Table 3
advertisement
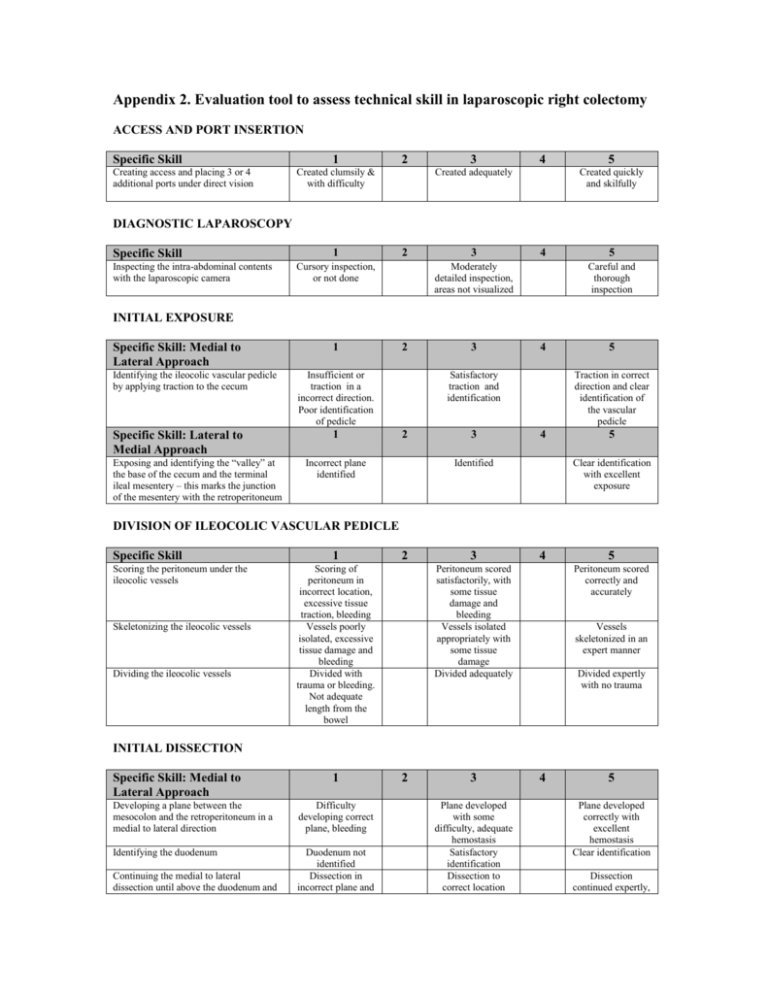
Appendix 2. Evaluation tool to assess technical skill in laparoscopic right colectomy ACCESS AND PORT INSERTION Specific Skill Creating access and placing 3 or 4 additional ports under direct vision 1 2 Created clumsily & with difficulty 3 4 Created adequately 5 Created quickly and skilfully DIAGNOSTIC LAPAROSCOPY Specific Skill Inspecting the intra-abdominal contents with the laparoscopic camera 1 2 Cursory inspection, or not done 3 4 Moderately detailed inspection, areas not visualized 5 Careful and thorough inspection INITIAL EXPOSURE Specific Skill: Medial to Lateral Approach Identifying the ileocolic vascular pedicle by applying traction to the cecum Specific Skill: Lateral to Medial Approach Exposing and identifying the “valley” at the base of the cecum and the terminal ileal mesentery – this marks the junction of the mesentery with the retroperitoneum 1 2 Insufficient or traction in a incorrect direction. Poor identification of pedicle 1 3 4 Satisfactory traction and identification 2 Incorrect plane identified 3 5 Traction in correct direction and clear identification of the vascular pedicle 4 Identified 5 Clear identification with excellent exposure DIVISION OF ILEOCOLIC VASCULAR PEDICLE Specific Skill Scoring the peritoneum under the ileocolic vessels Skeletonizing the ileocolic vessels Dividing the ileocolic vessels 1 2 Scoring of peritoneum in incorrect location, excessive tissue traction, bleeding Vessels poorly isolated, excessive tissue damage and bleeding Divided with trauma or bleeding. Not adequate length from the bowel 3 4 Peritoneum scored satisfactorily, with some tissue damage and bleeding Vessels isolated appropriately with some tissue damage Divided adequately 5 Peritoneum scored correctly and accurately Vessels skeletonized in an expert manner Divided expertly with no trauma INITIAL DISSECTION Specific Skill: Medial to Lateral Approach 1 Developing a plane between the mesocolon and the retroperitoneum in a medial to lateral direction Difficulty developing correct plane, bleeding Identifying the duodenum Duodenum not identified Dissection in incorrect plane and Continuing the medial to lateral dissection until above the duodenum and 2 3 Plane developed with some difficulty, adequate hemostasis Satisfactory identification Dissection to correct location 4 5 Plane developed correctly with excellent hemostasis Clear identification Dissection continued expertly, the head of the pancreas and under the transverse mesocolon Identifying the right branch of the middle colic artery Dividing the right branch of the middle colic artery Specific Skill: Lateral to Medial Approach Scoring the peritoneum around the cecum and the terminal ileum (TI) along this valley and entering the retroperitoneal plane Opening the right lateral peritoneal reflection (lateral to the cecum and the ascending colon) and dissecting towards the midline Exposing the duodenum Mobilizing the ascending colon to the midline with inadequate exposure, tissue trauma and bleeding Poor identification, inadequate dissection Divided with poor hemostasis 1 with minimal trauma in correct plane and to correct location. No bleeding Clear identification Satisfactory identification Divided adequately 2 3 Difficulty entering retroperitoneal plane Entered correct retroperitoneal plane Difficulty remaining in correct plane Correct plane developed with some difficulty Poor exposure Difficulty with mobilization or excessive bleeding Adequate exposure Mobilization with moderate hemostasis Divided safely with good hemostasis 4 5 Entered into correct plane smoothly and accurately Correct plane developed Good exposure Mobilization with excellent hemostasis MOBILIZATION OF THE HEPATIC FLEXURE Specific Skill Positioning the patient in reverse Trendelenburg with their right side up Dividing the omental attachments at the transverse colon Entering the lesser sac and dividing the omentum proximally Medial-caudal retraction of the flexure Dividing the flexure with an appropriate energy source 1 2 3 Patient not positioned correctly Patient positioned correctly after some delay Attachments divided with poor technique, correct plane not identified, bleeding Trouble entering lesser sac. Omentum divided with associated trauma Flexure not retracted in correct direction Flexure divided with excessive tissue trauma, bleeding Attachments divided with some bleeding 4 5 Patient repositioned at correct point in the operation Attachments divided with good hemostasis Lesser sac entered in the correct plane with some difficulty, minimal bleeding Flexure retracted adequately after some repositioning Flexure divided adequately Lesser sac entered and omentum divided in an expert manner Flexure retracted appropriately and in correct direction Flexure divided in an expert manner with no tissue trauma or bleeding EXTERIORIZATION BOWEL RESECTION AND ANASTAMOSIS Specific Skill Dividing the proximal and distal bowel intra- or extra-corporeally Using a wound protector if the bowel is exteriorized Anastomosis performed according to the surgeon’s preference 1 Bowel divided with tissue trauma and gross contamination Wound protector not used Anastomosis made clumsily with spillage of bowel contents, bleeding, or under tension 2 3 Bowel divided with minimal spillage Anastomosis made adequately with some assistance 4 5 Bowel divided cleanly and expertly Wound protector used Anastomosis made with no spillage, good hemostasis and no tension