and Nidal Toman, MD
advertisement
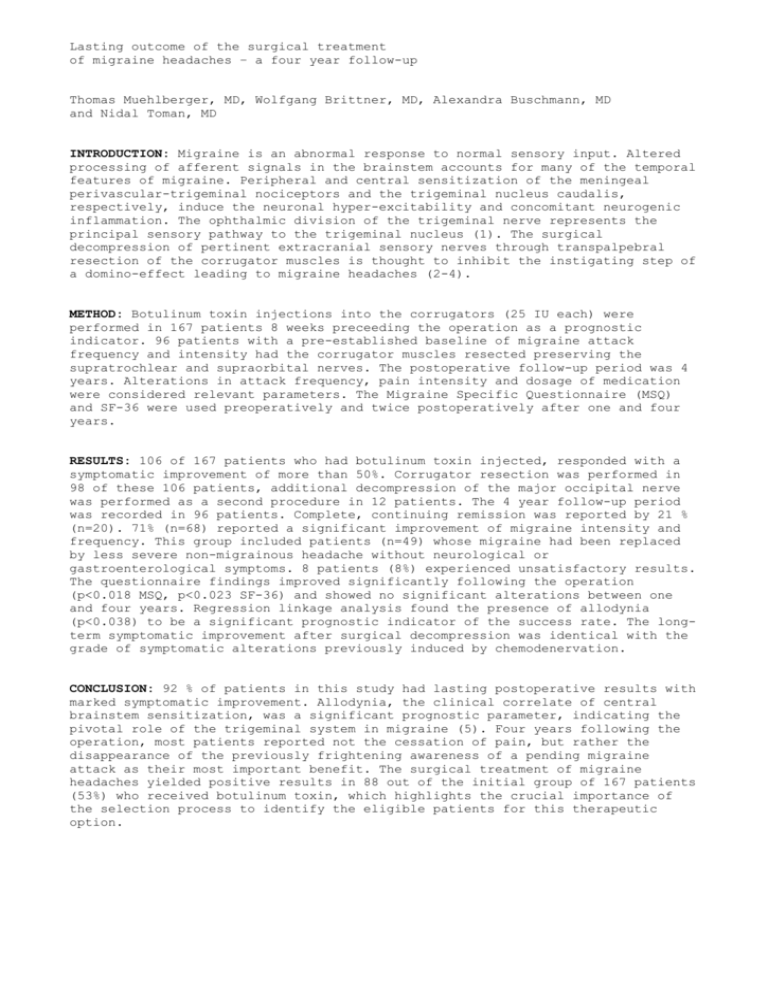
Lasting outcome of the surgical treatment of migraine headaches – a four year follow-up Thomas Muehlberger, MD, Wolfgang Brittner, MD, Alexandra Buschmann, MD and Nidal Toman, MD INTRODUCTION: Migraine is an abnormal response to normal sensory input. Altered processing of afferent signals in the brainstem accounts for many of the temporal features of migraine. Peripheral and central sensitization of the meningeal perivascular-trigeminal nociceptors and the trigeminal nucleus caudalis, respectively, induce the neuronal hyper-excitability and concomitant neurogenic inflammation. The ophthalmic division of the trigeminal nerve represents the principal sensory pathway to the trigeminal nucleus (1). The surgical decompression of pertinent extracranial sensory nerves through transpalpebral resection of the corrugator muscles is thought to inhibit the instigating step of a domino-effect leading to migraine headaches (2-4). METHOD: Botulinum toxin injections into the corrugators (25 IU each) were performed in 167 patients 8 weeks preceeding the operation as a prognostic indicator. 96 patients with a pre-established baseline of migraine attack frequency and intensity had the corrugator muscles resected preserving the supratrochlear and supraorbital nerves. The postoperative follow-up period was 4 years. Alterations in attack frequency, pain intensity and dosage of medication were considered relevant parameters. The Migraine Specific Questionnaire (MSQ) and SF-36 were used preoperatively and twice postoperatively after one and four years. RESULTS: 106 of 167 patients who had botulinum toxin injected, responded with a symptomatic improvement of more than 50%. Corrugator resection was performed in 98 of these 106 patients, additional decompression of the major occipital nerve was performed as a second procedure in 12 patients. The 4 year follow-up period was recorded in 96 patients. Complete, continuing remission was reported by 21 % (n=20). 71% (n=68) reported a significant improvement of migraine intensity and frequency. This group included patients (n=49) whose migraine had been replaced by less severe non-migrainous headache without neurological or gastroenterological symptoms. 8 patients (8%) experienced unsatisfactory results. The questionnaire findings improved significantly following the operation (p<0.018 MSQ, p<0.023 SF-36) and showed no significant alterations between one and four years. Regression linkage analysis found the presence of allodynia (p<0.038) to be a significant prognostic indicator of the success rate. The longterm symptomatic improvement after surgical decompression was identical with the grade of symptomatic alterations previously induced by chemodenervation. CONCLUSION: 92 % of patients in this study had lasting postoperative results with marked symptomatic improvement. Allodynia, the clinical correlate of central brainstem sensitization, was a significant prognostic parameter, indicating the pivotal role of the trigeminal system in migraine (5). Four years following the operation, most patients reported not the cessation of pain, but rather the disappearance of the previously frightening awareness of a pending migraine attack as their most important benefit. The surgical treatment of migraine headaches yielded positive results in 88 out of the initial group of 167 patients (53%) who received botulinum toxin, which highlights the crucial importance of the selection process to identify the eligible patients for this therapeutic option. REFERENCES 1. Dellon AL, Andonian E, DeJesus RA. Measuring sensibility of the trigeminal nerve. Plast Reconstr Surg 120:1546-1550, 2007. 2. Guyuron B, Kriegler JS, Davis J, Amini SB. Comprehensive surgical treatment of migraine headaches. Plast Reconstr Surg 115:1-9, 2005. 3. Dirnberger F, Becker K. Surgical treatment of of migraine headaches by corrugator muscle resection. Plast Reconstr Surg 114:652-657, 2004. 4. Muehlberger T, Fischer P, Lehnhardt M. The anatomy of the surgical treatment of migraine. Zentralbl Chir 130:288-292, 2005. 5. Mathew NT, Kailasam J, Seifert T. Clinical recognition of allodynia in migraine. Neurology 63:848-852, 2004.


![[Plan Logo] [INSERT DATE] Dear Employer: About 36 million](http://s3.studylib.net/store/data/006909432_1-5c160caea8d3c9b2927369f2f795ecc4-300x300.png)