MRI Protocol
advertisement

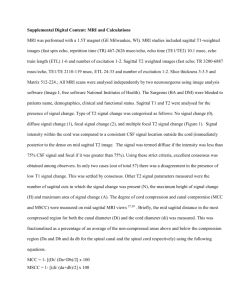
MAGNETIC RESONANCE IMAGING IN ARVC Cardiac MRI studies for the diagnosis of ARVC should only be performed in units with appropriate hardware and experience in cardiac MRI studies. Interpretation of such MRI studies should be done by readers with experience in cardiac MRI and knowledge of clinical ARVC diagnosis. The following is a proposal for a uniform cardiovascular Magnetic Resonance Imaging (MRI) protocol for the diagnosis of ARVC. The protocol is designed to be performed with standard equipment and includes basic and optional features to allow performance of MRI studies which are comparable between participating units. A) Subject Preparation Patient informed consent Pharmacologic control of arrhythmia or sinus tachycardia (if necessary) B) Image Acquisition: Hardware 1.5 Tesla MR scanner (modern-generation equipment preferred) Thoracic torso or cardiac coil (phase array receiver coil) Anterior surface coil may be used to reduce “wrap around “ artifact. Field of view preferred: 24-26 cm (but <32 cm). C) Image Acquisition: Sequences 1. Ventricular anatomy, wall thinning, fatty infiltration a. ECG-gated turbo spin echo, transaxial plane, to cover from above the pulmonary valve to the diaphragm. Suppression of blood pool signal (black blood; preparatory double inversion pulse). Either 3 mm multi-slice (4 NEX, 5 mm gap, respiratory compensation) or 5 mm single slices (1 NEX, 3 mm gap, multiple acquisitions during breath holds). Fast spin echo technique recommended only for breath-hold images. In plane pixel resolution should be <1.5 x 1.5 mm. b. Same turbo spin echo sequence in the short axis plane from base to apex of both ventricles. 2. Ventricular function (regional and global): Breath-hold cine gradient echo sequences (Steady State Free Precession = SSFP) preferred (TrueFISP, balanced fast field echo (FFE), Fiesta), encompasssing the entire RV and LV in both transaxial and short axis planes (corresponding spin echo and cine acquisitions to allow direct comparison). 10 mm gap between center of slices and optimal thickness according to local practice (not < 5 mm. 3. Optional: a) Other planes (sagital, RVO-view, long-axis 4-chamber) in spin-echo and/or cine MRI. b) Motion/artifact control techniques: i.e. saturation band behind the anterior RV free wall (transaxial planes) to improve image quality. c) Fat suppression double inversion recovery fast spin echo images to improve identification of intramyocardial fatty replacement. D) Image Analysis: 1. Quantification of global and regional RV and LV volumes, function and mass. 2. Examination of RV anatomical (structural) abnormalities such as thinning, bulging, abnormal trabeculation, etc.. 3. Examination of possible fatty replacement of RV and/or LV myocardium by identification of abnormal intramyocardial fat (signal increase in T1-weighted images) with/without optional use of fat-suppressed images. 4. Examination of other known causes and locations of cardiac fat, i.e., epicardial fat, obesity, RCA/LAD groove, AV-groove, atrial lipomatous hypertrophy, etc. to avoid misdiagnosis of myocardial fatty replacement. 5. Examination of regional RV and LV wall motion abnormalities on dynamic cine-MR images/movies. 6. Direct comparison of possible fatty replacement and/or wall thinning sites on spin echo images with regional wall motion in corresponding areas on dynamic cine MR images/movies. 7. Examination of LV involvement by analysis and direct comparison of spin echo and cine MR images/movies.