lateral infection
advertisement

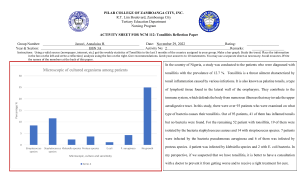
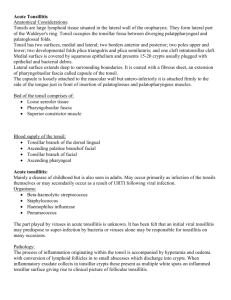
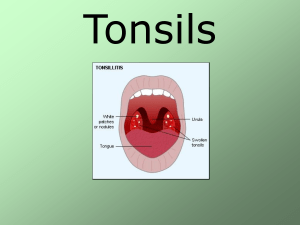
10.23 Diseases of the Throat Recognise and distinguish the common causes of oral ulceration Assoc w systemic disorder IBD (Crohns / UC) Coeliac disease Systemic / discoid lupus Behçets disease Neutropenia Immunideficiency Reiters disease Stevens-Johnsons syndr Starchans syndrome Assoc w dermatologic dis. Lichen planus Dermatitis herpetiformis Erythema multiforme major Toxic epidermal necrolysis Pemphigus vulgaris mucous membr pemphigoid Assoc. w viral infection Herpes simplex I/II Coxsackie (hand, foot and mouth disease) Zoster (chickenpox) Cytomegalovirus Assoc w drugs antimalarials Methyldopa Tolbutamide Penicillamine Gold salts Assoc w deficiency Iron B12 Folate Vitamin C Others Syphilis infection Tuberculosis infection Trauma (ill-fitting dentures, toothbrushing, sharp teeth) Neoplasm (SCC) Those in bold are more likely to be causes of oral ulceration History: GI symptoms, rashes, drug history, dietary history, dentures, fever / sweats etc. Examination: rashes, pallor, oral cavity including floor of mouth and entire surface of tongue. SCC produces indurated aphthous ulcers with raised and rolled edges, usually on the floor of the mouth or lateral borders of the tongue. Background box: diseases causing oral ulceration Behcet's syndrome is a chronic multisystem venulitis of unknown aetiology. It is characterised by: recurrent oral and genital ulcers, arthritis, iritis, and neurological disease. It is three times more common in males than females. Pemphigus: This is a group of conditions that are characterized by the formation of blisters within the epidermis of both skin and mucous membranes. Current evidence suggests that there is an autoimmune basis. Incidence is slightly higher in women, and in Asians and Jews. Peak onset is between 60 and 70 years of age. Reiters disease is a reactive arthritis and comprises a triad of symptoms: urethritis, conjunctivitis and a seronegative arthritis. Two broad subtypes are recognised: an enteric form related to gastrointestinal infection and a genital form related to sexual activity. Erythema multiforme is a term describing target lesions - circular lesions often with central blister with a symmetrical peripheral distribution, usually on limbs. Stevens Johnson syndrome is a severe and sometimes fatal form of erythema multiforme. There are often mouth, genital and eye ulcers and fever. There is a higher incidence in children and young adults, and it is twice as common in males than females. There may be pulmonary, gastrointestinal, cardiac or renal involvement. Strachans syndrome is the combination of: orogenital ulceration, sensory neuropathy, and amblyopia. The aetiology is unknown. Recognise and manage tonsillitis The tonsils and adenoids are aggregates of lymphatic tissue within the oral cavity - they form what is known as Waldeyers ring (see pic right). Tonsillitis may occur at any age but is most common under 9 years old, in winter and spring. Spread is by droplet infection with 50-85% of cases probably being viral. Symptoms include: sore throat and dyspahgia; earache (referred otalgia); headache and malaise. Signs include: Pyrexia (may be high); enlarged hyperaemic tonsils (may exude pus); inflamed pharyngeal mucosa; foetor; and cervical lymphadenopathy. The management of tonsillitis is as follows Bed rest High fluid intake Soluble paracetamol (or aspirin in adults) held in the mouth and then swallowed. Antibiotics if severe. Injected penicillin followed by 10 days orally is usual treatment of choice. Important differentials include: infectious mononucleosis, scarlet fever, diphtheria, HIV. Sore throat + malaise + pyrexia +/- cervical nodes odynophagia/ dysphagia Pain may be referred to the ear via the glossopharyngeal nerve Halitosis Mouth breathing If dysphagia is severe & limiting oral intake of food/liquid ADMIT If TRISMUS/ Drooling/ Hot potato voice = peritonsillar abscess Organisms Viral (~70%): HSV (red, swollen tonsils. May have aphthous ulcers on their surfaces) Cytomegalovirus Adenovirus Measles virus EBV (with palatal petechiae) may cause tonsillitis in the absence of mononucleosis. Common in young children. A grey membrane may cover tonsils Consider infectious mononucleosis (MN) due to EBV in adolescents/ young children with acute tonsillitis, particularly when tender cervical, axillary, and/or inguinal nodes; splenomegaly; severe lethargy and malaise; and low-grade fever accompany acute tonsillitis. Bacterial (~15-30%) Group A ß haemolytic Strep (pyogenes) Strep pneumonia H. influenzae S. aureus Bacteriodes fragilis (recurrent tonsillitis) Viral & bacterial causes difficult to discern clinically Tonsils may be covered in white plaques in bacterial infections Differential Peritonsillar abscess Infectious mononucleosis Diphtheria Scarlet fever (RARE): Strep tonsillitis + punctuate erythematous rash, whiteness around mouth + strawberry & cream tongue) Investigations Blood: FBC, WCC, ESR, U&E Throat swab Monospot test Blood culture Rx. Rest Encourage fluids Soluble paracetamol Penicillin 500mg TDS 10days NOT AMOXICILLIN: this causes a rash in infectious mononucleosis Admit if fluid & oral intake is significantly restricted or quinsy present Inpatient Rx IV FLUIDS Analgesia Oral morphine Ibuprofen Paracetamol (IV if necessary) ABx: Benzylpenicillin 1.2mg QDS (<300mg/min) & Metronidazole (500mg/8hs) Steroids: Prednisolone/IV hydrocortisone if necessary Recurrent tonsillitis Likely to be disrupting school/ ADL (takes up to 2 weeks to fully recover) Long term low dose ABx: (250mg penicillin) or start course with each cold if child always gets tonsillitis with colds Tonsillectomy if: 7 attacks in 1 year 5 in each of the last 2 years 3 in each of the last 3 years Airway obstruction Quinsy Discuss pros & cons with patient/parents Complications Hemorrhage Infection of tonsillar fossa Otitis media (Pulmonary abscess/ Pneumonia) Due to aspiration of blood/tissue (RARE) Recognise quinsy Quinsy is the name given to a peritonsillar abcess (see pic right). This abcess is usually a complication of acute tonsillitis and is more common in adults. Pus collects in the space between the tonsil and the pharyngeal tonsil and causes: fever pain dysphagia referred otalgia trismus (difficulty opening the mouth). Note the displaced uvula (which may be very oedematos) and tonsil. Systemic antibiotic is strongly indicated without delay together with incision to drain the abcess if much trismus is present. In young children this should be done under general anaethesia. A tonsillectomy is often carried out six weeks post drainage. Pus outside the tonsillar capsule. Complication of strep tonsillitis Severe tonsillitis + trismus +/- halitosis & drooling Hot potato voice due to pharyngeal oedema Patient continues to become more ill despite ABx. Severe dysphagia (sometimes unable to swallow saliva) Referred earache common Complications: parapharyngeal abscess mediastinitis Rx Admit to hospital drainage (never attempt in GP due to proximity of the external carotid artery) IV Fluids & solid food when able IV Penicillin/erythromycin + metronidazole (usually marked improvement in 12 hrs) Consider tonsillectomy in 6 weeks