Optimal strategy in patients with suspected acute appendicitis
advertisement

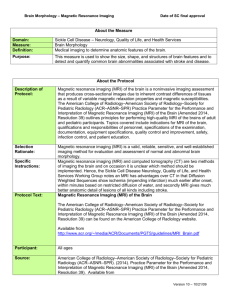
Najaarsvergadering NVGE, oktober 2011 Can MRI replace CT in patients with suspected acute appendicitis? A multicenter diagnostic accuracy study MMN Leeuwenburgh1,2, BM Wiarda3, APJ Houdijk4, BC Vrouenraets5, S Jensch6, MJ Wiezer7, HW van Es8, WH Bouma9, JWC Gratama10, HBAC Stockmann11, A Spilt12, LPJ Cobben13, PMM Bossuyt14, J Stoker2, MA Boermeester1 on behalf of the OPTIMAP study group Department of Surgery, Academic Medical Centre, University of Amsterdam, Department of Radiology, Academic Medical Centre, University of Amsterdam, 3 Department of Radiology, Alkmaar Medical Centre, Alkmaar,4Department of Surgery, Alkmaar Medical Centre, Alkmaar, 5Department of Surgery, Sint Lucas Andreas Hospital, Amsterdam, 6Department of Radiology, Sint Lucas Andreas Hospital, Amsterdam, 7 Department of Surgery, Sint Antonius Hospital, Nieuwegein, 8Department of Radiology, Sint Antonius Hospital, Nieuwegein, 9Department of Surgery, Gelre Hospitals, Apeldoorn, 10 Department of Radiology, Gelre Hospitals, Apeldoorn, 11Department of Surgery, Kennemer Gasthuis,12Department of Radiology, Kennemer Gasthuis,13Department of Radiology, Medisch Centrum Haaglanden, Leidschendam,14Department of Clinical Epidemiology, Academic Medical Centre, University of Amsterdam, the Netherlands 1 2 In patients with suspected appendicitis, imaging is needed to substantiate the clinical diagnosis. The accuracy of US is suboptimal and the use of ionizing radiation in CT has the risk of inducing malignancy. MRI is an alternative imaging option. The aim of this study was to compare imaging strategies in adult patients with suspected appendicitis. Data were collected in a multicenter study in which patients with clinically suspected appendicitis were prospectively included at the emergency department of six hospitals. Consenting patients underwent a standard protocol, with initial US, followed by CT in case of negative or inconclusive US results. Additionally, all patients underwent MRI (HASTE, HASTE SPAIR, DWI), with the MRI reader blinded for the results of the other imaging methods. A final diagnosis was assigned by an expert panel based on histopathology and clinical follow up after 3 months. We evaluated the sensitivity and specificity of three imaging strategies: (1) US in all patients followed by CT after a negative or inconclusive US; (2) US followed by MRI after a negative or inconclusive US; (3) MRI only. Statistical differences in accuracy between strategies were evaluated with the McNemar test. In total, 230 patients were included; 223 patients underwent MRI according to the study protocol; their mean age was 38 years, 41% were male. The expert panel assigned acute appendicitis as final diagnosis in 118 patients (51%). Conditional imaging strategies with CT or MR after a negative or inconclusive US resulted in comparable sensitivity of 0.97 (95%CI 0.93 to 0.99) and 0.99 (95%CI 0.95 to 1.00, p=0.50) at a specificity of 0.91 (95%CI 0.84 to 0.95) and 0.88 (95%CI 0.81 to 0.93, p=0.45) respectively. The MRI only strategy had a similar high sensitivity (0.97, 95% CI 0.92 to 0.99) and specificity (0.93, 95%CI 0.87 to 0.97). Conclusion – MRI is an appropriate replacement for CT in detecting acute appendicitis in adult patients in the emergency department. Strategies with conditional CT or MRI after a negative or inconclusive US have comparable accuracy. An MRI only strategy could be an alternative approach.