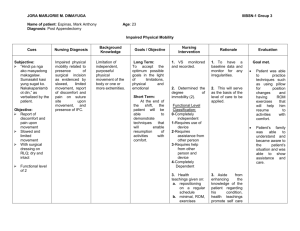
Sample Process Improvement Plan Impact of Skin Monitoring Tool on Skin Breakdown OBJECTIVE: (Example) Assess the impact of clinical intervention on early recognition and communication of skin breakdown through implementation of a new method of patient bathing which includes a unique skin monitoring and communication tool (Comfort Personal Cleansing® Bath with the I-See-Red™ Skin Check Guide), based on: 1. Improved communication among caregivers (staff) 2. Improved maintenance of skin integrity 3. Earlier detection of skin breakdown 4. Improved communication with patients POLICY: (Example) The Comfort Personal Cleansing® Bath will be used on all patients requiring bed baths unless a patient declines or has any known sensitivities to ingredients. If a patient is incontinent, also follow the incontinence care protocol. Bathing Patient with Comfort Personal Cleansing® Bath with I-See-Red™ Skin Check Guide 1. 2. (Example) 20639 1. PROCEDURE: (Example) Background: (Example) Your facility’s historical skin breakdown rates as compared to current protocol and procedures with the I-See-Red Skin Check Guide, which supports JCAHO’s 2005 National Patient Safety Goal of improving the effectiveness of communication among caregivers. In January 2004, skin breakdown rates housewide were recognized as high. After review of the literature and subsequent implementation of enter current protocol…here. RESULTS: (Example) 3. 4. 5. Warming the Comfort Personal Cleansing Bath Product a. Warm according to directions on the package. b. Consult package for complete indications, ingredients and warnings. Bathing with the Comfort Personal Cleansing Bath a. Ensure a private environment. KEY POINT: Use a towel or sheet to cover the patient appropriately to protect their privacy as you progress through the bath. b. Remove the Skin Check Guide from the bath package and place in an accessible location. c. Peel back the package label and test the temperature of the washcloths. If temperature is acceptable to your touch you may proceed with the bathing process. If not, stop procedure. Repeat every 10 minutes until temperature is acceptable to patient. KEY POINT: Remember, gloves diminish your sensitivity to heat. Obtain feedback from your patient on his or her comfort with the bath. Continue to monitor patient’s comfort level with temperature as bath progresses. d. Remove the first washcloth. Clean the face, neck and upper torso with the #1 washcloth and discard. No rinsing or drying is required. KEY POINT: Following the bathing procedure in a sequenced order reduces the chance of cross contamination by providing a clean washcloth for separate areas of the body while maximizing appropriate use of the product to prevent waste. KEY POINT: In patients who have a potential for moisture entrapment in skin folds, it may be necessary to pat dry with clean soft towel. Use caution around dressings, intravascular lines, etc. e. Remove the #2 washcloth. Clean the right arm and armpit with the #2 washcloth and discard. f. Remove the #3 washcloth. Clean the left arm and armpit with the #3 washcloth and discard. g. Remove the #4 washcloth. Clean the perineal area with the #4 washcloth and discard. If patient is incontinent, clean perineal area according to the incontinence care policy and procedure. h. Remove the #5 washcloth. Clean the right leg with the #5 washcloth and discard. i. Remove the #6 washcloth. Clean the left leg with the #6 washcloth and discard. j. Remove the #7 washcloth. Ask the patient to turn on their side, if able, or obtain assistance, as necessary. Clean the upper back with the #7 washcloth and discard. k. Remove the #8 washcloth. Clean the buttocks with the #8 washcloth and discard. If additional cleaning in the buttocks region is necessary due to incontinence, refer to incontinence care policy and procedure. l. Once the bath is completed, apply clean gown, cover the patient as appropriate and return side rails to correct position. DO NOT FLUSH WASHCLOTHS. m. Complete additional personal hygiene activities as necessary (oral care, comb hair and clean nail beds; wash hair and shave facial hair as necessary). Educate the patient/family about importance of personal hygiene. Clean the work environment and leave the patient in a safe, comfortable position. Return the head of bed to a 30-degree position if no contraindications or discomfort. Documentation: a. Using the Skin Check Guide, mark areas of skin redness, irritation, bruising, blistering, discoloration, cuts/open areas, unusual moles, or any skin condition you are unsure of on the appropriate body diagram. Document patient ID, location and who completed the skin monitoring check. If skin monitoring was completed by a nursing assistant, give the completed guide to the RN assigned to the patient for follow up skin assessment. Otherwise, place the Skin Check Guide in a designated documentation location as applicable. b. Document completion of the procedure on your facility’s appropriate form. Author: Kathleen M. Vollman, MSN, RN, CCNS, CCRN, FCCM Clinical Nurse Specialist/Educator/Consultant ADVANCING NURSING 2004 Note: For “Purpose,” “Articles Needed,” and “References” (used to develop this sample protocol), download the complete protocol at: www.sageproducts.com/products/skincheck.asp. This new bathing method (Comfort Personal Cleansing® Bath with I-See-Red™ Skin Check Guide) enables me to better meet my unit’s protocol. Sample Results: You can create and import your own pie charts or graphs from information compiled from your facility’s completed Clinical Feedback Forms. 2. Comfort Personal Cleansing Bath’s one-step cleansing and moisturizing washcloths enable me to use my time more efficiently to monitor the patient’s skin condition… 10% Agree 90% Strongly Agree 3. The I-See-Red™ Skin Check Guide is an effective communication tool between the patient, caregiver and nurse. 4. The I-See-Red™ Skin Check Guide is easy to use. 5. The I-See-Red™ Skin Check Guide is a useful reminder of the importance of skin monitoring. 6. I believe this new bathing method is an important improvement in the quality of patient care at this facility. Results: Data through: Rate = Number of skin breakdowns observed/communicated: Average prior rate: Average post rate: Average length of stay prior to intervention: Average length of stay post implementation: Economic Impact: Average cost of nosocomial pressure ulcer: Average cost per month prior to intervention: Average cost per month post implementation: Savings per month: