NEU/1 (P) ACUTE DISSEMINATED ENCEPHALOMYELITIS (ADEM
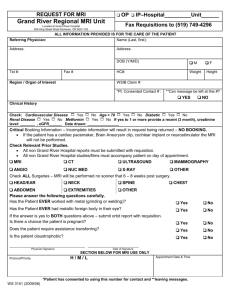
advertisement

NEU/1 (P) ACUTE DISSEMINATED ENCEPHALOMYELITIS (ADEM) IN 9 YEAR OLD CHILD Ravinder K Gupta, Vikas Sharma Associate Professor, Department of Pediatrics, Acharya Shri Chander College of Medical sciences (ASCOMS), Jammu J&K - 180017 Email: drrk_gupta2000@yahoo.com A 9 years old male child belonging to a good socioeconomic status, studying in class 4th standard presented with intermittent fever for almost one month, headache off and on for 15 days, irritability, vomiting, and pain abdomen for 5 days and noticed weakness of right side of body for last 2 days . He had speech difficulty and expressive aphasia. There was no history of any recent vaccination, visual disturbances, hepatitis or any exanthemata in the past. On examination vitals were normal, pupils were bilaterally reacting, tone was normal, moving right side less as compared to left and reflexes were present. The fundus examination was normal. There were no signs of meningeal irritation and right plantar was up going. . Investigations carried out for systemic diseases were unremarkable including blood cultures, LFT, RFT, montoux test and blood sugar. Electrocardiogram and Chest X-ray were normal. CSF analysis including viral cultures were normal. CT-scan of brain was normal but contrast enhancement MRI revealed few small hyper intense lesions in the sub cortical white matter of cerebral hemispheres, left caudate nucleus and rostrum of corpus callosum on right side suggestive of acute disseminated encephalomyelitis. He was treated with intravenous Methyl Prednisolone (30mg/kg/day) for 3 days and then started on oral Methyl Prednisolone (1mg/kg/day) for two weeks and was discharged with a advise to taper the steroids within 10 days . The child showed dramatic improvement to this therapy and led to resolution of all his neurological deficits. Follow up for 6 months revealed no neurological deterioration. To conclude, ADEM is likely to be diagnosed with greater frequency with MRI evaluation of children presenting with encephalomyelitis. NEU/2 (P) COARCTATION OF AORTA PRESENTING HAEMORRHAGIC STROKE IN A 14 YEAR ADOLESECENT BOY Gurdeep S. Dhooria, Harmesh S. Bains, Deepak Bhat 753 'I' Block Brs Nagar Ludhiana-141012 Email: gurdeep2005_123@sify.com AS ACUTE We report a 14 years adolescent boy, who presented for the very first time with acute haemorrhagic stroke with MRI brain showing subarachnoid hemorrhage with intraventricular hemorrhage. CT cerebral angiography of the brain was done which revealed lobular sacculated aneurysm of left vertebral artery (V4 segment) and saccular aneurysm of anterior communicating artery. Fundus examination done in view of persistent hypertensive records, showed hypertensive retinopathy, suggesting an alternate diagnosis. Four limb blood pressure readings showed discrepancy in the upper and lower limb readings with higher BP values in upper limbs. Chest x-ray showed features of left ventricular enlargement and characteristic rib notching. Diagnosis was confirmed by echocardiography and CT angiography. Intracranial aneurysms are more often found in patients with aorta coarctation than in general population, and aneurysm rupture occurs much earlier in these patients. Before presenting with cerebrovascular complications, the disease can easily be diagnosed with four limb blood pressure measurements, physical examination and radiological investigations like echocardiography. This case of aorta coarctation was diagnosed because of its cerebrovascular complications. NEU/3 (P) CEREBELLAR ATROPHY IN FALCIPARUM MALARIA- A CASE REPORT P. Sriram, Associate Professor, Department of Pediatrics, Indira Gandhi Medical College and Research Institute, Puducherry-605009 Email: psriram_ped@yahoo.co.in Abstract: Malaria is one of the most common infectious diseases and poses an enormous public health problem. It afflicts more than 500 million people, causing more than one million deaths each year. Severe neurological complications are associated with falciparum malaria. Its overall incidence is 0.1% in patients with malaria due to falciparum malaria. Despite adequate treatment, 10.5% of survivors develop sequelae in the form of psychosis, ataxia, hemiplegia, cortical blindness, aphasia and extrapyramidal signs . Cerebellar involvement in falciparum malaria is in the form of acute cerebellar ataxia, delayed cerebellar ataxia and post malarial neurological syndrome and usually respond to antimalarial therapy. But the occurrence of cerebellar atrophy in falciparum malaria has not been described till date.We describe the case of an eight year old male child with severe plasmodium falciparum malaria with high-level parasitemia and severe thrombocytopenia. Child was provisionally diagnosed as cerebral malaria and was treated with Artesunate, doxycycline and ceftriaxone. There were features of abnormal gait, speech difficulty and altered behavior pattern during the recovery phase. This occurred even after receiving antimalarial therapy. MRI sequences on T1 saggital and T2 coronal images showed diffuse atrophy of vermis and both cerebellar hemispheres. The suprarachnoid space in the posterior fossa and cisterna magna were dilated. Cerebral cortex, brain stem, thalamus and basal ganglia were normal. Child was adviced for physiotherapy with special emphasis on pelvic muscle exercises and gait training. Parents were councelled regarding the condition of the child and were adviced for regular follow up. NEU/4 (P) BRAIN STEM TUMORS MASQUERADING AS INFECTIOUS SPACE OCCUPYING LESIONS: RETROSPECTIVE ANALYSIS FROM TERTIARY CARE HOSPITAL Sweta Mukherjee, Abhishek Pandey, Shuvendu Roy, Daljit Singh, Girish Gupta and KS Rana Department of Pediatrics, Armed Forces Medical College, and Command Hospital (Southern Command) Pune, Maharashtra Email: sonai24@yahoo.com Introduction: Brain stem space occupying lesions (SOLs) are associated with dramatic presentations with upper-motor-neuronal symptoms, cranial nerve palsies, gait instabilities, and features of raised intra-cranial pressures. Magnetic resonance imaging (MRI) with spectroscopy is the mainstay in diagnosis of these lesions. Aims and Objectives: Data of children who were initially diagnosed as brain stem infectious SOL and later established to have brain stem malignancies were analyzed to compare their MRI/spectroscopy analysis with the final histopathological diagnosis. Materials and Methods: Retrospectively, we identified four patients between June 2009 to June 2012 who were initially diagnosed to have brain stem infectious SOL but subsequent histopathological analysis revealed malignant lesions. Results: The mean age of patients was 7years (3 male). The clinical presentations were: ataxia (n=3), seizures (n=1), and raised intra-cranial pressure (n=1). The additional clinical features included fever (n=3), cough and contact with tuberculosis (n=2), and otitis media (n=1). MRI revealed ring-enhancing lesions in pons (n=2), cerebello-pontine angle (n=1) and midbrain (n=1). Spectroscopy suggested a normal choline peak for all patients. Initial 3linic-radiological diagnoses were: tuberculoma (n=2), brain abscess with otitis media (n=1), and neurocysticercosis (n=1). Subsequent histopathological analyses were suggestive of astrocytoma (n=2), primitive neuro-ectodermal-tumor (n=1) and rhabdomyosarcoma (n=1). The median delay in diagnosis of malignancy was 42days (range 16-55 days). Conclusion: MRI with spectroscopy though an indispensible initial step while analyzing children with suspected brain stem lesions is not flawless. Histopathological analysis should be resorted to whenever possible to rule out malignancy in brain stem SOLs. NEU/5 (P) POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME IN CHILDREN: A RETROSPECTIVE ANALYSIS OF CLINICO-RADIOLOGIC SPECTRUM Aditi Sharma, Aradhana Aneja, Swati Dash, Biju John, KS Rana, Girish Gupta Department of Pediatrics, Armed Forces Medical College, Pune, Maharashtra. Email: aditidhills@gmail.com Introduction: Posterior reversible encephalopathy syndrome (PRES) is a clinico-radiologic phenomenon associated with a variety of medical conditions including renal, hematological and malignant disorders. Hypertension and immunosuppressive therapy are common triggers of PRES in children. Aims and Objectives: To analyze cohort of pediatric patients diagnosed as PRES at a tertiary care referral hospital in order to identify the predisposing factors, describe the clinico-radiological features and report the clinical outcome. Materials and Methods: Retrospectively, we identified twenty-nine patients (19 males) who had clinical (transient encephalopathy) and radiological (hyper-intense T2 signal consistent with edema and improvement of abnormal signal in follow-up neuroimaging) features consistent with PRES between January 2006 to August 2012.Results: The mean age at the time of PRES onset was 7years. Primary diagnosis was acute lymphoblastic leukemia (n=17), acute myeloid leukemia (n=3), rhabdomyosarcoma (n=3), hepatoblastoma (n=1), neuroblastoma (n=1), and chronic kidney disease (n=4). Pharmacologically, steroids, L-asparginase and methotrexate were administered to 17/29, 15/29, and 16/29 patients respectively. Seizures (23/29), altered sensorium (16/29), and visual disturbance (12/29) were the commonest clinical presentations. Concurrent brain magnetic resonance imaging (MRI) demonstrated T2 signal abnormalities (29/29), restricted diffusion (13/29) and hemorrhage (5/29). Frontal lesions occurred as frequently as parietal lesions followed by occipital lesions. Follow-up MRI demonstrated changes consistent with previous hemorrhage in 5 patients and ischemia in two patients. Neurological deficits persisted in 3/29 patients. Conclusion: Children with PRES can have heterogeneous clinical and radiological findings, some of which are irreversible. NEU/6 (P) A CASE OF BIOTINIDASE DEFICIENCY PRESENTING AS QUADRIPARESIS Rajeev Thapar, Kannan Venkatnarayan Department of Pediatrics, Command Hospital (Eastern Command), Alipore Road, Alipore, Kolkata 700027 Email: rajeevrenuthapar@gmail.com Abstract: Introduction: Biotinidase deficiency is a rare metabolic disease with estimated incidence of approximately 1:61,067 (1). This enzyme is required for the restoration of free Biotin from Biocytin after it has activated various carboxylases, in the Biotin cycle (2, 3). Absence of Biotinidase results in Biotin deficiency, which results in a wide spectrum of neurological, dermatological and immunological abnormalities (4). Identification of this disorder is important as it is easily treatable and the patients show dramatic response to therapy, besides the fact that it can prove fatal if not diagnosed. We report a case of Biotinidase deficiency who presented with quadriparesis, highlighting all these issues. Case Report: A 3 years 10 month old girl child was referred to our hospital with complaints of episodes of rapid breathing and progressive weakness of all four limbs. Over the period of time she developed weakness of all four limbs, manifesting as unsteady gait and inability to self-feed. The weakness progressed and she was bed ridden at the time of admission. She was a product of a non- consanguineous marriage, with no remarkable delay in attaining the target developmental milestones. Her elder brother had died following similar clinical manifestations of progressive weakness at 4 years of age. Clinically she was alert and had silent tachypnea. Skin manifestations in form of Candida lesions of the toe clefts and axilla along with alopecia were present; the bilateral plantars were extensor with gross hypotonia and the power in the proximal muscles of both limbs being grade II. Base line investigations revealed partially compensated metabolic acidosis. MRI studies showed mild cerebral atrophy with hypoplasia of cerebellar vermis. MRI of spine was suggestive of myelopathy. CSF study, ophthalmologic and audiological evaluations were normal. In view of family history and the episodic nature of respiratory complaints suggestive of metabolic acidosis, along with the skin manifestations, possibility of neurometabolic syndrome was considered. Serum lactate was elevated (31 mg/dl (4.5-19.8 mg/dl)) and the Biotinidase activity was 0 nmol/min/ml. The child was started on daily oral Biotin 20 mg and made significant recovery. Discussion: Deficiency of Biotinidase results in deficiency of Biotin, which is required as a catalyst for the carboxylase systems in the body. Though, individual deficiencies of all four Carboxylases have been reported, the clinical spectrum varies widely from a severe form presenting early (multiple carboxylase deficiency, holocarboxylase synthase deficiency) to milder varieties presenting late (Biotinidase deficiency) (5, 6). The clinical spectrum of Biotinidase deficiency depends on the severity of the defect. The clinical manifestations predominately include neurological, skin and respiratory manifestations. The neurological spectrum includes seizures, hypotonia, and developmental delay in the early period. The present case had progressive spastic quadriparesis and muscle weakness. Seborrheic dermatitis, alopecia and Candidal infections due to immunological dysfunction are the predominant skin manifestations and our patient had most of these features. Metabolic acidosis resulting in hyperventilation, often masquerades as a primary respiratory illness, as in this patient. Identification of this disorder is important as it can be treated with supplementation of Biotin. Lifelong supplementation up to 40 mg/day is needed and results in both clinical and radiological improvement. NEU/7 (P) SUBACUTE COMBINED DEGENERATION OF SPINAL CORD DUE TO VITAMIN B12 DEFICIENCY IN TWO CHILD: CASE REPORT Manish Rasania, Hardik Gandhi, Vaibhav Patel, Lalit Nainiwal, Dulari Gandhi Department of pediatrics, Dhiraj Hospital, Pipariya, Gujarat Email: hardikgandhi26@yahoo.co.in Vitamin B12 deficiency causes haematological, gastrointestinal, psychiatric and neurological diseases. Subacute combined degeneration (SACD) of the spinal cord, characterized by degeneration of the lateral and posterior columns, is often found due to vitamin B12 deficiency. SACD is more common in elderly population. We report 2 cases in children. CASE 1: 17 year male patient presented with complain of abdominal pain and difficulty in walking since 15 days. Higher mental functions were normal. Romberg’s test was positive. Patient was moderately anemic (Hemoglobin 8.7 gm%). CBC, blood indices and peripheral smear examination findings were suggestive of macrocytic anemia. Patient’s Sickling test was positive. Hb electrophoresis showed sickle cell trait. MRI spine – showing infarction in thoracic vertebrae and hyperintensity throughout the spinal cord especially in post column suggestive of subacute combined degeneration of spinal cord. Serum Vitamin B12- 114 pg/ml (normal range 211 – 900 pg/ml). CASE 2: 16 year female presented with complain of difficulty in walking since 15 days and tingling and numbness over limbs since 1 year. Patient was mildly anemic (hemoglobin 9.6 gm%). Blood indices with peripheral smear showed macrocytic anemia. In these child also Romberg’s test positive and higher mental function was normal. MRI brain with spine- showing hyperintensity throughout the spinal cord in post column suggestive of subacute combined degeneration of spinal cord with no significant intracranial abnoramality. Serum Vitamin B12 was <50 pg/ml. Both the children treated with injection Cyanocobolamine intramuscularly daily for 2 weeks, followed by 1000 mg weekly for a month followed by 1000 mg monthly. Response to therapy was dramatic with improvement in clinical symptoms noticed within few days of therapy and near complete improvement of gait & resolution of ataxia within 2 months. Conclusion: Vitamin B12 deficiency has become more prevalent in society. Though increasingly reported in elderly patients, more and more reports are coming up with vitamin B12 deficiency related problem in adolescent and young adult population. Commonest presentation of vitamin B12 deficiency is megaloblastic anemia. Neurological deficiency with subacute combined degeneration of spinal cord is not very frequent. Any child with gait disturbance and tingling and numbness vitamin B12 deficiency should be suspected especially if he is also having megaloblastic anemia. Early spinal MR imaging assists in the early diagnosis and treatment of the disease. NEU/8 (P) TUBERCULAR MENINGITIS PRESENTING AS GRADENIGO SYNDROME Sanjeev Khera, Brig M Kanitkar Dept of Pediatrics, Military Hospital Danapur, Danapur (Bihar) - PIN 801503 Email: kherakherakhera@gmail.com Introduction- Gradenigo described a symptom complex of suppurative otitis media, pain in the distribution of the trigeminal nerve,and abducens nerve palsy. Tubercular meningitis per say has not been described in literature manifesting as Gradenigo’s syndrome. Case Report11 yr old male was admitted with history of fever, headache, double vision for 20 days duration. He had intermittent fever with severe throbbing Lt sided retro-orbital headache. There was no history of contact with patient of tuberculosis, wt loss, poor wt gain, chronic cough. With above complaints he took multiple consultations with irregular antibiotic treatment for last 15 days. He had h/o CSOM Lt since infancy for which he was on irregular treatment. On examination he was sick looking with grade I protein energy malnutrition. BCG scar was present. Otherwise there were no stigmata of Tuberculosis.CNS examination revealed a positive Kernig’s sign with neck rigidity. He had a Lt Lat Rectus palsy (Fig.1). ENT examination revealed Lt attico-antral perforation with no active pus discharge. Rest of the systemic examination was normal. CECT brain was normal and there were no features of raised ICT.CSF examination at our centre revealed WBC= 200/cmm (Neutrophil : Lymphocyte ratio=50:50), RBC= 10/cumm, Protein= 90 mg/dl, Sugar= 45 mg/dl ( as against a BSL= 109 mg/dl), Gm stain/AFB stain were negative. He was managed as a case of partially treated meningitis to start with and was administered injectable 3rd generation cephalosporins. However there was no clinical improvement despite antibiotic therapy in next 05 days. CSF culture was reported as sterile. In view of no response to antibiotic therapy, the child was investigated for tuberculosis. Chest X ray revealed non homogenous opacity of Rt middle zone Monteux reaction and sputum for AFB were negative. On the basis of above, first line ATT (2HRZE+8HR) was started along with 08 weeks of steroids followed by gradual tapering of steroids. Though over next 02 weeks the fever and meningeal sign improved the child continued to complain of severe throbbing Lt sided headache. A repeat CECT brain revealed tuberculoma in the floccules of Lt cerebellar hemisphere with perilesional oedema (Fig.2). It also revealed partially sclerosed Lt mastoid air cells. At this time diagnosis of Disseminated Tuberculosis with Gradinego’s syndrome was made. Headache slowly responded to analgesics. Child continued on ATT along with steroids. After 04 months of follow up child is asymptomatic, Lt lateral rectus palsy has gradually improved (Fig.3), CXR is normal and Lt mastoidectomy is planned. Conclusion- The peculiarities highlighted in our case are twofold. One, TB meningitis presenting with Gredinego’s syndrome is not described in literature. However few case of tubercular cranial osteitis is reported leading to Gradenigo syndrome. Two, the development of intracranial tuberculomas during antimycobacterial therapy is rare and poses diagnostic and therapeutic challenge for clinicians. Fig1. Child presented with Lt Lat Rectus Palsy Fig2.CECT brain revealed tuberculoma in the floccules of Lt cerebellar hemisphere Fig3. Child after treatment and resolution of Lt Lat Rectus Palsy NEU/9 (P) CASE REPORT OF AML PRESENTING WITH BILATERAL PROPTOSIS AND CRANIAL NERVE PALSIES Jaikumar S. Patel , Manish Tiwari, Dr.Ashwini Kundalwal Room 313 New Pg Hostel, Srtr Medical College & Hospital, Ambajogai, Beed, Maharashtra Email: jay12_686@yahoo.co.in 10 year old FCh came to OPD with C/o 1. Bilateral proptosis with difficulty in closing eyes since three months. 2. Difficulty in swallowing & speech since 7 days . Patient went to private practitioner & diagnosed as a case of hyperthyroidism and given carbimazole. There was no relief , so patient came to our institute for second opinion .Clinical examination HR- 88/min, RR- 28/min, BP- 112/72 mm of hg.No lymphadenopathy / no bone tenderness /no petechaie/ no obvious thyroid swelling.there was bilateral proptosis with conjunctival congestion. Systemic examination: CNS there was palsy of vii, ix and x cranial nerves of left side which was lower motor neuron type. Rest of CNS and other systems were normal . No spleen or liver palpable. Investigations: 1. Patient already had done thyroid profile, T3 -- 84.2 ng/dl , T4 --18.4 mcg/dl,tsh -- 1.5 miu/ l, TPO abs.levels -30.25 u/ ml. These findings were not consistent with hyperthyroidism. So patient was investigated further CBC showed leucocyte count 6900/mm3,platelet count 92,000/mm3 haemoglobin was 9.2 g/dl.. 2. P.S and B SCAN findings were normal. 3. CT BRAIN with orbit revealed proptosis secondary to infiltration ? Cause. 4.Bone marrow examination done - altered M:E ratio secondary to myeloid hyperplasia. 60% blast cells of myeloid series,erythroid series decreased in number.Megakaryocytes decreased. This shows AML can present with proptosis and cranial nerve palsy without blast cells in blood. NEU/10 (P) GUILLAIN BARRE SYDROME WITH HYPERREFLEXIA: AN UNUSUAL PRESENTATION Barnali Mitra, Vinod Dagar, Shuvendu Roy, Daljit Singh Resident Pediatrics, Department of Pediatrics, Command Hospital, Pune E mail: 7barnali@gmail.com Introduction: Areflexia is the diagnostic hallmark for the diagnosis of Guillain Barre Syndrome. Presentation of this syndrome with hyperreflexia is very unusual. Case Report: A 6 years old boy was admitted with history of frequent falls while walking noticed by mother 10 days before admission. Over the next 2 days the child was unable to get up from squatting position, which progressively increased to inability to sit up from lying position and weakness of upper limbs. Neurological examination revealed normal higher mental status with intact cranial nerves function. On admission, there was generalized muscle weakness involving all four limbs and the truncal and neck muscles. All deep tendon reflexes were exaggerated and plantar response was bilaterally flexor. CSF study revealed classical albumino-cytological dissociation with WBC 01/hpf and proteins of 172 mg/dl. Nerve conduction study revealed low amplitude and low velocity conduction suggestive of acute demyelinating and axonal polyneuropathy, thus confirming the diagnosis of Guillain Barre Syndrome. The child was treated with Intravenous Immunoglobulin and showed remarkable improvement over next one month. Conclusion: Guillain-Barre syndrome is a postinfectious polyneuropathy involving mainly motor but sometimes sensory and autonomic nerves. It classically presents as ascending paralysis with areflexia. Reflexes are lost, usually early in the course. But in this case the reflexes were exaggerated till 2nd week of illness. This rare presentation revealed that hyperreflexia does not rule out the possibility of Guillain Barre Syndrome. NEU/11 (P) ALEXANDER DISEASE A DIAGNOSIS BY MRI Savita khadse, Arpan chauhan, Anjali kalbhande, Kailash patra. ESI- PGIMSR and Model Hospital, Andheri, Mumbai Email: drkailashcp@yahoo.co.in Abstract: Alexander disease is a rare, nonfamilial leukoencephalopathy that typically presents with frontal preponderance of white matter abnormalities and macro-encephaly. Patients with the infantile variant, the clinical symptomatology were dominated by failure of normal development, seizures, serious feeding problems, macrocephaly, and rapid neurologic deterioration. Case history: • We report a case of 6 years old male child born of nonconsanguineous marriage with progressive increasing head size and convulsions since 3 years of age and developmental delay, no history of perinatal insult, no contributory family history. On examination child was having macrocecephaly (HC-54cm) with spasticity of all 4 limbs. On investigation- fundus was normal.Neuroimaging was showing progressive white matter abnormalities with bilateral cerebral hemisheres(frontal>temporal>parital); subcortical cysts in bilateral frontal lobe, signal abnormalities and cystic changes in medulla , inferior cerebellar peduncle ,cerebral peduncle, exvacuo dilatation of ventricular system suggestive of atrophy. Discussion: • Alexander disease a neurodegenerative disorder was identified on basis of neurohistological criteria i. e. presence of dystrophic astrocytes containing intermediate filament aggregates (Rosenthal fibers) associated with myelin abnormalities.Different forms are identified: The infantile form (birth to 2 years)-have an early onset around 6 months and their prognosis is poor, symptomatology associates abnormal psychomotor development, progressive megalencepaly and/or hydrocephaly, a pyramidal syndrome, ataxia and epileptic seizures. The juvenile form-starts in school age around 9.5 years (15 months to 12 years) symptomatology consists mainly of spastic paraplegia and progressive bulbar signs, cognitive functions are usually spared. Adult formmost of patients have relapsing neurological symptoms suggestive of multiple sclerosis. Demonstration of Rosenthal fibers on histological examination is considered a prerequisite for a definitive diagnosis. A brain biopsy, which is an invasive procedure, is a diagnostic necessity, especially in cases of slow progression. The only other option is to wait for postmortem examination. • MR imaging is known for its high sensitivity and specificity in identifying white matter disorders (1,2). On the basis of these MR findings we defined five MR imaging criteria: • 1) extensive cerebral white matter abnormalities with a frontal preponderance, either in the extent of the white matter abnormalities, the degree of swelling, the degree of signal change, or the degree of tissue loss (white matter atrophy or cystic degeneration) • 2) Presence of a periventricular rim of decreased signal intensity on T2weighted images and elevated signal intensity on T1-weighted images. • 3) abnormalities of the basal ganglia and thalami, either in the form of elevated signal intensity and some swelling or of atrophy and elevated or decreased signal intensity on T2-weighted images • 4) brain stem abnormalities, in particular involving the midbrain and medulla; and • 5) contrast enhancement involving one or more of the following structures: ventricular lining, periventricular rim of tissue, white matter of the frontal lobes, optic chiasm, fornix, basal ganglia, thalamus, dentate nucleus, and brain stem structures • MRI shows anomalies of hemispheric white matter, sometimes cavitated which predominates in the frontal lobe. They are often associated with lesions in pontine nuclei, thalamus and cerebellum.(3). NEU/12 (P) A CASE OF MULTIPLE SCLEROSIS IN AN 8 YR OLD CHILD Mehndiratta S, Rajeshwari K, Dubey AP. Department of Pediatrics, Lok Nayak Hospital, New Delhi, India Email: drsmehndiratta@gmail.com; drsmehndiratta@rediffmail.com Introduction: Multiple sclerosis is a demylenating illness in childhood with a relapsing – remitting disease course. 3-18% cases of MS have onset < 18 yrs of age. Differentiation between ADEM and MS is sometimes difficult and challenging. Pediatric MS is usually reported in adolescent age group. We report a case in an 8 years old female child with this entity. Case Report: The patient presented with fever, headache and vomiting since 5 days that was being treated as meningitis elsewhere. There were associated complaints of progressive visual deficit since once month. This patient had left sided hemiparesis 1 yr back for which no treatment had been undertaken and the weakness resolved spontaneously to a large extent over the next few months. Ophthalmological examination revealed bilateral optic atrophy. VEP study showed bilateral extinguished waves. MRI of the brain and spine revealed a large area (measuring 4.8x 4.1x 1.7 cm) of altered signal intensity with internal septation appearing hyperintense on T2W and hypointense on T1W sequence, showing signal suppression on FLAIR, not showing significant enhancement on post contrast scans in the right frontal region. Multiple small T2 hyperintense foci perpendicular to the ventricular margin seen in the fronto-parietal region, corpus callosum and posterior limb of the internal capsule-features suggestive of Multiple sclerosis with a tumefactive plaque in the right frontal lobe. The patient was treated with Intravenous corticosteroids. The child is well on follow up for 7 months without any relapse. Discussion: The spectrum of demyelenating illnesses in the pediatric age group includes: Acute disseminated encephalomyelitis, multiple sclerosis, neuromyelitis optica and clinically isolated syndrome. Neuro-imaging plays a crucial role in diagnosis. Multiple sclerosis is multifactorial demyelinating illness of the central nervous system with interaction of genetic vulnerability and environmental exposure. The criteria for diagnosis of pediatric MS are: Two or more inflammatory CNS demyelinating events separated in time and space (The first event cannot be ADEM). The morbidity is significant, particularly within the first 2 years of the onset of the disease. MRI should demonstrate compatible features of CNS demyelination and exclude other causes for a diagnosis. Intrathecal demonstration of IgG oligoclonal bands have been found in over 90% cases. The preferred treatment is use of intravenous corticosteroids. IVIG can be used for non responders to steroid therapy. NEU/13 (P) TUBERCULAR VENTRICULITIS: A CASE REPORT OF AN UNRECOGNIZED ENTITY Suresh Kumar, Rakesh Kumar, B D Radotra, Meenu Singh Department of Pediatrics, Advanced Pediatric Centre (APC), Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. Email: sureshangurana@gmail.com Abstract: CNS tuberculosis in children commonly present as tubercular meningitis, hydrocephalus, and tuberculoma. However, there is limited literature regarding ventriculitis as a manifestation of CNS tuberculosis, its occurrence, pathophysiology, treatment, and prognosis. Here we report a 3-month-old infant with proven tubercular ventriculitis who also had disseminated tuberculosis. He presented with cough for 2 months with acute deterioration in form of fever, respiratory distress and seizures. His father was recently diagnosed to have sputum positive pulmonary tuberculosis. Examination revealed features of pneumonia, raised intracranial pressure and hepatosplenomegaly. Contrast CT of head showed communicating hydrocephalus with diffuse enhancement of basal meninges. Cerebrospinal fluid examination showed 400 cells/mm3 (80% lymphocytes); protein 119 mg% and glucose 24 mg% (with blood glucose of 84 mg%); negative gram stain, culture, Ziehl–Neelsen stain and culture for Mycobacterium tuberculosis; and ADA 31 unit/L. Treatment started with antitubercular therapy, steroids, antiepileptic drugs and external ventricular drain. On day 13 of admission he succumbed to the illness. Post-mortem examination revealed multiple caseating granulomas in liver, spleen, kidneys and lungs with AFB positivity. In brain multiple epitheloid granulomas were noted involving brain parenchyma and ependymal lining with AFB positivity. Few of ependymal tuberculomas had ruptured into ventricles. Tubercular ventriculitis occurs due to involvement of ependymal lining or choroid plexus in the process of inflammation or rupture of granulomas into ventricles. The treatment required is antitubercular therapy with CSF shunt, but it may be a marker of poor prognosis. NEU/14 (P) CLINICO-AETIOLOGICAL STUDY OF MENINGITIS IN CHILDREN INCLUDING NEONATES P Dowerah, Saikia, R.Sonowal. Dept. of Pediatrics, Assam Medical College, Dibrugarh. Email: ritzsnwl@gmail.com ACUTE BACTERAL Introduction: Acute bacterial meningitis being one of the most frequently encountered pediatric emergency with devastating consequences with a change in the aetiology and antibiotic sensitivity from time to time has felt the need for this study. Aims and objectives: To study the clinical profile of acute bacterial meningitis in children upto 12 years including neonates, to study the Cerebrospinal fluid findings along with bacteriological profile and antimicrobial sensitivity. Methods and materials: The study was done in the department of paediatrics of AMC in Dibrugarh.3-5ml of CSF sample was collected by lumbar puncture in all clinically suspected cases of bacterial meningitis. Those with CSF analysis suggestive of bacterial origin were included in the study and further evaluated. Results And Observations: Out of 59 cases of bacterial meningitis who met the inclusion criteria, 76.27% cases were below one year of age and neonates comprising a majority of cases(54.23%).Male: female ratio was 1.3:1.Seasonal variation in occurrence of the disease noted, maximum being during the period of September-January. Most frequent presenting features were fever (86.4%),convulsion(55.93%), refusal to feed(30.50%) and vomiting(35.59%).In infants, a bulging frontanelle was the most frequent clinical finding(54.25%).Neck rigidity and Kernig’s sign were seen in older children in 28.81% and 25.42% cases respectively. CSF pressure was high in 50.84% cases, CSF appearance varied from normal to purulent, maximum being hazy (44.06%).CSF protein ranged between 151-300mg/dl in 69.49% cases, CSF sugar ranged between 21-30mg/dl in 50.84% cases and CSF cell count ranged from 51500 cells/cubic millimetre in 86.44% cases. Gram staining of CSF revealed organisms in 30.5% cases and culture was positive in 33.89% cases. Staphylococcus aureus was the most predominant organism isolated(22.03%).E.Coli was isolated from 6.77% cases, Klebsiella pneumoniae from 3.38% cases and Streptococcus pneumoniae in 1.69% cases. Culture was negative in 66.10% cases. All gram positive isolates were 100% sensitive to Oxacillin, Vancomycin and Linezolid. All gram negative isolates were 100% sensitive to third generation cephalosporins and Amikacin. Mortality rate was found to be 5.08% and neurological sequelae was found in 4 cases. Conclusion: To decrease the mortality rate and neurological sequelae in cases of bacterial meningitis, causative organism and the antibiotic sensitivity is needed to be studied frequently. NEU/15 (P) CLINICO-EPIDEMIOLOGICAL CHARACTERISTICS AFFECTING THE HEALTH RELATED QUALITY OF LIFE IN CHILDREN WITH EPILEPSY: A CROSS SECTIONAL STUDY Vandana Arya, Virender Kumar Gehlawat, Jaya Shankar Kaushik, Geeta Gathwala Department of Pediatrics, Pt B D Sharma Postgraduate Institute of Medical Sciences, Rohtak, Haryana, India-124001 Email: jayashankarkaushik@gmail.com Abstract: Introduction: Epilepsy in children could significantly impact quality of life (QOL) in their physical, psychological, social and emotional domains of functioning. Aims and objectives: To assess the self reported quality of life (QOL) in children with epilepsy (CWE) and to assess the demographic and clinical factors which influence the QOL in CWE. Study design and setting: The study was a cross sectional study conducted in outpatient clinics of Department of Pediatrics at a tertiary care hospital of North India. Methods: Children aged 615 years with active epilepsy and who were receiving antiepileptic drugs in preceding 6 months were enrolled consecutively in the study. Children with comorbid neurodevelopment conditions and mental retardation were excluded from the study. The QOL was measured by QOLCE questionnaire, a 76 item parent-reported questionnaire. The questionnaire was translated into Hindi and the internal consistency of the subscales was determined using Cronbach's alpha. An overall QOL score was computed and the mean QOL scores were compared in children with clinical and demographic characteristics using appropriate statistical tests. Results: A total of 40 children were enrolled in the study with a mean (SD) age of 10.6 (2.7) years, of which 22 (55%) were males. Majority of the children belonged to lower [15(37.5%)] and middle [23(57.5%)] socioeconomic class, with 12 (30%) of the mothers and 8 (10%) of the fathers being illiterate. The most frequent seizure types were generalized tonic-clonic [27(67.5%)] and partial seizures [11(27.5%)]. Most of the patients had well controlled epilepsy [36(90%)] and were receiving monotherapy [39(97.5%)]. The mean (SD) overall QOL score among CWE was 66.7(4.8). The mean overall QOL scores were comparable by age (p=0.590), gender (p=0.646) and socioeconomic status (p=0.968). Similarly, the mean QOL scores were comparable by type of seizure (p=0.916), seizure frequency (p=0.756) and last seizure time (p=0.624). The mean QOL scores were better in the domains of social function, emotional wellbeing & cognition, but were impaired in the physical domains and behavioral function. Conclusion: The overall QOL was not affected by the demographic and disease characteristics including the type, frequency of seizure & duration of treatment. Children with active epilepsy had a more compromised QOL in behavioral functioning and physical domains. Hence QOL measures should be a part of periodic follow up in children with epilepsy. NEU/16 (P) CLINICAL PROFILE AND ELECTROENCEPHALOGRAPHIC CORRELATES IN CHILDREN WITH EPILEPSY: A CROSS SECTIONAL STUDY Vandana Arya, Rekha Bhavsar, Virender Kumar Gehlawat, Jaya Shankar Kaushik Department of Pediatrics, Pt B D Sharma Postgraduate Institute of Medical Sciences, Rohtak, Haryana, India-124001 Email: jayashankarkaushik@gmail.com Introduction: Epilepsy is defined as a condition in which seizures are triggered recurrently from within the brain and considered when two or more unprovoked seizures occur at an interval greater than 24 hours apart. Electroencephalogram (EEG) is the single, most valuable, safe and non-invasive laboratory test for evaluation of children with epilepsy. Objective: To determine demographic and clinical profile of children with epilepsy and to correlate with EEG findings. Study design and setting: Study was a cross sectional study conducted in the pediatric department of a tertiary care center. Study method: A total of 70 children aged 1m-12y presenting with first time diagnosed epileptic seizures were consecutively included. Children with co-morbid neurodevelopment conditions and mental retardation were excluded from the study. Demographic, clinical details, seizure characteristics and radiological investigations were recorded. EEG was performed by 20-20 electrode system. Results: Majority of children were in age group 1-5 year [34(48.6%)] with median age of 4 years. Of 70 enrolled children, 41(58.6%) were not on any antiepileptic drug (AED). Positive family history of epilepsy was present in 6 (8.6%). Examination revealed microcephaly in 7 (10%) and neurocutaneous markers were detected in 3 (4.2%). Type of epileptic seizures were generalized tonic-clonic [46(65.7%)], generalized tonic [7(10%)], myoclonic [2(2.8%)], infantile spasm [2(2.8%)], absence seizure [2(2.8%)] and complex partial seizure [10(14.3%)]. Abnormal neuroimaging was seen only in 12 (17.1%). EEG correlates of generalized epilepsy (n=46) were spike-polyspikes pattern suggestive of idiopathic generalized epilepsy in 33 (71.7%), normal in 13 (28.3%). Among children with complex partial seizure (n=10), EEG was normal in 2 patients, 3 were diagnosed with BCECTS and 5 had features of localization related epilepsy. The EEG findings supported the diagnosis of Cryptogenic West syndrome, Benign Rolandic Epilepsy, Petitmal Absence and Juvenile Myoclonic Epilepsy in 2 patients each. Conclusion: The present study highlights the clinical and electroencephalographic data of epileptic children which reemphasize the need of electroencephalography among children with epilepsy. NEU/17 (O) CLINICAL-EEG & RADIOLOGICAL PROFILE OF CHILDREN WITH FIRST EPISODE OF SEIZURES Suprita Kalra 7/3 Mandalay Lines, (Behind Mh Kirkee), Range Hills Kirkee, Pune-411020, Maharashtra Email: kalrasuprita@gmail.com Introduction- Retrospective analysis of clinical data, EEG findings & radiological data of children in age group beyond neontal period upto 12 yrs who reported to the emergency department with first episode of afebrile seizures in last one year. Aims & objectives-To analyse clinical profile,EEG & MRI Brain findings of these children. Materials & methods22 children, clinical profile including developmental milestones achieved appropriate for age ,school performance, details of type of seizure,its duration,presence of aura & post ictal neurological deficit.All children were subjected to conventional EEG recording & MRI Brain plain & contrast. Results -15 developmentally normal ,9 > 5 yrs of age with good scholastic performance,2 with poor school performance.6 had developmental delay with 4 with cerebral palsy. Table-1 summarizes details of seizure, EEG & MRI Brain Findings Type of seizure No Duration of Post ictal EEG Findings MRI with seizure Aur neurologica Brain type a l deficit of seizur e Generalized 6 5mins - Nil 2 Abnormal tonic clonic 1hr(mean spike & wave Abnormal 12 mins,SD pattern-4 & -3 2.1mins) normal - 2 Generalized 9 3mins-30 Nil 2 Abnormal Abnormal tonic mins(mean spike & wave -4 8 mins,SD pattern 1.8 mins) Absence seizure 2 Very Nil Nil 3Hz spike & normal brief,no of slow wave seizures 10discharge 20 Atonic seizure 1 5mins Nil Nil Abnormal normal spike & wave pattern Infantile 1 Very Nil Nil hypsarrhythmi Abnormal spasm(myocloni brief,no of a c seizure) spasms 810/episode Focal seizure 3 3mins2 1 had localization Abnormal 8mins(mea transient related -2 n 5.3 blindness epilepsy mins,SD 1.1 mins) Conclusions- Generalized seizures are the commonest & MRI Brain shows the findings of underlying disorder in these children & is normal in others. Focal seizures are associated with EEG & MRI indicating the focus NEU/18 (P) POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME – A CASE SERIES Mehak Bansal, Amita Mahajan, Vineet Bhushan Gupta, Anupam Sibal D-8 Gk Enclave-1, New Delhi Email: mehakbansal@yahoo.com Introduction: Posterior Reversible Encephalopathy syndrome (PRES) is a clinicoradiological entity with characteristic changes on neuroimaging and nonspecific symptoms comprising headache, altered sensorium, visual disturbances and seizures. PRES occurs in diverse settings such as bone marrow and solid organ transplantation, patients on chemotherapy and immunosuppressive therapy, renal diseases and hypertension. Early recognition of PRES and treatment of seizures and antihypertensive therapy leads to excellent neurological outcome. Aims and Objectives: To review the clinical and neuroimaging findings in patients with PRES. Materials and Methods: We retrospectively analysed records of children diagnosed with PRES at our centre between September 2011 to September 2012 and reviewed their clinical features, neuroimaging findings and outcome. Results: Six patients (aged 3-18years) with mean age of 9.3 years were diagnosed to have PRES. Clinical presentation included generalised seizures (50%), partial seizures (50%) and visual disturbances (66.7%), altered sensorium (33.3%). Of the six patients, three were patients of acute lymphoblastic leukaemia on induction chemotherapy, two patients were post liver transplant and one patient was post bone marrow transplant. Hypertension was found in 50%. Neuroimaging findings included hyper intensities in parieto-occipital region in all. Three of the six patients had involvement of the frontal and cerebellar areas. All cases were managed with antiepileptics and three required antihypertensives. All patients showed complete neurological recovery. Conclusions: PRES is a rare disorder in children and associated with vast array of conditions. Early diagnosis of PRES by radiological and clinical evaluation and prompt management is necessary to prevent central nervous system sequelae. NEU/19 (P) INTRACRANIAL TUBERCULOMA PRESENTING AS ISOLATED SIXTH NERVE PALSY- A CASE REPORT Parveen Mittal, Shinu Singla House no.37, Khalsa college colony, Near saket hospital, Patiala Email: shinusinglabnl@gmail.com; doc parveen@yahoo.co.in Introduction- In developing countries, tuberculomas may account for up to 40% of spaceoccupying intracranial masses. However, isolated brain stem tuberculomas are rare lesions and account for only 5% of all intracranial tuberculomas in endemic areas . These intracranial masses commonly present as oculomotor and other cranial nerve palsies, the one-and-a-half syndrome , unilateral saccadic paralysis , and other focal neurologic signs of brain stem involvement. We describe a case of isolated unilateral horizontal gaze palsy due to pontine tuberculoma in an immunocompetent patient. This report documents a rare entity in which gaze palsy was the only manifestation. Case report- A 12 year old female presented with inability to move her right eyeball laterally, and double vision on looking towards right side for one and half month duration .There was history of headache for the same duration and the child was keeping her head tilted toward left side. There was no history of fever, vomiting , seizure, diminution of vision , ptosis, deviation of angle of mouth, difficulty in swallowing or nasal regurgitation. There was no history of weakness or incoordination of limbs. Her general physical examination and systemic examination was normal. Her weight was 26 kg, height 150 cm, PR-80/m,RR-20/m ,Temp-980F.On CNS examination , patient`s higher mental function were normal .Cranial nerves were normal except right sixth cranial nerve. Patient was not able to move her right eye toward lateral side. There was no other neurological deficit. Motor system, sensory system and autonomic nervous system was normal. Her gait and tandem walking was normal. A presumptive diagnosis of isolated sixth nerve palsy was made. A hemogram showed an elevated erythrocyte sedimentation rate of 56 mm/h and a white blood count of 12,400 cells/mm3 with 55% lymphocytes. The Mantoux test was positive about 12 mm in size. Chest X- Ray was normal.2D MRI showed a discrete rounded lesion with perilesional edema in posterior aspect of pons in the midline .Rest of brain parenchyma showed no other focal lesion.(fig.1) Fig. 1 showing Pontine Tuberculoma Patient was diagnosed as case of Pontine Tuberculoma. Anti-tuberculous therapy was started with a combination of rifampicin 10 mg/kg per day, isoniazid 5 mg/kg per day, ethambutol 30 mg/kg per day, and pyrazinamide 25 mg/kg per day along with steroids 2mg/kg/day. After 7 days child started recovering and one month after treatment child showed marked improvement. Discussion: There have been only 2 case reports in the English literature of an isolated ocular motility abnormality as the only presenting feature of brain stem tuberculoma. In the first report , the patient presented with diplopia and abnormal eye movements and had a supranuclear gaze palsy together with reduced abduction of the left eye, which was responsible for diplopia. A postcontrast brain CT scan revealed multiple small areas of signal attenuation in the cerebrum and brain stem. The patient subsequently developed fever, seizures, and abnormal gait and eventually died despite anti-tuberculous therapy. Autopsy revealed multiple caseating granulomas in the liver, kidneys, adrenal glands, right ovary, lungs, and brain indicative of disseminated tuberculosis. In the second report , a 12-year-old girl developed a left gaze palsy associated with reduced adduction of the left eye, resulting in horizontal diplopia on right gaze consistent with an isolated one-and-a-half syndrome. Brain MRI revealed a lesion in the pons and midbrain with an intermediately enhancing signal rim surrounding the lesion. The chest x-ray was normal. A presumptive diagnosis of pontine tuberculoma was made, and anti-tuberculous therapy was continued for 18 months. Repeat brain MRI after 6 months of treatment revealed complete resolution of the lesion, and the patient made a complete clinical recovery. Intracranial tuberculomas occur most commonly in the cerebral and the cerebellar hemispheres, which have relatively profuse blood supplies. Our patient is remarkable in that, despite the apparent size of the tuberculoma on imaging, the only neurologic manifestation was horizontal gaze palsy. NEU/20 (P) PROGRESSIVE MULTIFOCAL LEUCOENCEPHALOPATHY IN A NON HIV INFECTED INFANT-A CASE REPORT Debashree Priyadarshini, Leena Das,N Mohanty Dept.of Paediatrics, SCB Medical College, Cuttack Email-drdebashreedas@gmail.com Background-Progressive multifocal leucoencephalopathy is a rare & usually fatal viral disease characterized by progressive damage or inflammation of white matter of brain at multiple locations caused by reactivation of JC virus.It usually occurs in severe immunodeficiency like AIDS,malignancies etc. There are only isolated case reports of PML in patients without apparent immunosuppression. Case-6 mon mch presented to our hospital with a 7 days h/o fever,convulsion,loose motion & respiratory distress.Patient was received in status epilepticus & had hepatomegaly(6 cm),splenomegaly(4cm) with anasarca on examination.On investigating the patient,TLC was high(18,200) with polymorphs constituting 70%,+ve CRP,staph.hemolyticus on blood c/s &CSF study showing 82 cells with 25%polymorphs.CSF PCR for viruses was negative.HIV screening of both parents &tubercular screening of the patient was negative.Despite treatment patient was deteriorating.MRI done subsequently showed multifocal nonenhancing white matter lesions without mass effect.JC virus could not be isolated due to lack of facilities. DiscussionAssymptomatic primary infection with jcv occurs in childhood(85% below 9 yrs),but the virus remains latent in kidney & lymphoid organs.Although only 5.6% of such cases have been reported so far,there is no definite treatment & the condition is usually fatal within 1 to 4 mon of diagnosis. Correspondence-Dr Debashree Priyadarshini PG Paediatrics, SCB Medical College,cuttack NEU/21 (P) INFANTILE TREMOR SYNDROME WITH SUBAORTIC VENTRICULAR SEPTAL DEFECT WITH SEIZURE DISORDER S Badarinath, A Kaur, PC Mishra C/O Sanjay Singh, room number 6, B block, Adelphi girls hostel, B-1, Bund road, opposite to Allahabad university library, Alllahabad 211002, India. Email: shruthibadarinath@gmail.com Abstract: Aim: To report a case of Infantile Tremor Syndrome(ITS) with Subaortic Ventricular Septal defect (VSD)with Seizure disorder. Introduction: Infantile Tremor Syndrome is a rare clinical syndrome of acute or gradual onset of mental and psychomotor changes, pigmentary disturbances of hair and skin, pallor, and tremor in malnourished children aged between 5 months and 3 years.Many factors have been found to be deficient in this syndrome.But other congenital defects or medical complication have not been reported in association with ITS.We report a case of ITS with Subaortic VSD with Seizure disorder. History: A 15 month old female child was admitted with complaints of continuous and generalized tremor involving all limbs and head for 6 days.Developmentally child had psychomotor regression.Child had 3 episodes of lower respiratory tract infection in the past which required hospital admission and had 3 episodes of generalised tonic clonic convulsions during hospital stay. Examination: Child had generalised tremor,pedal edema,grade 2 malnutrition pigmentary changes of hair and skin.Ausculatation revealed tachycardia and pansystolic murmur of grade 2/6. Investigation: Haemoglobin of 8 ,normocytic normochromic blood picture and normal levels of cobalamine, zinc and vitamin C were seen(as theories suggested that these deficiencies could be a causative factor).2D ECHO revealed Subaortic Ventricular Septal Defect(VSD).MRI brain revealed generalised diffuse cortical atrophy.Ultrasound abdomen revealed mild hepatomegaly.EEG was normal. Conclusion: Investigations did not reveal any nutritional deficiency.VSD could be an association or rarely a causative factor for ITS.There is insufficient scientific data to prove or disprove the above statement.Hence a rare association of Infantile Tremor Syndrome with Ventricular Septal defect and Seizure disorder was documented. NEU/22 (P) MOYAMOYA DISEASE-A CASE REPORT OF 21/2 YEARS OLD GIRL PRESENTED WITH STROKE Chaitali Patra, Malay Kr. Dasgupta Department of Pediatric Medicine, R. G. Kar Medical College & Hospital, Kolkata Email: baselinegame@gmail.com;chaitalipatra2009@gmail.com Abstract: Moyamoya disease (MMD) is a rare progressive cerebrovascular disorder of unknown etiology characterised by the narrowing or occlusion of major blood vessels to brain with particular involvement of the Circle of Willis and the arteries that feed it. It is characterised by the appearance on angiography of abnormal collateral vascular network adjacent to stenotic vessels (PUFF OF SMOKE).Its prevalence is 3.16/1lakh population only. MMD, though being a rare case in our part of the world, should be considered in the differential diagnosis of childhood stroke. We report here a case of 2 yrs 6 months old female child presenting with repeated episodes of seizures, vomiting followed by unconsciousness without any history of fever. After one day of conservative management, she got consciousness and there were right sided hemiparesis with right sided facial nerve palsy and aphasia. Initial neuroimaging study with noncontrast computed tomography scan revealed infarct at left fronto-empo-parietal lobe. MRangiography shows features suggestive of Moyamoya disease. She was treated with aspirin, LMWH and other supportive measures. After gradual improvement, she was referred to a higher centre for appropriate surgery with advice of oral aspirin and anti-epileptic drug. A high index of suspicion is required to diagnose MMD in children with stroke. MRangiography is the most definitive method of diagnosis. The cases which could not be diagnosed earlier can now be easily diagnosed and hence can be treated promptly in this modern era of neuroimaging. NEU/23 (P) ACUTE INTOXICATION WITH HYDROGEN PEROXIDE WITH AIR EMBOLI IN CENTRAL NERVOUS SYSTEM - A CASE REPORT Shivani Deswal,Pradeep Debata,Murtaza kamal,Madhu Garg Department of Pediatrics, Safdarjung hospital & V.M.M.C, New Delhi Email: shivanipaeds@gmail.com Hydrogen peroxide is a clear, colourless, odourless oxidizing agent found in concentrations ranging from 3% to 90% that is used in a number of household products and as a bleaching agent in industries. Ingestion results in morbidity through three main mechanisms: direct caustic injury, oxygen gas formation and lipid per oxidation. At standard temperature and pressure, household 3% H2O2 releases oxygen in the volumetric ratio of 1 ml 3% H2O2 to 10 ml oxygen gas. As a result, ingestions of small amounts of household (3%) H2O2 are generally benign but even a small amount of concentrated H2O2 can result in cerebral air gas embolism. A healthy six year old child presented to the emergency on ambulatory positive pressure ventilation with GCS of 3/15 following accidental ingestion of one fourth of a 500 ml unlabelled container of 35% hydrogen peroxide which was mistaken for water. By history, within 5 minutes after the ingestion, hematemesis was noted and the patient became unresponsive with circulatory collapse. The oral cavity and oropharynx were slightly erythematous and the abdominal examination revealed no distension & normal bowel sounds. The chest x-ray was normal. Brain Imaging could not be done .Blood workup was normal except for mild leukocytosis .ABG showed pH = 7.35, pO2 = 88 mm Hg, pCo2 = 38 mm Hg,HCO3 = 20 mmol/,BE = - 5 mmol/L ,Blood Sugar : 150mg% , S.Na-133meq/l,S.K-3.4 meq/l..CSF- normal. S.creatinine 0.8 mg/dl & B.urea 70 mg/dl.Child was put on mechanical ventilation for two days and expired of refractory shock .Post mortem report suggested diffuse brain infarction. Hydrogen peroxide has purported benefits ranging from HIV to cancer treatment.Thus is an emerging source for accidental poisonings. Management with hyperbaric treatment has theoretical benefit but has not been adequately studied. The absence of gas and cerebral infarction in CT scans does not exclude brain gas embolism. Gut decontamination is not indicated following ingestion, due to the rapid decomposition. Public awareness and regulation of the use of this substance is required. NEU/24 (P) RADIOIMAGING IN INFANTILE TREMOR SYNDROME JaswirSingh, ManpreetSodhi, Sanjeev Kumar Deptt. Of Pediatrics, Govt.Medical College / Rajindra Hospital Patiala – 147001 Email:bhagatsanjeev141@gmail.com Introduction:-Infantile tremor syndrome (ITS) is a disease of unknown etiology. Imaging of central nervous system (CNS) may reveal abnormalities in relevance to presentation. Aims& Objectives:-To observe radioimagical changes in CNS in ITS. Material& Methods:-The study included 7 children with ITS admitted to Deptt. Of Pediatrics, Government Medical College,Patiala.Age, sex, address, chief complaints were noted. Detailed general physical and systemic examination findings were noted. Hemogram along with peripheral blood film examination was done to know the type of anemia. Relevant investigations in the form of xrays, lumbar puncture were done wherever indicated. MRI scan of head was done in each case. Results: -Five (5) children were infants and 2 were above 1 year of age. The presentation in infants was between 8-10th months of age. Grade of malnutrition according to IAP was IIin 5 cases, one case was of grade I malnutrition and one was of grade IV malnutrition. All presented with tremors of tongue and hands. Four (4) had regression of mile stones. All except 2 had hyperpigmented knuckles. Five (5) children had dimorphic and 2 had microcytic hypochromic anemia, 3 had bronchopneumonia and 2 had meningitis. All except one had changes on MRI scan head.Five(5) had diffuse cerebral atrophy, 3 had small hypodensities in basal ganglia region. Only one had hyperintensity signals in left frontal region and periventricular white matter. Results: -Changes in CNS were observedin 86% of children with ITS. Diffuse cerebral atrophy was predominant finding. NEU/25 (P) FAHR’S DISEASE: A RARE SPORADIC CASE REPORT WITH IDIOPATHIC BASAL GANGLIA CALCIFICATION& SEIZURE S.K.Murmu,Priyabhasini Chinmoyee Ray,Praveen Nayak K From the Department of Pediatrics, VSS Medical College & Hospital, Burla, Sambalpur,Odisha Email: pcr.sony@gmail.com Abstract: Introduction: Fahr’s syndrome (or Fahr’s disease) involves progressive calcific deposition in the wall of blood vessels of the basal ganglia and dentate nuclei of the cerebellum in young and middle-age persons. It is occasionally associated with mental retardation and extrapyramidal symptoms. Clinically it may present with an array of movement disorders, dementia and other behavioural disturbances.The disease is often familial with autosomal dominant inheritance, but a few cases have been reported to have autosomal recessive inheritance and even sporadic cases have been reported in the literature. Case report: 14years male S.Nayakadmitted withabnormal dystonic movement for 5 days & GTCS of 2 episodes with history of similar episode multiple times in last two years with history of behavioral disturbance & poor school performance.There is no family history of similar complaint in any of family members.The patient also has gross delay in motor, language, social, fine motor mile stones. On examination patient was disoriented, with slurring of speech & dystonia. Vitals are stable. On CNS examination patient is having subnormal intelligence,hypertonia,with b/l plantar extensor & DTR exaggerated with Trousseau sign negative. His hematological profile (serum calcium, serum magnesium, serum phosphate,serum parathyroid, serum vitamin D2), renal function,liver function,urine routine and stool examination were normal. EEG showing abnormal epileptiform disorder & CT Scan showing B/L basal ganglia calcifications. NEU/26 (P) ETIOLOGY AND RADIOLOGICAL STUDY OF CHILDREN WITH STATUS EPILEPTICUS Rajniti Prasad, Sujoy Saha, O.P.Mishra Associate Professor, Department of paediatrics, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221005, India E-mail: rajnitip@gmail.com Introduction: Status epilepticus (SE) is a common neurological emergency in children and is life threatening with risk of neurological sequelae, thus it needs urgent management to prevent significant morbidity and mortality. Aims & Objectives: The present study was done to find out etiology, laboratory findings, imaging studies and short term outcomes in children admitted with status epilepticus. Material & Methods: One ninety three patients of status epilepticus above 1 month of age presented to pediatric emergency department were enrolled for this prospective hospital-based observational study. They were subdivided in to three group group-I(seizure controlled),group-II (seizure uncontrolled),and group-III(children who died). Complete blood count, serum bichemistry, ABG, CSF study, RFT and imaging of cranium were done in all patients. children were treated as per recommendation of Indian Academy of Paediatrics. Findings of the subjects were recorded in a pretested proforma and data was analysed by SPSS version.16. software. Results Out of 193 children (M:F-2.3:1), majority (38.3%) belonged to age group 61-180 months. Generalised tonic clonic seizure (85%) was most common. 46.1% children presented with history of more than four episodes of seizure. Random blood glucose is significantly high in group-III, where as total and ionised(p-value-0.034) calcium were low in group-III. There is also significant difference in pH(p-value-0.048)between group-I, and group-II. Most common etiology was meningoencephalitis, followed by seizure disorder. Status epilepticus in most of the patient(50.8%) was controlled by lorazepam with phenytoin. The duration of status epilepticus was significantly (p-value<.05) more in group-II, and group-III. The time take to control SE is more(p-value<.05) in group-II, and group-III. 9.84% patients had died. The most common neurological deficiency was cognitive deficiency. Conclusions: Etiology, duration of status SE and time taken to control is major detrimental factor of future outcome. NEU/27 A STUDY OF SEIZURE PROFILE IN INFANCY AND ITS OUTCOME IN 1YEAR FOLLOW UP IN A TERTIARY CARE CENTRE,SCBMCH,CTC Bichitrananda Raut, Rasmita Sahoo, Arati mallick Department Of Pediatrics, SCBMCH, CTC, Cuttack- 753007, Orissa Email: drbichitrarout@gmail.com; rasmita8301@gmail.com Introduction: Seizure is one of the most common neurological problem in children.children are more susceptible to seizure when they are infants,during which their brains are fast developing.In children incidence of seizure is around 10%.Most of them are provoked.<1/3rd of total seizure are due to unprovoked seizure,but its incidence in infancy is high.Earlier the incident worse is the prognosis. Objectives: 1. To reduce the incidence and complication of infantile seizures and modifying its impact on the child,his family and society. 2. Delineate the type of seizure,etiological profile,its management and neurodevlopmental outcome. Materials & Method: It’s a prospective study.All infants with unprovoked seizure are admitted to SCBMCH, CTC with in a month are examined by- 1. Comprehensive personal and family history 2. Clinical examination 3. Investigaions [CBC, CRP, EEG, NEUROIMAGING, csf study]. Then determination of etiology and management of each case.Then they are followed up for a period of 1yr.The neurodevelopmental outcome of each baby will be evaluated. Conclusion: Seizure profile in infancy of SCBMCH,CTC constitutesBirth asphyxia constitutes around 54% of total whose outcome is better if properly managed and followed up.Second most common is meningitis.TB meningitis in infancy has poor outcome in our set up.but in case of pyogenic meningitis only 1/3rd of patients developed neurodevelopmental deficit and rest lead a normal life.Infantile spasm and IEM have bad outcome. TUBEROUS SCLEROSIS if properly fallowed up and managed properly outcome is good.IVH has 100% neurodevelopmental seuele. NEU/28 (P) ALTERATION IN SERUM LIPID PROFILE ON DISCONTINUATION OF VALPROATE AND CARBAMAZEPINE THERAPY Anju Aggarwal, Deepika Harit, Swati Kalra, MMA Faridi, Neelam Chillar Department of Pediatrics, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India Email: aanju67@gmail.com Introduction: Carbamazepine and valproate therapy alter serum lipids and hence may be artherogenic. Aims and objectives:To compare serum lipids, apolipoprotein A and apolipoprotein B levels at discontinuation of antiepileptic therapy and 3 months later. Methods: Children 3-12 years who were seizure free for at least 2 yrs were recruited after written informed consent and ethical clearance. Fasting blood sample was collected before starting the tapering of AED and after 3 months of stopping the drug. Levels were determined by a standardised procedure on a autoanalyzer. Pre and post levels were compared using students “t” test. Results: Of the 45 children (17 males, 16 females) enrolled,33 were followed up till 3months after therapy(7 had repeat seizure during tapering,5 lost to follow up).They were receiving carbamazepine therapy (n=20) or valproate( n=13). Mean total cholesterol was 110.1+37.1md/dl before and 112.1+34.4 mg/dl after therapy(P=0.82).There was no significant difference in levels of LDL, VLDL and HDL( P>0.05), HDL and VLDL cholesterol increased and LDL remained same. Mean levels of ApoA and ApoB increased after stopping therapy and the difference was statistically significant for ApoB (P=0.03).The levels were not affected by age or sex of the child ( P>0.05) or the type of AED. Conclusions: Serum lipids are altered after discontinuation of AED therapy. Hence the artherogenic potential of antiepileptic drugs may not be long term. NEU/29 (P) STATUS EPILEPTICUS IN A CHILD WITH SANJAD SAKATI SYNDROME O.P.Mishra, Rajniti Prasad, Chhaya Kumari Department of Pediatrics, Institute of Medical sciences, Banaras Hindu University, Varanasi221005, India Email: rajnitip@gmail.com; opmpedia@yahoo.co.uk Abstract: Introduction: Sanjad Sakati syndrome (SSS), an autosomal recessive disorder is characterized by hypoparathyroidism, mental retardation, growth retardation and dysmorphic facial features. It is a rare cause of hypoparathyroidism and hypocalcemia, which leads to status epilepticus in children. Objective: To present a case report. Case report: A 6 yrs male born from consanguineous parent was brought in emergency with history of fever and multiple episodes of generalized tonic clonic seizures for 2 months and unconsciousness for 4 days. At admission, child was unconscious and had generalized tonic clonic seizure. In emergency, after securing airways, intravenous lorazepam was given followed by intravenous phenytoin(loading 20 mg/kg followed by 5 mg/kg bid) to control seizure. In past, child had similar episode 1 year back and treated by anti-tuberculous drug for tuberculous meningitis. Child had global developmental delay. He had dysmorphic facies(prominent forehead, deep seated eyes, beaked nose, long philtrum , thin lips, poor dentition) and increased tone in all limbs with exaggerated deep tendon reflexes and bilateral upgoing plantars. Other systemic examination was normal. ABG showed Ph:7.24, PaO2:62mm of Hg, PaCO2: 28 mm of Hg, HCO3-:14 meq/L and ionized calcium: 0.69 mol/L. CSF was normal. Computer tomography (CT) cranium showed bilateral basal ganglia calcification. MRI cranium showed mild cerebral atrophic changes with prominent ventricular system and B/L calcification of basal ganglia. Serum calcium and phosphate values were 5.8 mg/dl and 6.22mg/dl respectively. Based on report of investigations, hypoparathyroidism as cause of seizure was suspected and confirmed by serum parathyroid level (iPTH), which was <3 pg/dl (Normal: 25 to 75 pg/dl). Child was put on intravenous calcium initially for 72 hours, thereafter oral calcium. His consciousness and seizures got controlled with intravenous calcium gluconate. Subsequently child shifted on oral calcium and calcitriol and was discharged on same. Conclusion: We report a case of Sanjad Sakati Syndrome, which is not reported from India. NEU/30 (P) VALPROIC ACID ADMINISTERATION IN MANAGEMENT OF STATUS EPILEPTICUS CAUSING REYE’S SYNDROME Pooja Kamath, Sushma Save, Alpana Somale, Sandeep Bavdekar Department of Pediatrics, T. N Medical College, BYL Nair Hospital, Mumbai Email: drpoojakamath@gmail.com Introduction- Reye’s syndrome involves mitochondrial injury, which inhibits oxidative phosphorylation and fatty-acid beta-oxidation. Accumulation of high concentrations of ammonia leads to encephalopathy and anicteric hepatitis with 3- fold rise in liver enzymes. Here we report a rare case of Reye’s syndrome. Case Summary- A 2 year old female child underwent Modified Blalock Taussig shunt surgery for Tetrology of Fallots. Post-operatively patient developed Status epilepticus attributed to hypoxia. During Status epilepticus management ,she responded to second dose of Valproic acid. The child had poor Glasgow Coma Scale(E1M2V1), unequal pupils not reacting to light with retinal haemorrhages and developed features of shock. Lab investigations revealed thrombocytopenia and deranged liver function test (SGOT- 5489 IU/L, SGPT- 2496IU/L), INR- 1.5 while Sr bili (0.3 mg/dL), Sr Ammonia 1118 mg/dL, Hypoglycemia (D-stix low). Inspite of adequate treatment patient succumbed. Post- mortem liver biopsy showed fatty change suggestive of Reye’s syndrome. Discussion: Reye’s syndrome is a serious, biphasic condition of children and adolescents that is rarely seen today. The commonest drugs being salicylates but rarely valproic acid is also known to cause Reye’s syndrome. Studies have suggested that induction of the MPT(mitochondrial permeability transition) is a common pathophysiological mechanism. Several infectious agents have been correlated with it. The severity of can be classified with the clinical staging system. The diagnosis is of exclusion. A high index of suspicion with appropriate treatment strategy is to provide supportive care. Conclusion: It poses great challenge in management of Status epilepticus. Mortality being very high, one must use Valproic acid carefully in control of seizures & pick up early signs of reye’s syndrome & treat it vigorously. NEU/31 (O) COMPARISON OF INTRANASAL MIDAZOLAM WITH INTRAVENOUS DIAZEPAM FOR TREATING FEBRILE SEIZURES IN CHILDREN: PROSPECTIVE RANDOMISED STUDY Alok Kumar Meher, Nandini Naskar, Manas Ranjan Mallick, Niranjan Mohanty Dept. Of paediatrics, SCBMCH, Cuttack, Odisha. Email: alokrules29@gmail.com Objective: To compare the safety and efficacy of midazolam given intranasally with diazepam given intravenously in the treatment of children with prolonged febrile seizures. Design: Prospective randomised study. Setting Paediatric emergency department in SCB medical college, cuttack,odisha. Subjects 40 children aged six months to five years with prolonged febrile seizure (at least 10 minutes) during a 12 month period. Interventions Intranasal midazolam (0.2 mg/kg) and intravenous diazepam (0.3 mg/kg). Main outcome measures Time from arrival at hospital to starting treatment and cessation of seizures. Results Intranasal midazolam and intravenous diazepam were equally effective. Overall, 18 of 20 seizures were controlled with midazolam and 17 out of 20 with diazepam. The mean time from arrival at hospital to starting treatment was significantly shorter in the midazolam group 3.6 minutes, than the diazepam group 5.5 minutes. The mean time to control of seizures was significantly sooner 6.8 minutes in the midazolam group than the diazepam group 8.0 minutes No significant side effects were observed in either group. Conclusion Seizures were controlled more quickly with intravenous diazepam than with intranasal midazolam, although midazolam was as safe and effective as diazepam. The overall time to cessation of seizures after arrival at hospital was faster with intranasal midazolam than with intravenous diazepam. The intranasal route can possibly be used not only in medical centres but in general practice and, with appropriate instructions, by families of children with recurrent febrile seizures at home. NEU/32 (P) BROWN-VIALETTO-VAN LAERE SYNDROME Udani.V.P , Somasekharan.R, Sharma.B 69 Al Jebreya Court, Marine Drive, Mumbai - 400020, Maharashtra Email: bharti2000.2008@rediffmail.com Abstract:- The Brown-Vialetto-Van Laere syndrome (BVVL) is a rare neurological disorder characterized by progressive pontobulbar palsy associated with sensorineural deafness. Other features include respiratory compromise, limb weakness, slurring of speech, facial weakness, and neck and shoulder weakness. The female to male ratio is approximately 3:1.Approximately 50% of cases are familial (autosomal recessive). The remaining cases are sporadic. The diagnosis is usually clinical. We here present a case of 6 year old girl 1st by birth order, born of 3rd degree consanguinous marriage who came with complaint of ptosis of left eye , slurred speech, hypophoniaand laboured breathing since 2 months. Her younger brother had similar complaints 3 months back and he died 1 week back.On examination her vitals were stable but respiratory rate was >40/min with subcostal retractions.On CNS examination ptosis of left eye with mask like facies , poor gag reflex; no response to sound; uvula central ;no tongue fasiculations; no upper limb and lower limb weakness with normal reflexes.On investigation CBC , S.E ,CSF study were normal. Anti-Ach-receptor antibody was negative; EMG and NCV revealed bilateral 7th nerve palsy; MRI brain normal. Paediatric neurologist opinion was taken and BERA test was done which revealed bilateral sensorineural deafness and hence diagnosis of BVVL was made. Patient was treated symptomatically; was on ventilatory support for 1 week and NGT feeds and was started on riboflavin and riluzole.presently she is showing signs of simprovement. NEU/33 (O) ETIOLOGY AND OUTCOME OF FIRST EPISODE OF AFEBRILE SIEZURE IN CHILDREN Vijay Kamale, Nitin Kadam, Varun Kasliwal Dept. Of Paediatrics, MGM Medical College Hospital, Sector 4e, Kalamboli-410209. Email – drvijaynkamale@yahoo.co.in Introduction: Acute Seizure is a common pediatric emergency.Acute asymptamatic seizures are caused by infection, head trauma, electrolyte imbalance, space occupying lesion, etc. Febrile seizure is special category. Epilepsy, febrile seizures and CNS infections are well studied, but afebrile seizures are not studied well. Aims And Objectives: A study was carried out in tertiary care medical college, Hospital to find out etiology, outcome OF AFEBRILE seizure. Afebrile seizures was defined as first episode of seizure which was not associated with fever and not having any obvious symptomatic cause on history. The Age group was 1 Month -12years to rule out neonatal seizure. Material And Methods: The detailed history, neurological examination and relevant investigations including metabolic workup and neuroimaging was done. Total 329 children with 1st seizure episode from January 2010 to December 2011 were evaluated, out of which 46 children fulfilled the above mentioned criteria. Results: The etiology of seizure was hypoglycemia in 12 / 46 (26.09%), hypocalcemia in 10 / 46 (21.74%), tuberculoma in 12 / 46 (26.09%), hyponatremia in 6 / 46 (8.70%) and neurocysticercosis, cerebral malformation and drug over dose in 2 / 46 (4.35%) case each. Out of 46, two children died, two had neurodeficit and other 44 recovered completely. Idro et al have studied incidence etiology and out come of seizures in malaria endemic Kenyan 900 children, in 2008. They found hypoglycemia and hyponatramia as common causes. Conclusion: Afebrile seizures are commonly associated with metabolic causes. The tuberculomas although infectious etiology is not associated with fever and is important cause of afebrile seizure. Thus tuberculoma as important cause of afebrile seizures should always be considered. NEU/34 (O) NUTRITIONAL STATUS OF CHILDREN WITH CEREBRAL PALSY M.K. Behera., Sarang Digambar Waghmare, S Haribhakat, M Patil Dept of Paediatrics , SKN Medical College & hospital Pune Email: manaskumarbehera@yahoo.co.in; manasbehera1952@gmail.com Introduction: Cerebral palsy is a common chronic neurological disorder in children. C P children are more vulnerable to malnutrition not because of their physical handicap but for other factors like familial neglect, economical stress and psychosocial stigma. Aims & Objectives: 1 To study the nutritional status (Wt / Ht indices) of children with Cerebral palsy and Compare with latest WHO norms.and 2 To Co-relate it with socio-economic status. Material &Methods: A cross sectional observational study was conducted in SKN Medical College and General Hospital during April- June 2012. Cerebral palsy children up to 05 yrs were studied. Weight, height and length were measured by electronic weighing scale, stadiometer, infantometer and by means of flexible tap respectively. Results: Total 50 children with Cerebral palsy aged 5 month to 5 years were studied. Mean age 3 years, male: female 31:19. Spastic CP- 45 (90%) and 2 each (8%) hypotonic, Dyskinetic and 1(2%) of mixed variety. In the spastic CP Quadriplegia 23(46%), Diplegia 13 (26%), Paraplegia 6 (12%) and hemiplegia and monoplegia each were 4(14%). Majority of parent (86.66%) are of low socioeconomic status .In this study 36(72%) were malnourished of which SAM -23 (63.88%) and MAM -13 (36.11%). Stunting was observed in 30(60%) of cases. SAM is mostly associated with spastic variety of CP. 60 % of Children had clinical evidence of vitamin deficiency. Malnutrition was more in lower socio-economic status. Conclusion: Malnutrition was detected in 72% of cerebral palsy children and more in lower socioeconomic status. Parents of CP children should be more concern about the nutritional status of their children and supplement adequate nutrition to prevent the morbidity and mortality. NEU/35 (O) ACUTE DISSEMINATED ENCEPHALOMYELITIS (ADEM) – A CLINICAL AND NEURORADIOLOGICAL PROFILE OF PEDIATRIC PATIENTS Partha Pratim Halder, Prabhas Prasun Giri, Apurba Ghosh, Dipankar Das, Swapan Mukhopadhaya Institute Of Child Health, Kolkata Email: dr.prabhas@yahoo.co.in Introduction-Typically ADEM is an acute monophasic immune mediated demyelinating disorder involving brain and/or spinal cord following vaccination or infection. Evidence of prodromal illness or vaccination followed by clinical features of encephalopathy along with MRI findings of demyelination, these 3 are typical triad of ADEM. Though a life threatening disease, early diagnosis and prompt treatment accounts for a very good survival. Here we present a prospective study about the varied presenting features of ADEM with neuroimaging findings we observed in our institute for the last 3 years. Aims & Objectives- To discuss the clinical and neuroradiological profile of pediatric patients with ADEM. Patients & MethodsClinical records of children fulfilling the diagnostic criteria of ADEM admitted at the Institute of Child Health, Kolkata during the time period of July 2009 to July 2012 were reviewed . The diagnosis of ADEM was based on the typical clinical findings supplemented with relevant laboratory investigations and exclusion of other diseases. The data collected included details of clinical and laboratory features, treatment and outcome and MRI findings. Total no of patients were 30, mean age of presentation was 5.86 years. Rersults- around 60% of patients had the h/o either viral prodrome or vaccination. Fever at the time of onset was present in 40% of cases. Neurodeficit was almost universal, presented in 93% of cases.In the investigations, 40% patients revealed pleocytosis in their CSF while all of them presented with features of demyelination in MRI. The demyelination was asymmetrical in around 67% of cases, but symmetrical in 27% of cases. Most of the patients were treated with IV Methylprednisolone (30/mg/kg/day ) for 3 to 5 days followed by oral prednisolone. There was complete recovery in 80% cases and the mortality being only 7%. Conclusion- ADEM is not so uncommon as thought previously. Wide availability of good MR imaging with a strong clinical suspicion makes diagnosis early and leads to improved survival. NEU/36 (P) ASSOCIATION OF HYPOMELANOTIC DISORDER WITH AUTISM: CASE SERIES Shah Vivek, Torkadi Rushita, Bavdekar Sandeep, Save Sushma, Kondekar Alpana. Neurology OPD, Pediatric Department, T.N. Medical College, BYL Hospital, Mumbai Email: drvivekshah@gmail.com Introduction- Association of hypomelanotic skin disorders with autism is rare. Hypomelanotic skin disorders occur in about 10% of patients with autism. Autism occurs in 1-60% patients with hypomelanotic skin disorders. Materials and Methods- From September 2008 –September 2012 total 375 cases with autism spectrum were screened and diagnosed. Of which 6 patients were associated with autism; 2 of them are of Tuberous sclerosis, 2 are of Hypomelanosis of Ito, 1 is of Angelman syndrome and 1 is of Oculocutaneous Albinism. Discussion- Association of hypomelanotic skin disorders with autism may be due to fact that genes of these have chromosomal loci that lie near the loci for genes of autism. A major gene for most of them is on chromosome 15. Cytogenetics has shown that variation in Chromosome 15q24, 11p12-p13 are associated with Autism. Chromosome 15 is dysfunctional in Oculocutaneous albinism & deleted in Angelman syndrome. Contiguous to this is a cluster of genes-GABRA5, GABRB3 and GABRG3 that code for receptors of GABA .Allelic variants of these GABA receptor genes have increased risk of autism. This association is also due to dysfunctional migration of ectodermal and mesodermal cell precursors during embryogenesis leading to neuro-developmental problems like autism. Conclusion- Hypomelanotic cutaneous lesions may be the earliest manifestation of a child with autism. Autistic children should be screened for hypomelanotic skin lesions & subsequently for the associated disorders for early diagnosis & timely intervention. NEU/37 (O) CEREBRAL PALSY- A GLOBAL CONCERN..WHAT CAUSES IT ? AND HOW CAN IT BE PREVENTED? Anil Kumar.K.H, Sanjay.K.S, Basavaraja.G.V, Rajeshwari Indira Gandhi Institute of Child Health, Bangalore - 560029 Email: dranil.paed@gmail.com Introduction:The developmental disabilities are a group of disorders differentiated by the pattern of delay among developmental streams. Motor function abnormalities are a key feature. It is a most common developmental disorder of children first described by William little in the 1861. Since then the global prevalence been almost same. Aims and Objectives: To study the modifiable/preventable etiologies of Cerebral palsy. Materials and methods: 100 cases of Cerebral Palsy were studied over duration of one year in Neurodevelopmental clinic of Indira Gandhi Institute of Child Health, Bangalore. Results: 100 cases of Cerebral palsy studied over a period of 1 year with thorough clinical and necessary investigations revealed a pattern of etiological profile as Prematurity – 15%, Perinatal asphyxia – 43%, Malformation – 16%, Intracranial bleed – 6%, Post –meningo- encephalitis – 8%, Post-TBM – 2%, TORCH infections – 2%, Cortical vein thrombosis – 1%, Neonatal sepsis -3%, Idiopathic – 4%. The scenario/pattern is much different from that of Developed countries with wide scope for improvement in obstetric and perinatal care. Conclusion: Considering above mentioned etiologies or risk factors it is clear that about 50-60% of the them are preventable/modifiable with improved obstetric and perinatal care with timely interventions. And warrants the same in order to reduce the glaring morbidity and possible health care costs and psychosocial problems arising out of it. NEU/38 (P) ISOLATED NEUROSARCOIDOSIS NEUROTUBERCULOSIS Jhancy, Sowmya, Rohit, Anusha, M.S.Raju Rangaraya Medical College, Kakinada, A.P Email:jhansimalay@yahoo.com MISDIAGNOSED AS A 11 year female child admitted on referal in our ward 10 days ago with headache,vomiting and fever. with no other focal neurological signs. Her csf was normal, mantouex test positive, MRI brain showed multiple subependymal nodules in left lateral ventricle, foramen of manro and 3rd ventricle. Florid enhancement of the cisternal space, tentorium sellar,ventricular margins, around the cervicomedullary cord. Sellar region enlarged with increased enhancement along the stalk and hypothalamus. Child was on ATT since 9 months for similar complaint. Previous MRI showed similar findings, no other systemic manifestations were found. Diagnosed as rare possibility of neurosarcoidosis and sent for biopsy. Discussion: Child hood sarcoidosis is a very rare disease with 0.29 per 100000 incidence1 and differ in presentation than in adults. Juvenile sarcoidosis may present as early as 4 years of age. The clinical manifestations depend on organ involvement. There were 29 cases of childhood neurosarcoid were reported . Seizures were the most common presenting symptom (38% of subjects, 11 of 29).Twenty-one percent(6 of 29) had cranial nerve findings, Twentyone percent(6 of 29) had cranial nerve findings Five children presented with headache,as in our case, 4 with motor signs, and 3 with papilledema2..The diagnosis of neurosarcoidosis may be difficult and could be confused with infection (such tuberculosis or mycosis), with inflammatory diseases (such multiple sclerosis) or with neoplasm3.noncaseous granuloma on Biopsy is confirmatory. Steroids for prolonged period is the main stay of treatment. Relapses may occur. Sequential MRI is useful mean for follow up. NEU/39 (O) A STUDY OF SKELETAL MATURATION AND MINERALISATION OF CHILDREN WITH SPASTIC QUADRIPLEGIA S. Sitaraman, Indar Kumar Sharawat Sector 4-91 Jawaharnagar, Jaipur 302004, Rajasthan E.mail: drsraman.jp@gmail.com Abstract: Objectives: Diminished bone mineral density and delayed skeletal maturation are common in children with spastic quadriplegia. The purpose of this study was to provide a detailed evaluation of bone mineral density (BMD) and metabolism in this population and to assess the relationship of these measures to multiple other clinical, growth, and nutrition variables. Study design: This was hospital based, cross sectional, case-control study. Methods: 42 (28 males, 14 females) children with spastic quadriplegia and 42 (24 males, 18 females) healthy children were included in the study. Bone mineral density values of patient and control subjects were measured by dual energy absorptiometry (DXA). Left hand and wrist radiographs of all patients and right hand and wrist radiographs of controls were taken, and bone ages of all radiographs were determined. Results: In both male and female spastic quadriplegics, bone mineral density values of upper extremity, lower extremity, thoracolumbar spine and pelvis were lower than those of controls ( p <0.0001 ). Bone age was lower than chronological age in 75% cases withnon severe malnutrition and in 100% cases with severe malnutrition. In stepwise regression analyses, it was found that nutritional status independently contributes to lower bone mineral density values. Physical therapy and use of anticonvulsant drugs did not correlate significantly with bone mineral density values. Conclusions: Low BMD and delayed bone age is prevalent in children with spastic quadriplegia. The underlying pathophysiology is complex, with other multiple factors; nutritional status is the important factor contributing to the problem.Key words: Spastic quadriplegia, bone mineral density, skeletal maturation, nutritional status. NEU/40 (O) QUALITATIVE STUDY OF PYSCHOSOCIAL PROBLEMS AMONG MOTHERS OF CHILDREN WITH CEREBRAL PALSY ATTENDING TWO TERTIARY CARE HOSPITALS IN WESTERN INDIA SM Nimbalkar, Shyamsundar Raithatha, Rutwij Shah, Dhara Antani Department of Pediatrics, Pramukhswami Medical College and Shree Krishna Hospital, Karamsad, Dist: Anand, PIN: 388325, Gujarat E mail: somu_somu@yahoo.com Background and aims: The parents of children with cerebral palsy face several problems in meeting the physical, psychological and social requirements of their children. We explored the psychosocial problems faced by the mothers of children with cerebral palsy in rural and urban settings and compared the same. Methods: Qualitative research design through Focus Group Discussions (FGDs) was utilized. Two FGDs were conducted – one each at a rural and an urban tertiary level care hospital involving eight and six mothers respectively. Ethical clearance was obtained from institutional Human Research Ethics Committee. The FGDs were conducted by a moderator using an FGD guide and were video recorded. Transcripts were prepared from the video recordings and were analyzed qualitatively. Results: The problems experienced by the mothers were associated with common themes such as – Disturbed social relationships, Physical problems, Moments of Happiness, Worries about future, Need for a special school, Requirement of a support group, Lack of adequate number of trained physiotherapists and Lack of government support. All the parents had children with problems since birth and most had gone to various health care providers for a cure for their child. The participants in the FGD undertaken at the urban based hospital appeared to be poorly adjusted to the problem of the child as compared to the participants in the rural based hospital. Conclusions: Current pyscho-social status of the parents should always be considered. Program planners, Hospital administrators and health care providers need to be sensitized about the perceived need of this vulnerable population. NEU/41 (P) JUVENILE PILOCYTIC ASTROCYTOMA - TUBERCULOMA DELAYING DIAGNOSIS Nakul Kothari, Vikram Patra, N. Revathi, Bageshree Seth, Vivasvan Parekh, Parul Khanduja, Mitul Y Jasani Department of Pediatrics, M.G.M hospital, Kalamboli, New Bombay Email: nakulkothari@gmail.com Intracranial SOLs in children are often considered to be tuberculoma due to high incidence of tuberculosis in india. Of all the SOLs reported, 46.4% are tuberculomas. Brain tumours are often inappropriately labelled as tuberculoma without detailed investigation, thus causing a delay in diagnosis. CNS tumors are the second most common malignancy in childhood. Of all the different types, pilocytic astrocytomas & medulloblastoma are the most common tumours in childhood. Juvenile pilocytic astrocytoma is a cerebellar neoplasm that occurs 2:100000. Most affected are children aged 5-14yrs. But we often miss the clinical features, as this child was misdiagnosed as Tuberculoma & started on AKT. A 13 yr old female child presented with fever, non-projectile vomiting, headache, unsteady gait & neck pain of 1 day. She was developmentally normal & had no recent deterioration in scholastic performance. She was started on AKT 4 mnths back i/v/o neck stiffness & positive mantoux test. No neuro-imaging was done. On examination, she had pappiledema in right eye. Spino-motor examination was normal. However She had cerebellar & meningeal signs. Routine investigations & CSF study were inconclusive. CT scan revealed a large cystic SOL in lt cerebellar hemisphere & vermis, compressing 3rd & 4th ventricle with periventricular ooze suggestive of Juvenile pilocytic astrocytoma. Such delay in diagnosis can lead to complications further worsening the condition of child. Child got operated & histolopathological confirmed the diagnosis of JPA. NEU/42 (P) RETROSPECTIVE ANALYSIS OF CASES OF ACUTE FLACCID PARALYSIS FROM A TERTIARY CENTRE IN BANGALORE Smitha, Basavaraja, Shivananda, Indira Gandhi Institute Of Child Health, Bangalore Email: drsmithavasu@gmail.com Abstract: We are presenting the results of a retrospective study of cases of Acute flaccid Paralysis at Indira Gandhi Institute of Child Health – tertiary care centre in Bangalore. Study was conducted between Jan 2010 – June 2012. We encountered 30 cases of acute flaccid paralysis during the study period. Most common etiology causing acute flaccid paralysis was found to be Guillian Barre Syndrome followed by transverse myelitis and non polio entero virus infection (NPEV). Guillian Barre syndrome accounted for 80% of cases. A sudden surge in cases was noticed between Jan 2012 to June 2012 which accounted for 53% of total cases. Intensive care was required in 24 cases [80%] of which 7 [23%] patients required ventilation, 2 patients expired during stay in the hospital accounting for 6% mortality. Key words: Acute flaccid paralysis, Guillian Barre Syndrome, Tranverse Myelitis, NPEV NEU/43 (P) CLINICO-EPIDEMIOLOGICAL STUDY OF ACUTE FLACCID PARALYSIS AT BPKIHS, DHARAN, NEPAL Singh R R, Chaudhary S, Bhatta NK, Khanal B, Bhandari R. Professor of Pediatrics, BPKIHS, Dharan, Nepal Email: profrupasingh@yahoo.co.in Abstract: Introduction: Acute flaccid paralysis (AFP) is a clinical syndrome characterized by rapid onset of weakness, including (less frequently) weakness of the muscles of respiration and swallowing, progressing to maximum severity within several days to weeks. There are many conditions leading to AFP. Methodology: Prospective hospital-based study was carried out to find out the clinico-epidemiological features of AFP and its associated co-morbidities. All cases fulfilling the AFP case definition criteria were included. Cases were reviewed for full medical history and examinations. The necessary investigations were carried out and required treatment given. Regular follow-ups were done and final classification was made with the help of AFP surveillance team. Results: Forty-three children were included in the study out of which 18 expired and 25 completed the 60-day follow-up. Fever, altered sensorium and convulsions were present in 79.1%, 65.1% and 58.1% respectively along with weakness. Preceding viral illness was present in 9.3%. The mean Glasgow Coma Scale was 9.53±4.27 with a significant difference in the mean GCS of expired and surviving groups of children (p=0.02). Thirty-nine percent of children with AFP required intubation out of which 33% expired (p value=0.001). Higher temperature and lower respiratory rate were associated with poor prognosis (p =0.025 and 0.049 respectively). The final classification showed 53.5% Acute Encephalitis Syndrome (AES), 9.3% GBS, 9.3% dyselectrolytemia, 9.3%, peripheral neuritis, 7% Non-polio enterovirus, and 11.6% others. Conclusion: The commonest cause of AFP was AES. Poor GCS is an indicator of poor prognosis NEU/44 (P) LARGE CONGENITAL FRONTOPARIETAL ARACHNOID CYST-A RARITY Kamath Sowmini P, Baliga B S, Ballal C K,, P S Sangeethadevi, Prasad Rahul U Kasturba Medical College, Mangalore, Manipal University. Email: kamathsowmini@yahoo.com Abstract: Background: Arachnoid cysts are congenital, cerebrospinal fluid (CSF)-filled, intraarachnoidal lesions commonly picked up incidentally. We are reporting this unusual case since the cyst was large with frontoparital location. Case report: Three month old male baby presented to us with progressive increase in head size since birth. Convulsions at 3 months controlled with phenytoin.Birth history uneventful. Development age appropriate. On examination, Head circumference (HC) -44.5 cm (above 95th centile), anterior fontanelle – 2x3cm at level, posterior fontanelle closed .No prominent and dilated veins over the forehead. Sunset sign was absent. No neurologic deficits. MRI brain was suggestive of large cystic lesion (13.3 x 18.8 x 7 cm) which is hypointense on T1W1 and FLAIR, hyperintense on T2W1 in the extraaxial space in the left frontoparietal region and midline anteriosuperiorly, projecting downwards causing mass effect on adjacent brain parenchyma. The frontal horn of lateral ventricle is splayed due to mass effect with subfalcine herniation of right side of 22 mm size. There is atrophy of left frontoparietal lobe. - Possibility of arachnoid cyst was entertained. After documenting a normal CSFanalysis, Cysto-peritoneal shunt surgery was performed. At discharge the HC-44 cms and requires further follow-up. Conclusions: It is rare to have no neurological deficits with normal development despite the presence of large frontoparietal arachnoid cyst, with mass effect NEU/45 (P) DIAGNOSTIC YIELD OF CT BRAIN IN PEDIATRICS AT TERTIARY CARE CENTER S.S.Wagh, Uday Rajput, Nikhil Kadam, Satish Ashtekar Government medical college, Miraj Email: nikhildkadam86@yahoo.in Introduction: CT brain plays important role diagnosis of brain disorders in children.But inadvertent use of CT scan for many unindicated CNS disorders lead to decreased effectiveness of neuroimaging.this study is planned to find out the usefulness of CT scan in diagnosing various CNS disorders. Aims And Objectives: To find out usefulness of CT Scan Brain in diagnosis of various CNS disorders. Material And Methods: Present study done at tertiary care center over the period of 2 years CT specification: Inclusion criteria:all patients having CNS dysfunction,those having focal signs and whenever indicated by clinical evaluation. Exclusion criteria:patients having existing CNS disorder or those who have undergone previous neuroimaging. Statistical Method Used-Observations Drawn. Results: Baseline characteristics measured are Out of 40 cases, 52.5 % were between 0-5 years, 42.5% between 6-10 years and 5% were above 11 years. It is also observed that 65% were males. Primary outcome- In this present study includes 14(35%) cases of CNS infections, 9(22.5%) cases of Space Occupying lesions,4(10%) Congenital/Developmental defects, 4(10%) cases were Cerebrovascular diseases, 3 (7.5%) cases of Neurocutaneous syndrome, 1 (2.5%) case of Neurodegenerative disease and 5(12.5%) cases of Head injury. Conclusions: ● CT brain is useful for diagnosis of various paediatric CNS disorder.It is most efficacious in diagnosing CNS infections.Tubercular meningitis is the most common diagnosis found in this study NEU/46 (P) RHEUMATIC CHOREA: OUR OLD ENEMY IS STILL ALIVE Subhodh Shetty Department of Pediatrics, Kasturba Medical College, Mangalore, India Email: pedsshetty@gmail.com Abstract: Sydenham chorea (SC) is neurological manifestation of rheumatic fever and most common acquired chorea in children. It presents as choreiform movements and behavioral changes following streptoccocal throat infection. Although incidence of SC has diminished because of aggressive antibiotic treatment, isolated cases and epidemics persist, necessitating emergency physicians to be familiar with the disease Children with Sydenham's chorea and PANDAS (Pediatric autoimmune neuropsychiatric disorders associated with streptococcal throat infections) share an array of neuropsychiatric symptoms and distinguishing one from the other, especially at onset can prove challenging. It is importantto distinguish between these post-streptococcal disorders since their response to therapy differs. Children with SC require long-term benzathine penicillin prophylaxis to reduce risk of rheumatic heart disease. The efficacy of penicillin prophylaxis in preventing tic or obsessive-compulsive symptom exacerbations in children with PANDAS remains doubtful. We describe case of 9-year-old girl with SC. Pathophysiology, clinical presentation and management of SC was discussed NEU/47(P) GLUTARIC ACIDURIA TYPE 1 Ashok Rathod, Spoorthi Jagadish, Rohit Narvekar Prof Of Pediatrics, Bldg # 1, Flat # 15, Sir JJ Hospital Campus, Byculla Mumbai-400008, Maharashtra Email: spoojagadish@gmail.com GA 1 is a rare autosomal recessive organic aciduria, with incidence of 1in 40,000. The gene involved is GCDH on chromosome 19p13.2. It presents in infancy due to deficiency of glutaryl-coenzyme A dehydrogenase. Body is unable to break down lysine, hydroxy lysine and tryptophan.Macrocephaly is common.They appear normal, then suffer acute metabolic crisis at 6-18 months with recurrent episodes of ketosis, vomiting, hepatomegaly and encephalopathy when child develops infection, and neurological finding that improve slightly then remain static. Treatment includes fever control, fluids, glucose and carnitine is recommended. Prognosis is guarded if not treated. Our patient, a 2 year old boy came with weakness of lower limbs, inability to hold head since past 1 year with abnormal posturing of limbs since past 9 months. He had attained normal milestones, when at 1 year of age he had high grade fever, loose stools and vomiting followed by loss of previously attained milestones with weakness of limbs which remained same since then. Child had macrocephaly,hypertonia of 4 limbs, dystonia of upper limbs and ugoing plantars.CSF lactate was raised, MRI brain showed altered signal intensity in lentiform nuclei, cerebral atrophy and symmetrically enlarged CSF spaces in bilateral temporal fossae and frontoparietal subdural spaces(batwing dilatation of sylvian fissures). Tandem mass spectroscopy showed high concentration of glutarylcarnitine. Treated with low protein, high carbohydrate diet with oral riboflavin and carnitine and physiotherapy. Patient showed no improvement probably due to late presentation to hospital and was counselled regarding prognosis and discharged.