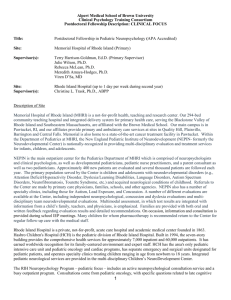
division of pediatric emergency medicine
advertisement

PEDS EMERGENCY FELLOWSHIP BINDER Revised February 2009 Section III 1 CONTENTS Section 1 Leadership Lines of Responsibility Grievance Policy Disciplinary Action Phone List Web Pages Physician Photos Section II Purpose of Fellowship Curriculum Overview Clinical Responsibilities Administrative Responsibilities Rotations Section III Schedules Moonlighting Section IV Evaluations Section V Conferences Section VI Other Responsibilities Section VII General Information Section VIII Summary Maps Section III 2 DIVISION OF PEDIATRIC EMERGENCY MEDICINE FELLOWSHIP ORIENTATION MANUAL SIGNATURE PAGE The Division of Pediatric Emergency Medicine has developed this manual to assist fellows in the program in understanding the operations, guidelines and policies of the division, department, and affiliated health care systems. This manual will be updated periodically for necessary changes and reviewed annually. If you have any questions, please see the fellowship director. Your signature below indicates that you have received a copy of this manual and understand the importance in reading it and using it as a reference in the future. Naghma Khan, MD Division Director Steven Lanski, MD Fellowship Director _________________________________________ _____________________________________ Date _____________________________________ Date _______________________________ Pediatric Emergency Medicine Fellow _____________________________, MD Date______________________________________ Section III 3 ADMINISTRATIVE CONTACTS TO THE DIVISION OF PEDIATRIC EMERGENCY MEDICINE Emory University School of Medicine Children’s Healthcare of Atlanta Medical School Dean: Tom Lawley, MD Chairperson: Barbara Stolle, MD Graduate Medical Ed: James Zaiden, MD Division Director: Naghma Khan, MD Assoc. Div Director: Harold Simon, MD SVPMA: Jay Berkelhamer, MD VPMA: Corinne Taylor, MD Medical Director: Naghma Khan, MD Hughes Spalding Children’s Hospital Pediatric Emergency and Urgent Care Centers (PEC and PUC) Medical Director: Naghma Khan, MD Assoc. Medical Director: Wendy King, MD Division Director: Naghma Khan, MD Nurse Manager: Angela Smith Emergency Center @ Egleston Medical Director: Naghma Khan, MD Assoc. Medical Director: Alesia Fleming, MD Nurse Director: Maryann Hatfield Division Director: Naghma Khan, MD Nurse Manager: Laura Jones Administrative Personnel Office Business Manager: Debra Busby Fellowship Coordinator: Donna Stringfellow Coding Clerk – Annette Myers Research Coordinator – Michael Deguzman, MPH Section III 4 EMERGENCY PEDIATRIC GROUP LEADERSHIP Division and Medical Director Naghma Khan, MD Associate Division Director / Academic Director Harold Simon, MD, MBA Associate Medical Director – Hughes Spalding ED Wendy King, MD Associate Medical Director – Egleston ED Alesia Fleming, MD Associate Medical Director – Business Affairs Jeff Linzer, MD Residency Education Coordinator David Goo, MD Fellowship Director – Steven Lanski, MD Advisory Council Chair/Div Director Fellowship Director Call Center Assoc Director PEM Representative PEM Representative UC Representative - Section III Naghma Khan, MD Steven Lanski, MD Daniel Hirsh, MD Debra Young, MD Michael Ziegler, MD Roshni Patel, MD 5 LINES OF RESPONSIBILITY Questions, Concerns, Issues, Grievances Supervising Physician for Individual Patient Supervising Physician For Rotation or Elective Always Available -Fellowship Director -Associate Fellowship Director -Division Administrator on Call Divisional Director or Associate Director Department of Pediatrics, Chairperson Emory University School of Graduate Medical Education Section III 6 Lines of Responsibility (For Trainees in Pediatric Emergency Medicine) It should be noted that at any point in time trainees should feel free to contact any individual outlined in the preceding page should questions or concerns arise with either clinical or non-clinical responsibilities. The following is designed as a general overview of the structure for the Pediatric Emergency Medicine Group and its relationship to trainees. Remember that you can contact your advisor or the fellowship director at any point in time should this not be clear or if questions arise. 1) When dealing with individual patient issues, you should first contact or discuss issues and concerns with the supervisory physician responsible for the particular clinical situation. At all times, there is also a divisional administrator on call who is immediately available. The administrator is listed on the daily call schedule. 2) Should concerns arise in which additional input concerning an elective, rotation, or clinical situation occur, you can contact the supervisory physician for that particular rotation. 3) The Fellowship Director can then be contacted should additional concerns arise and can be contacted immediately should you feel the situation deems immediate input or intervention. 4) Further questions or concerns can be directly addressed with the Division Director. Again, if you feel the situation warrants such contact, you should feel free to do so. 5) Additional concerns can be taken directly to the Chairman of Pediatrics or directly to Graduate Medical Education for Emory University (also see House-Staff Manual). Please remember that this is a general guide for the individual lines of responsibility, but that the Fellowship Director, Associate Director, Advisors, Administrators-On-Call, and anyone else can be contacted directly should you feel that their input is needed. Section III 7 Grievance Policy Pediatric Emergency Medicine Fellowship Program We always attempt to solve grievances and discipline issues concerning fellows in a professional, efficient and constructive way for all parties. Any grievances, either from or directed at a fellow, which concerns a possible violation of Emory University policy should be immediately presented to the Fellowship Director or Division Director. The guidelines for approaching these and all other similar disputes are detailed in the Housestaff Manual which supersedes the policy detailed here. For grievances and discipline issues which are not covered in the Housestaff Manual, the following guidelines will be implemented. Any attending, nurse, patient, resident or other trainees who have concerns with a fellow (or vice-versa) are encouraged to directly approach the individual as soon as possible in a discreet and professional manner. If the conflict cannot be resolved at that level or if those involved do not feel comfortable in directly approaching others involved then the following process will be implemented. The first arbiter of the dispute is the fellow’s advisor. The advisor is required to meet individually with those involved within 1 week of being notified of the dispute. If the advisor is already a party to the dispute then the Fellowship Director will fill the role of arbiter. After discussing the details of the dispute with all involved individuals, the advisor or Fellowship Director will attempt to reconcile the dispute and submit their written recommendations to the Fellowship Director (or Division Director if the arbiter is Fellowship Director). If any party wishes to pursue the matter further, then the grievance will be presented to the Chairman of the Fellowship Directors in the Department of Pediatrics. The Chairman is asked to review the case with 2 additional directors who have no prior involvement in the dispute. If, for whatever reason, the dispute is not resolved at this level, then will be presented to the Graduate Medical Education director as per Housestaff Guidelines. Please remember that this is a general guide and that the fellowship director, division director, advisors, administrators on call can all be contacted directly should you feel that their input is warranted. Section III 8 Disciplinary Action Pediatric Emergency Medicine Fellowship Program The following applies to violations of policy established by the Fellowship in Pediatric Medicine. Any violations of Emory University policy is subject to disciplinary action dictated by the University as detailed in the Housestaff Manual. The purpose of any disciplinary action is to provide support and guidance for deficits in the fellow’s performance. Fellows who violate PEM Fellowship policy may be disciplined at the discretion of the fellowship director using interventions proportional to the infraction. For example, if a fellow fails to successfully complete a rotation then they will be required to repeat the rotation. If the rotation is not satisfactorily completed during the elective month, then the rotation may be added on to the end of the training period in order to satisfactorily complete the fellowship program. If the rotation is not completed in a satisfactory manner after these 2 attempts then the fellow will not have successfully completed the program requirements. The following behaviors may result in loss of elective time: Failure to satisfactorily complete any required rotation or prior elective Failure to have an approved research paper submitted for publication by April of the fellow’s final in year training Failure to attend the minimum number of required conferences (barring prior excuse from the fellowship director) during any academic year Failure to submit signed forms required of the fellowship within 15 days of notification (e.g. performance reviews, timesheets) Failure to fulfill required teaching and administrative responsibilities as described in the Fellowship Manual Receiving anything less than Satisfactory on rotation evaluations or biannual evaluations. Any potential violation of Fellowship Policy not covered here will be reviewed by the Fellowship Director along with the Fellow’s Advisor and, possibly, the Division Director. Disputes regarding disciplinary action will be addressed as outlined in the Grievance Policy. Section III 9 EMERGENCY MEDICINE GROUP: PHONE LIST Pediatric Emergency Physicians Laurie Burton, MD John Cheng, MD Ellis Dixon, MD Alesia Fleming, MD David Goo, MD Michael Greenwald, MD Daniel (Dan) Hirsh, MD Shabnam Jain, MD Naghma Khan, MD Steven (Steve) Lanski,MD Jeffrey (Jeff) Linzer, MD Wendy Little, MD Dallin Randolph, MD Amita Shroff, MD Harold (Hal) Simon, MD Samuel (Sam) Spizman, MD Jesse Sturm, MD Taryn Taylor, MD Mark Ward, MD Deborah (Debbie) Young, MD Michael (Mike) Ziegler, MD Urgent Care Physicians Denise Claxton, MD Karen Colton, MD Anthony (Tony) Cooley, MD Tiffany McKinnie. MD Tracy Merrill, MD Michael (Mike) Miello, MD Roshni Patel, MD Amy Pattishall, MD Mary Sawyer, MD Fellows Eiman Abdulrahman, MD Brian Costello, MD Rebecca Floyed, MD Jonathan Rochlin, MD Jesse Sturm, MD Amanda Pierzchala, MD Shervin Kharazmi, MD Maggie Menoch, MD John Misdary, MD Support Staff Debra Busby Donna Stringfellow Annette Myers Michael Deguzman EEC PEC PUC (walk-in) Other Numbers Graduate Medical Education Paging Operator Section III Office 404-785-7130 404-785-7136 404-785-7130 404-785-7123 404-785-7124 404-785-7121 404-785-7132 404-785-7126 404-785-7127 404-785-7137 404-785-7131 404-785-7128 404-785-7130 404-785-7139 404-785-7133 404-785-7134 404-785-7449 404-785-7122 404-785-7135 404-785-7130 404-785-7140 Pager/Cell 404-427-9025 (c) 404-274-6949 (c) 404-406-5158 (c) 404-695-4841 (c) 404-226-0274 (c) 678-520-2299 (c) 678-613-8870 (c) 770-915-5294 678-462-2228 (c) 678-613-8939 (c) 404-408-2561 (c) 404-217-8291 (c) 770-314-7126 (c) 917-915-1097 (c) 404-518-9516 (c) 404-837-1628 919-423-5579 (c) 443-812-3569 (c) 404-754-7992 (c) 404-310-9668 (c) 404-805-2699 (c) Home 404-373-9903 404-274-6949 404-327-9769 770-879-2505 404-337-9150 770-457-3986 404-895-6447 770-414-1140 770-551-0929 678-613-8939 404-636-2190 404-253-9986 404-370-1355 404-941-9387 404-636-1442 404-816-6676 919-423-5579 (c) 443-812-3569 404-876-7457 770-981-2739 404-929-6782 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir 1645 Tullie Cir 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 404-785-7130 404-785-7130 404-785-7130 404-785-7130 404-785-7130 404-785-7130 404-785-7130 404-785-7130 404-778-1422 404-225-1777 (c) 404-683-0876 (c) 404-754-3274 (c) 404-225-0791 770-397-0072 404-406-4390 (c) 404-668-1205 (c) 717-350-5636 (c) 404-403-6619 (c) 404-212-4970 404-687-9641 404-892-9241 404-512-11561 (c) 404-213-4341 (c) 770-928-1123 404-552-8966 717-350-5636 404-403-6619 (c) 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir Grady FOB 404-785-7129 404-785-7129 404-785-7129 404-785-7138 404-785-7449 404-785-7151 404-785404-785404-785- 404-686-5000 #14603 404-686-5000 #16861 404-686-5500 #16994 404-686-5500 #15905 404-686-5500 #11846 404-686-5500 #15614 404-686-5500 #18629 404-686-5500 #18662 404-686-5500 # 18665 919-824-1162 (c) 612-669-5853 (c) 504-452-7115 (c) 917-359-0306 (c) 919- 423-5579 (c) 404-513-3972 (c) 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. 1645 Tullie Cir. Business Coordinator Program Coordinator Coding Clerk Research Coord. 404-785-7141 404-785-7142 404-778-1423 404-785-7209 404-785-6405 404-785-9662 404-785-9640 404-785-7989 Fax 404-785-7989 Fax 404-778-1401 Fax 404-785-7989 Fax 404-785-1545 Fax 404-785-9650 Fax 404-785-9561 Fax 1645 Tullie Cir. 1645 Tullie Cir. Hughes Spalding 1645 Tullie Cir 404-727-0456 404-315-6000 10 OTHER USEFUL NUMBERS TO KNOW GRADUATE MEDICAL EDUCATION – 404-727-0456 EMORY BENEFITS OFFICE - 404-727-7613 EMORY HUMAN RESOURCES – 404-727-7611 EMORY BADGES – 404-727-0224 EMORY COMPUTER HELPDESK – 404-727-7777 EMORY PAYROLL – 404-727-7617 GRADY BADGES – 404-616-1908 GRADY PARKING – 404-616-3769 CHOA HUMAN RESOURCES –404-785-0153 CHOA BADGES – 404-785-7820 CHOA COMPUTER HELP – 404-785-6767 CHOA RESIDENT COORDINATOR – 404-785-6418 IBEX TRAINING AT EGLESTON - (404) 785-1875 Section III 11 WEB Pages to Know www.epgatlanta.org Pediatric Emergency Group http://www.medweb.emory.edu/MedWeb/ (Emory MedWeb) http://med.emory.edu/PEDIATRICS/ (Department of Pediatrics) http://www.hr.emory.edu/ (Human Resources for Emory) http://www.abp.org/ (American Board of Pediatrics) http://directory.service.emory.edu/ (List of Emory Faculty & Staff) http://careforce/ CHOA Careforce Connection https://simonweb.eushc.org/ SmartWeb Paging Composite State Board of Medical Examiners https://www.ganet.org/sosrenew/meb/renewappl.cgi Section III 12 PEM PHYSICIANS Laurie Burton John Cheng David Goo Mike Greenwald Naghma Khan Steve Lanski Dallin Randolph Section III Hal Simon Ellis Dixon Dan Hirsh Jeff Linzer Sam Spizman Alesia Fleming Shabnam Jain Wendy Little Jesse Sturm 13 Taryn Taylor Mark Ward Debbie Young Mike Ziegler URGENT CARE PHYSICIANS Denise Claxton Tony Cooley Tracy Merrill Mike Miello Section III Karen Colton Roshni Patel Tiffanie McKinnie Mary Sawyer 14 FELLOWS 3rd Year Jonathan Rochlin Amanda Pierzchala 2nd Year Eiman Abdurahman Brian Costello Rebecca Floyed Maggie Menoch John Misdary 1st Year Shervin Kharazmi Section III 15 I. PURPOSE OF FELLOWSHIP Our program aspires to train our fellows to become outstanding clinicians. We also strive to support the development of research and teaching skills that will allow for success in the changing world of academic medicine, and encourage the understanding of administrative issues to allow for future involvement in positions of leadership in academic pediatric emergency medicine. The fellowship provides the opportunity to attain all these goals. This manual is devoted to introducing you to the basic operating procedures of this fellowship and the pediatric division of Emergency Medicine. II. EXPECTATIONS FOR FELLOWS Our program complies with all requirements for board certification as outlined by the American Board of Pediatrics. In addition, the following standards should be accomplished: Patient Care: Year 1 Develop competence in technical skills such as advanced resuscitation and airway management, percutaneous central intravenous lines, intraosseous needle placement, splinting, and advanced wound care. Each fellow will develop their skill in obtaining an accurate history and physical assessments of their patients. First year fellows will acquire all the basic technical skills for the compassionate care of acutely ill and injured children. Year 2 The fellow will continue working on gaining more complex procedural skills as well as increasing independence in decision making regarding medically complex and high acuity patients. Increased opportunity for supervising and clinical education of medical students and residents will occurs as well. Year 3 The fellow will have all the necessary skills and knowledge to care for the most ill and injured children at this stage. The fellow will concentrate on aiding in the flow and overall management of the emergency department with the attending. Fellows will be expected to take the lead on medical resuscitations as well as take calls from referring institutions during this period of training. Medical Knowledge: The fellow will learn to diagnose and manage a vast variety of pediatric medical conditions from the very common (asthma, various infectious conditions and minor injuries) to the uncommon and medically complex (rare genetic conditions, organ transplant recipients, immunocompromised patients and major trauma patients). Fellow will be expected to research conditions that they are unfamiliar with to aid in the growth of their medical knowledge. Lecture development and research question development (described below) will further aid in the fellow’s knowledge base. Section III 16 Practice Based Learning and Improvement: Each fellow will develop formal presentations complete with images and handouts. These presentations will enhance the fellow’s ability to gather medical information using electronic and library databases as well as increase their medical knowledge. The fellow’s ability to evaluate and assimilate pertinent evidence into clinical practice will be enhanced as well as lecture preparation skills. Fellows will maintain an up-to-date record of all advanced procedures performed. The procedure log will be turned in at each semi-annual evaluation. Fellows as well as the program will use the log to assess adequate exposure to procedures commonly used in the practice of pediatric emergency medicine. The first year fellow will develop a research project related to a topic of interest. The initial exploration of a research question in conjunction with a faculty research advisor will enhance both the fellow’s medical knowledge as well as their information gathering and assimilation skills as well. This process continues throughout the 3 years of fellowship and typically repeats at least once based on the individual fellows research productivity. Interpersonal and Communication Skills: Year 1 Fellows present lectures at the divisional and possibly departmental level. Progress will be monitored with the ultimate goal of developing individual teaching portfolios and acquiring confidence presenting to different audiences. A teaching course will be given during the first year, which includes a variety of topics relating to public speaking. During the middle portion of the first year the fellows will have increasing exposure to supervising medical students and residents to begin to develop their bedside teaching skills. Year 2 Fellows will expand their lecture audience to include other departments, the community as well as regional lecture and research presentation opportunities. Increased supervision and teaching of junior trainees occurs in the second and continues throughout the third year of fellowship. Year 3 Continue to expand lecture and research presentation audiences to include national and possibly international venues. Throughout the 3 years fellows will learn to communicate effectively to a wide variety of people from different backgrounds including medical personnel and families. Section III 17 Professionalism: Fellows attend an ethics course in the first year, which covers various aspects of ethical decision making in medicine. In the course each fellow will learn how medical decision-making can be biased and how to begin to develop their own compassionate fair method of medical decision-making. Throughout the 3 years of fellowship, each fellow is exposed to issues of compassionate patient care during the monthly divisional meetings as well as weekly fellows’ conferences. Topics such as abuse evaluations, pain management and approach to handling a difficult family are addressed. System Based Practice: Each fellow will be a member of a hospital committee during their fellowship. During the first year each fellow will choose a committee and begin attending the monthly meetings. This experience is designed so that each fellow will understand how the practice of emergency medicine pertains to the hospital system and medical community. The more senior fellows, after being a member of a committee for a period of time, will be expected to take on a more active role in discussions as well as any projects the committee is involved. Research Activities: Year 1 Define a research plan in consultation with the Scholarship Oversight Committee. This should include the following: a. an outline of a general research plan for your fellowship experience starting with primary project HIC protocol submission through data collection, statistical analysis, manuscript preparation and submission. Also included should be plans for your secondary project(s). “Subspecialty residents must be instructed in the scientific and ethical bases of clinical research, including study design, modeling and methodology, statistical concepts, and data collection and analysis. Research must begin the first year and continue for the entire period of training to allow adequate time for the development of research skills, completion of research projects, and presentation of results to the medical community. Each subspecialty resident must actively participate in the design, conduct, evaluation, and preparation for publication of a clinical or laboratory research project in his/her subspecialty area.” ABP 3/07 b. Meaningful progress on HIC protocol submission should be demonstrated by the end of your first year. c. A manuscript of the research, submitted to a peer reviewed journal, will ultimately be required for successful completion of the fellowship. This is in conjunction with the standards set by the ABP for sub-specialty training in Pediatric Emergency Medicine. “In addition to participation in a core curriculum in scholarly activities, all fellows who began training on or after July 1, 2004, will be expected to engage in projects in which they develop hypotheses or in projects of substantive scholarly exploration or analysis. Areas in which Scholarly Activity may be pursued include, but are not limited to: basic, clinical or translational biomedicine, health services, quality improvement, bioethics, education, and public policy.” APB-03/07 Section III 18 Year 2 During the second year the fellow has significant time allotted to research related activities. Each fellow should have IRB approval completed early in the second year if it has not already occurred and be involved in data collection during the year. Preparation and submission of an abstract with preliminary data collected should occur by the end of the second year. Year 3 The third year is designed to allow continued research time and provide an opportunity for the preparation of a manuscript for publication. By the spring of the third year each fellow should have submitted to the ABP the actual “work product” of his/her scholarly activity. Each fellow should also have submitted to the ABP a comprehensive document describing the scholarly activity that includes a description of your role in each aspect of the activity and how it relates to your career development plan. Section III 19 FELLOWSHIP CURRICULUM OVERVIEW PEDIATRIC EMERGENCY MEDICINE 2009/2010 Clinical Education and Responsibilities (4 week block rotation) ** A. B. Pediatric Residency trained 1st Year 2nd Year Emerg. Dept. 5 Anesthesia 1 Toxicology 1 Orthopedics 1 PICU 1 Child Advocacy 1 Trauma 1 Research/Elec 2 ________________ Total 13 Emerg. Dept Research Adult ED PICU 3rd Year* 5 6 1 1 Emerg Dept. Research Adult ED EMS 13 5 6 1 1 13 EM Residency trained 1st Year Emerg. Dept. Anesthesia NICU Peds Ortho PICU Elective Advocacy Inpatient Total 2nd Year 5 1 1 1 1 2 1 1 13 Ped Emerg. Dept *Electives Outpatient Primary Outpatient Subs PICU 8 2 1 1 1 _______________________ 13 Electives can be chosen in consultation with the fellowship director from opportunities within the Egleston/Emory system (eg., Plastic Surgery, Ophthalmology, Radiology, Pediatric Surgery, Oral Surgery, Allergy & Immunology, Cardiology, Dermatology, Genetics, Endocrinology, Gastroenterology, Hematology/Oncology, Infectious Disease, Neurology, Psychiatry, Pulmonary, Nephrology, Sports Medicine, and Sexual/Physical Abuse). It will also be possible to pursue electives at other institutions, including The National PEM Fellowship Exchange Program. Electives may also be dedicated solely to research endeavors. In addition, an Introduction to Research Symposium is held annually and participation is mandatory for 1 st year fellows. 3 Vacation weeks and out-of-town conference time can be taken during elective/research months. Section III 20 Clinical Responsibilities Year 1: 32 hours/week during dedicated ED months 40 hours/month during research/elective months Year 2: 28 hours/week during dedicated ED months 40 hours/month during research/elective months Year 3: 32 hours/week during dedicated ED months 40 hours/month during research/elective months In general, shifts are scheduled during the busiest hours of the day to optimize exposure. The above is subject to change based on divisional needs and requirements of the American Board of Pediatrics. The Following Certifications will be Obtained During Fellowship (and are paid for by the division) Pediatric Advanced Life Support (PALS) – recertification only Advanced Cardiac Life Support (ACLS) Advanced Trauma Life Support (ATLS) Research Mentor: For each research month, the fellow will choose an attending research mentor from the PEM group to review short and long term goals and objectives in regards to the fellow’s research project. Written objectives for the month are expected to be turned in BEFORE the beginning of the research block and a list of written accomplishments are expected to be turned in at the end of the research rotation. Fellows are expected to take notes during each of their SOC meetings and turn a copy of the notes in following the meeting. Failure to receive a satisfactory evaluation during a research block may result in loss of elective time. Multiple occurrences will result in extension of the fellowship training period and possible expulsion from the training program. Evaluations (See page 29 for more info on evaluations): 1. 2. 3. 4. 5. Section III The supervising attending on non-Emergency rotations will complete evaluations during service months PEM attendings will be asked to evaluate fellows during their PEM clinical months. Research mentors will be asked to evaluate fellows during the research months PEM attendings will be asked to evaluate fellows on a per block basis and a meeting with the fellowship director will take place semi-annually to assess progress and performances in all areas of the curriculum. The periodic evaluations (from attendings and rotations) will be reviewed. This will include input and suggestions for improvement or changes needed in the training program. You will also be given the opportunity for anonymous feedback to the fellowship director or division director. You will be included in the division annual review process in which all attendings are reviewed anonymously by peers. Evaluations are available through the program coordinator for fellows to review at any time. 21 Research: Required as defined by the American Board of Pediatrics – see above Attendance to the Introduction to Research course is required in the 1 st year of fellowship 2 sessions with the division’s research coordinator in aiding in all aspects of divisional research efforts will be mandatory during each research block. Production of a completed research project deemed important to the field of emergency medicine is required. 1. 2. 3. 4. Administrative Responsibilities: 1. 2. 3. 4. 5. Participation in a hospital or healthcare committee is required Attendance to divisional business meeting is mandatory (unless on vacation or outside call rotation) 1st year fellows are responsible for presentation of cases for quality improvement 2nd year fellows are responsible for fellows conference lecture schedule 3rd year fellows are responsible for the fellows clinical schedule and collection of fellows clinical productivity data. Increasing responsibility by overseeing flow and function of the ED. This is expected throughout the training program. Fellows are expected to give feedback and suggestions during divisional business meetings as to how the flow and function of the ED can be improved. 6. Teaching: 1. 2. 3. 4. 5. Section III Give one noon conference per year to the Pediatric residents and to the Emergency Medicine residents Participate in Journal Club Participate and give grand rounds and other educational presentations Gradually increase bedside teaching for junior trainees Participate in weekly fellow’s conferences with at least 2 lectures given annually 22 Core Rotations for the Pediatric Emergency Medicine Program: Advocacy Contact Person: Stephen Messner Office Number: 404-785-3820 Email: stephen.messner@choa.org Goals and Objectives: Patient Care: The fellow should develop the skills necessary for evaluation and management of pediatric patients presenting for abuse evaluation. The fellow will learn when to suspect possible abuse and the appropriate work-up involved in such cases including appropriate evidence collection, immediate and follow-up care. Medical Knowledge: The fellow should become familiar with the signs which suggest abuse and treatment available for the patient in which abuse is suspected including those to prevent/treat sexually transmitted diseases . Practice Based Learning: The fellow will be exposed to new and/or improvement in abuse/neglect evaluation and treatment. The fellow should be prepared to present a brief discussion on the evidence supporting these approaches at the end of the rotation to members of the pediatric emergency medicine group. Interpersonal and Communication Skills: This discipline relays on a practitioners communication skills and the fellow will be exposed to new approaches which differ from those typically used in the emergency department setting. The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner. These skills will be part of the formal evaluation at the end of the rotation. Professionalism: The fellow will be exposed to ethical considerations in caring for patients who are evaluated and treated for abuse. This includes the ability to make care recommendations based on the best available evidence and not biased by impressions. Systems Based Practice: The fellow will be exposed to the system which is utilized in the care of children who have been abused or neglected including personnel from medicine, social and legal services. This exposure will allow the fellow to better utilize these personnel in the care of patients they evaluate in the emergency department setting. Anesthesiology Contact Person: Carolyn Bannister, MD, Director of Pediatric Anesthesia Office Number: 404-785-6670 Email: cbannis@emory.edu Goals and Objectives: Patient Care: The fellow should develop the skills necessary for management of critical airways in children. The fellow should become familiar and comfortable with Bag-valve mask techniques, intubations, and Laryngeal Mask Airways. The fellow will also become familiar with rapid sequence intubation and management of the difficult airway. The number of procedures will be assessed through a patient log, and the fellow’s ability to adequately perform all techniques will be assessed by a supervising attending at the end of the rotation. Medical Knowledge: The fellow should become familiar with all medications and equipment for airway management. This includes familiarity with inhalation agents and the use of paralytics, sedatives and reversal agents. The fellow will learn indications and contraindications of different types of intubation techniques – endotracheal, nasotracheal, LMA and other advanced airways. Section III 23 Practice Based Learning: The fellow will be exposed to new and/or improvement in anesthetic techniques and will be required to present a brief discussion on the evidence supporting its use at the end of the rotation to members of the pediatric emergency medicine group. Interpersonal and Communication Skills and Professionalism: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with coworkers and patients. These skills will be part of the formal evaluation at the end of the rotation. Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess quality of service in anesthesia. The fellow will be exposed to the role and interactions with other services the anesthesia service has in providing care outside the operating room (examples: call for trauma related patients, sedation, radiology, hospital codes…). By the end of the rotation the fellow should be comfortable with the pediatric airway and its management and the role the anesthesia service has in the hospital as a whole. The rotation should be completed early in the first year I order to assure comfort and familiarity with airway management. Inpatient Pediatrics Contact Person: Joseph Snitzer Office Number: 404- 785-6104 Email: jsnitze@emory.edu Goals and Objectives: Patient Care: The fellow to learn to manage a wide variety of ill and injured children following initial emergency department stabilization. The fellow should become familiar with on-going management of common pediatric illness as well as uncommon diagnostically challenging conditions. The fellow should become an integral part of the inpatient team and function with the responsibilities as would be expected of a junior hospitalist fellow. Medical Knowledge: The fellow should also become familiar with the tests utilized to diagnose common and uncommon pediatric medical conditions. The on-going use of advanced care medications such as antibotics, analgesics and immunoregulatory medications will be covered. The fellow will learn the issues and management involved in continued pediatric medical care for a wide variety of conditions in the inpatient setting. Practiced Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in pediatric medicine and will give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Interpersonal and Communication Skills: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with co-workers and patients. These skills will be part of the formal evaluation at the end of the rotation. Professionalism: The fellow will be exposed to ethical considerations involved with in-patient care including discussions involving when continued outpatient care is appropriate. Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess cost effective quality service in the pediatric in-patient care area. The fellow will be exposed to the role and interactions with other services the hospitalist service has in providing care (examples: medical sub-specialist, social workers and rehabilitation workers ). Neonatology Contact Person: James Moore Office Number: 404-727-3360 Email: jmoor05@emory.edu Goals and Objectives: Section III 24 Patient Care: The fellow will learn to stabilization and initial management of a newborn at the time of delivery. This skill is important for any unexpected deliveries occurring in the emergency department. Skills include resuscitation methods as well as intubation and vascular access techniques. Medical Knowledge: The fellow will be exposed to special considerations in the management of a newborn including thermoregulation, electrolyte disturbances, infection, early respiratory conditions and congenital anomalies will be discussed. Practiced Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in neonatal resuscitation and will give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Systems Based Practice: The fellow will be exposed to the interactions neonatology has with other hospital services and will develop a better appreciation of the multi-discipline care given to the extreme young. Outpatient Pediatrics Contact Person: Terri McFadden Office Number: 404-785-9500 Email: tmcfadd@emory.edu Goals and Objectives: Patient Care: The fellow will become familiar with the primary management of a wide variety general pediatric conditions and issues including development, immunizations, psychosocial conditions as well as nutrition. The fellow will gain an appreciation for the “follow-up” care once a patient is discharged from the emergency department as well as on-going management of chronic conditions. The fellow should become an integral part of the primary care clinic during their month, functioning as would a senior resident. Medical Knowledge: The fellow should also become familiar with the primary immunization schedule, basic development milestones and common pediatric nutritional conditions focusing especially those that pertain to the practice of pediatric emergency medicine. Practiced Based Learning & Improvement: The fellow will be exposed to a new style of patient management as well as issues not commonly taught in emergency medicine. The fellow should spend time outside the rotation becoming familiar with the those areas that will aid in improving the care they give to patients in the ED such as immunization schedules and basic development. Interpersonal and Communication Skills: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with co-workers and patients. These skills will be part of the formal evaluation at the end of the rotation. Systems Based Practice: The fellow will be exposed to an area of medicine that relays on other services to provide optimum care. The fellow will be exposed to the role and interactions with other services the primary care practitioner has in providing care (examples: medical sub-specialist, social workers, developmental specialist and school administration ). Pediatric Intensive Care (PICU) Contact Person: Nga Pham, MD Office Number: 404-785-1600 Email: nga.pham@choa.org Goals & Objectives: Patient Care: The fellow to learn to manage critically ill and injured children following initial emergency department stabilization. The fellow should become familiar with advanced life-saving procedures such as placement of central lines, Section III 25 cardioversion, BiPAP and other critical care techniques. The fellow should become an integral part of the PICU team and function with the responsibilities as would be expected of a junior fellow in critical care. Medical Knowledge: The fellow should also become familiar with the use and management of advanced care medications, drips and pressors, advanced ventilation techniques, management of critical care conditions such as respiratory failure/severe pulmonary diseases, sepsis/shock, major trauma and severe head injury. Practiced Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in critical care medicine and will be required to give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Interpersonal and Communication Skills: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with co-workers and patients. These skills will be part of the formal evaluation at the end of the rotation. Professionalism: The fellow will be exposed to ethical considerations involved in critically ill patient care including discussions involving the extent of care given and termination of care in select medical conditions. Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess cost effective quality service in critical care medicine. The fellow will be exposed to the role and interactions with other services the critical care service has in providing care (examples: sub-specialists, aid in hospital codes). While only one month is required by the ABP/ACGME, we require our fellows to do a minimum of two months in the PICU during their training. The importance to the emergency physician of knowledge and comfort with advance care procedures and medications is vital. While rotating through the PICU the call schedule will be dictated by the PICU attending. No emergency department responsibilities are expected during this rotation. Orthopedics Contact Person: David Marshall, MD Office Number: (404) 785-6880 Email dgkmarshall@comcast.net Goals & Objectives: Patient Care: During this rotation the fellow should become comfortable with basic and advanced splinting techniques and the emergency department management of common pediatric orthopedic conditions. The fellow should become familiar with special procedures such as arthocentesis. The fellow should also become comfortable with initial management and stabilization of orthopedic conditions with particular focus on the outpatient evaluation and treatment of common overuse injuries. Medical Knowledge: The fellow should become familiar with the diagnosis of common sports related conditions and injuries. The fellow should learn to recognize conditions that can be initially treated in the emergency department by the ER physician (with stabilization and referral to an orthopedic specialist) and those conditions requiring immediate orthopedic consultation. Practice Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in the care of the orthopedic patient and will be required to give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Interpersonal and Communication Skills and Professionalism: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with coworkers and patients. These skills will be part of the formal evaluation at the end of the rotation. Systems Based Practice: The fellow will be exposed to the role and interactions with other services the orthopedic service has in providing care. (examples: cooperative efforts in patient care with the ED, trauma and intensive care follow-up). The fellow will be responsible for limited call on the orthopedic service during this month and will have limited clinical responsibilities in the Pediatric ED. Section III 26 Trauma Contact Person: Grace Roczyki, MD Office Number: (404) 616-5456 Email: grozyck@emory.edu Goals & Objectives: Patient Care: During this rotation the fellow will be an integral part of the trauma team at Grady Memorial Hospital. Under the direction of the trauma service, the fellow will learn to manage both adult and pediatric critically injured patients. The fellow should gain first hand experience in Advanced Trauma Life Support and related techniques. Medical Knowledge: Fellows should learn to manage blunt and penetrating injuries, as well as burns and other traumatic injuries. The fellow should develop the technical and cognitive skills necessary for the stabilization and critical initial management of injured patients. Practice Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in the care of the trauma patient and will be required to give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. The fellow will also take part in morbidity and mortality trauma conferences while on the rotation. Interpersonal and Communication Skills and Professionalism: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with coworkers and patients. These skills will be part of the formal evaluation at the end of the rotation. Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess quality of service in trauma surgery. The fellow will be exposed to the role and interactions with other services the trauma service has in providing care outside the operating room (examples: call for trauma-related patients in the emergency department). The fellow should complete basic the ATLS course prior to this rotation. The call schedule will be decided by the trauma service and there will be no other emergency department requirements during this month. Toxicology Contact Person: Arthur Chang Office Number: (404) 686-3845 aschang@emory.edu Goals and Objectives: Patient Care: The fellow will learn the cognitive skills necessary to critically manage both adults and pediatric toxic exposures (intentional and unintentional). The fellow will function as a member of the toxicology consult service in assessing and managing patients with acute toxic exposures and related illnesses. Medical Knowledge: The fellow should become familiar with common toxidromes, toxicology screens (their clinical utility) and the work-up and management of common exposures. The fellow will become familiar with the poison control center and the extensive resources available (poison index, etc.), and participate in poison center rounds and telephone advice services. Practice Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in the care of the patient with toxic exposure and will be required to give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Interpersonal and Communication Skills and Professionalism: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with coworkers and patients. These skills will be part of the formal evaluation at the end of the rotation. Section III 27 Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess quality of service in toxicology. The fellow will be exposed to the role and interactions with other services and the community the toxicology service has in providing care (examples: community outreach and phone services to the public, as well as consultative services to the hospital). The fellow will not be required to take call during this rotation and will have limited responsibilities in the Pediatric ED during this month. Adult Emergency Medicine Contact Person: Bisan Salhi, MD Office Number: (404) 616-6724 Email: bsalhi@emory.edu Goals & Objectives: Patient Care: The fellow will become familiar with the management of critically ill and injured adult patients. The will allow the fellow the opportunity to manage emergencies in patients outside the pediatric range. The fellow will be an integral part of the resident team of physicians and will take on the responsibilities as might be expected of a mid-senior level emergency department resident. During the second month of this rotation fellows will have the opportunity to concentrate on ultrasound and procedural skills needed in the care of adult patients presenting to the emergency department. By the end of this rotation the fellow should have basic skills in bedside ultrasound (fast exam, vascular access) as well as adult procedures (lumbar punctures, orthopedic reductions, central vascular access, chest tube placement). Medical Knowledge: The fellow should become familiar with the recognition of common adult emergency medicine concerns including myocardial infarction and DVT’s. The pediatric emergency medicine physician will often practice in freestanding pediatric centers and may be called upon when emergencies occur in family members of the pediatric patients throughout the hospital. Adult patients might also present inadvertently to the pediatric emergency center. It therefore becomes vital for the pediatric emergency medicine fellow to become familiar with common adult concerns, initial management and stabilization. Practice Based Learning & Improvement: The fellow will be exposed to new management techniques and improvements in the care of the patient with toxic exposure and will be required to give a brief discussion to the members of the pediatric emergency medicine group at the end of the rotation, on a chosen topic presenting the evidence supporting its use. Interpersonal and Communication Skills and Professionalism: The fellow will have on-going evaluations of his/her ability to work with a team, as well as the ability to both listen and express themselves in an effective manner with coworkers and patients. These skills will be part of the formal evaluation at the end of the rotation. Systems Based Practice: The fellow will be exposed to the methodology specifically used to assess quality of service in adult emergency medicine. The fellow will be exposed to the role and interactions with other services the adult ER service has in providing care. The adult emergency medicine training program will determine call and the fellow will not be responsible for pediatric emergency department call during this rotation. Two months are required. Additional months may be chosen as part of elective time. OUTSIDE ELECTIVES ALL outside electives MUST be arranged BEFORE the start of the rotation. Please have your elective chosen at least two months prior to its beginning and speak with Donna once you’ve Section III 28 made your elective choice. She will be able to set up your elective rotation, provide documentation to the department if necessary, and keep GME up to date on which department you are working with. A written plan of your rotation expectations, with outlined goals, should be turned in to Dr. Lanski and your advisor. If plans are not determined for a rotation in advance, the default rotation will automatically become a PED month. A summary of your elective month must be turned in after the rotation completion. A minimum performance rating of ‘satisfactory’ is mandatory for each monthly rotation (elective or required). Promotion to the next PGY level will require successful completion of ALL rotations throughout the academic year. Unsatisfactory performances in any rotation will not be credited to your training and may require the repeat of that rotation. One (1) attempt to repeat will be offered. An unsuccessful attempt on a repeat rotation will be grounds for suspension from the fellowship program. Please refer to the House Staff Manual of Emory University School of Medicine for overall program guidelines and regulations. This is distributed at residency orientation. You can also go to http://www.med.emory.edu/GME/house_staff_policies.cfm Attending Supervision While in the pediatric emergency department you will be supervised by an attending physician, who will evaluate your patients and will give you feedback regarding your history, physical exam and management plans for each patient you see. Procedures will be taught and supervised with the degree based on fellows experience with that procedure. During limited unsupervised time at the Hughes Spalding ED the Egleston PEM attending will be available by phone for any general questions or concerns. The evening Hughes Spalding attending will be available by phone for any complex questions as well as be immediately available to return to the ED if needed to aid in the management of a patient. Each fellow will have the opportunity to discuss and review all cases of interest with an attending. During outside rotations on-site attending supervision is expected during the day and 24/7 during adult emergency medicine rotations. In other locations, during limited evening hours, minimally attendings will be available immediately by phone for any questions as well as be available to come into the hospital to aid in patient management if needed. Any concerns regarding attending supervision on any rotation should be brought to the attention of the fellowship director to be addressed in a confidential manner. Section III 29 III. FELLOWSHIP SCHEDULES A. Shifts Emergency Pediatric Group fellows are expected to provide services in accordance with the assignment, coverage and on-call schedules. These schedules are designed and/or approved by the Medical Director with guidance from the Advisory Council to ensure that the needs of patients are met in a competent, timely and responsive manner on a continuous basis, twenty-four (24) hours per day, seven (7) days per week. Schedules balance the training and education needs of the fellows. Specific monthly schedules will be prepared prior to the beginning of each fellowship year in order to allow maximum planning time for each fellow. These schedules should be considered final and changes will be made only under special needs or circumstances. B. Schedule Blocks The schedule will be made in 4-week cycles, starting on Monday and ending on Sunday. There are 13 schedule blocks in the year. Year 1: 32 hours/ week during dedicated Emergency department months. 40 hours/ month during research/ elective months. Year 2: 28 hours/ week during dedicated Emergency department months. 40 hours/ month during research/ elective months. Year 3: 32 hours/week during dedicated Emergency department months. 40 hours/ month during research/ elective months. The schedule guarantees a minimum average of one (1) day in seven (7) off, less than 80 hours per week total and at least 10 hours off between shifts. Schedule requests will be submitted along the same time line as the attendings in order for the schedule to come out in a timely fashion. All necessary time off and fellow related time must be submitted with those requests. All time off for vacations and conferences require the fellowship director’s prior approval. This schedule is subject to change based on the clinical needs of the division as well as requirements of the ABP and RRC. Duty hour standards as instituted by ACGME beginning July 1, 2003: Section III An 80-hour weekly limit, averaged over four weeks An adequate rest period, which should consist of 10 hours of rest between duty periods A 24-hour limit on continuous duty, with up to six added hours for continuity of care and education One day in seven free from patient care and educational obligations, averaged over four weeks. In-house call no more than once every three nights, averaged over four weeks Programs can request an increase of up to 8 hours in the weekly hours, if this benefits resident education and is approved by the sponsoring institution and the Residency Review Committee (RRC) 30 Some specialties have more restrictive standards, reflecting patient care and educational demands More detailed information about the duty hour standards is available from the “Resident Duty Hour” page on the ACGME Web site www.acgme.org Monthly TIMESHEETS are a requirement and will be requested throughout the year. Moonlighting Policies Residents enrolled in a graduate medical education program at Emory University School of Medicine are prohibited from providing patient care services that are outside the scope of the residency training program (moonlighting) UNLESS they receive the written approval of their Program Director. To seek approval for moonlighting, residents must submit a signed request to their Program Director. This form can be obtained from the Program Director/Coordinator in the department. A Program Director’s decision to approve or deny a resident’s request will depend on one or more of a variety of factors including, but not limited to, interference with the resident’s responsibilities in the training program, individual circumstances of the requesting resident, legal requirements and total work hours. Residents must abide by the following rules related to moonlighting: Submit a signed copy of the appropriate “Request to Moonlight Form” to the Program Director and receive the Program Director’s approval before moonlighting. Sign a contract with the hospital or other health care facility where the resident will moonlight. The contract must state that the facility is responsible for providing professional liability insurance coverage or that the resident has personally obtained professional liability insurance to moonlight with respect to the services provided during the moonlighting assignment. The residency training program does NOT provide professional or general liability insurance for residents when they perform moonlighting services, even at Emory facilities. Moonlighting services may be performed only in an outpatient setting or emergency department at a hospital that is formally affiliated with the training program. Moonlighting services may also be performed at facilities not affiliated with the training program. Obtain a license to practice medicine in the state where the moonlighting will occur Residents on J-1 visas are prohibited from moonlighting Refrain from wearing anything identifying him/herself as a trainee in Emory’s residency training program when moonlighting outside of Emory-related hospitals. Understand that moonlighting activities that interfere with residency training or have an impact on a resident’s performance in the training program may be grounds for disciplinary action, up to and including termination from the training program. Assure the Program Director that the total hours in the combined education program and the moonlighting commitment DO NOT EXCEED the limits set by the ACGME. Section III 31 Request to Moonlight at a Facility OUTSIDE the Grady or Emory Healthcare System I submit this request to be approved to moonlight during the period ___________________________ (The period may not be longer than six months). I agree to have a valid contract to moonlight at ______________________________ (Name of hospital(s) or other facility). The contract must state that the facility will provide professional liability insurance coverage with respect to the services that I provide during my moonlighting assignment or that I have my own personal professional liability insurance to cover this moonlighting. I am fully licensed to practice medicine in the state where the moonlighting will occur. I am NOT in training on a J-1 Visa. I agree NOT to wear anything identifying me as a trainee in the Emory training program (including, but not limited to, Emory photo ID cards, uniforms, lab coats, etc.). I agree not to exceed any restrictions the training program has regarding the total number of hours I may work per week. I acknowledge any activities, including moonlighting, which interfere with residency training or have an impact on my performance in the training program may be grounds for disciplinary action up to and including my dismissal from the residency program. By signing below, I attest to the completeness and accuracy of the above information. __________________________________________________ Signature of resident requesting permission to moonlight ____________________ Date __________________________________________________ Print name of resident/PGY Request for moonlighting is is not (circle one) approved. ___________________________________________________ Signature of Program Director Section III ______________________ Date 32 IV. EVALUATIONS The ACGME considers a formal methods of evaluation to be key elements in certification according to recent statements on curriculum for Pediatric Emergency Medicine. Necessary documentation must include: A. Technical Skills It is your responsibility to document ALL procedures (patient’s name, medical record number, date of procedure, complications) and to maintain a comprehensive list of these procedures for your file. You will be required to produce this documentation at each of your semi-annual reviews and at the completion of the fellowship program. B. Monthly Evaluations Each month you will be evaluated by one of these: a. b. c. d. your research mentor if you are on a research month resident coordinator if you are doing anything other than a PEM month PEM attendings if you are doing a PEM month residents that you work with during your PEM month C. Semi-Annual Evaluations Every six months a critique will be done regarding your abilities in patient care, technical skills, teaching, consultations, note writing, and personal interaction with faculty and staff. Your ability to incorporate existing literature into your practice as well as your ability to work within the local healthcare system will be addressed as well. In addition, evaluations from the supervisors of your nonpediatric emergency medicine rotations and electives and from research mentors will be reviewed, as well as evaluations on the lectures you have given. Your procedure log will be due at this time. Fellows will also have the opportunity each year to anonymously complete evaluations of PEM faculty as well as the fellowship program. If, at any point during fellowship, you have a concern or issue relating to a rotation or attending (from our division or any other) it should be immediately brought to the attention of the Fellowship or Division Director. We encourage you to be as open and constructively critical as possible. Nearly all evaluation documentation takes place online. You will be provided a pass code and required to evaluate lectures, residents, and other parts of the program. It is important that you follow through on these evaluations. You will be learning the art of critiquing others, plus it is only fair that you evaluate them. They will be evaluating YOU! Section IV 1 V. RESEARCH C. Mentor Meetings Before each research month you will choose and meet with your mentor to discuss the plan and progress of your research project. A meeting with the division’s academic director, Dr. Simon, may occur as well on a as needed basis. You may also meet often with the research coordinator. D. Scholarship Oversight Committee Progress through the fellowship program will be monitored by the SOC. The SOC consists of 3 members (1 not a member of the PEM division) and meets individually with each fellow on a semiannual basis in order to evaluate the fellow’s progress and assess whether he/she is satisfactorily meeting APB established guidelines and will qualify to apply for subspecialty board certification on completion of the fellowship. The SOC reviews the fellow’s scholarly works to ascertain that he/she is completing project tasks and requirements in a timely manner. Each fellow will provide an agenda for the SOC meeting outlying the work done and future plans in the areas of research, administration and teaching. After each meeting the fellow will provide each SOC member a copy of the meeting minutes which will reflect the discussion during the SOC meeting. This should be sent to the members within 2 week of the meeting. Year 1: At minimum the fellow should have articulated a research question, identified research mentors and preformed an in-depth review of current literature pertaining to the proposed project and outlined methodology and a general timeline for completing the project. Submission of the project to the IRB should be accomplished before the end of the fellows 1st year. If this is not the case, the fellow and mentors will meet to discuss the situation and determine methods to accomplish this goal. Year 2: The fellow should be actively engaged in data collection and analysis of their research project. Minimally, an abstract should be completed and presented as well as a manuscript submitted by the second half of the second year. A second project should be developed and submitted by the end of their 2nd year as well. Year 3: The fellow should have started a second project, which was developed at the end of their second year. A second manuscript should be prepared and submitted to a peer-reviewed journal by April of the fellows 3rd year. Section IV 2 V. CONFERENCES Attendance at educational conferences by the fellow is vital to that individual’s educational experience. A. Division of Pediatric Emergency Medicine Core Fellowship and Educational Conference This mandatory conference is held weekly on Wednesdays at the Tullie office. This is the core didactic educational component of the fellowship. It also serves as a continuing educational forum for attendings, staff and other trainees. It allows for significant didactic interaction between trainees and other members of the division. Each session is centered on a primary lecture and topic taken from a core list of items to be covered every three years, as well as lectures on ED management, case conferences (morbidity and mortality), and topics of recent interest to trainees. The primary presenter is a subspecialty resident, a divisional or departmental attending, or an outside lecturer or guest. In addition to the core component, pediatric emergency medicine residents are responsible for presenting one of the following each week: journal club, procedure of the week, board review, case/topic presentation or journal review. Journal club consists of critiquing one or two journal articles covering areas such as study design, methods, results and statistics and determining whether or not a study is well done and relevant. Journal club presents pertinent literature on various controversial topics in order to promote discussion and enable residents to make sound decisions on the emergency department based on this insight. The procedure of the week is presented to review when and how to perform various procedures and discuss techniques for rarely performed procedures. Board review is a question and answer session taken using pediatric emergency medicine selfassessment and review texts to test the residents’ fund of knowledge and promote discussion of the types of questions that might be on the Board Exam. Case/topic presentation is an opportunity for subspecialty residents to present various topics in a formal format in order to build a core of lectures to use in other forums in the future. The presenter/lecture is evaluated according to content, style, presentation, and overall effectiveness of the lecture. Journal review is a presentation summary of recent journal articles pertinent to the practice of pediatric emergency medicine. Research issues including project design, data collection, statistical analysis, funding, abstract presentation, and manuscript presentation are also covered during this conference. Other items covered include review of fellowship applications and candidates by the entire group and updates on any clinical or administrative issues which the fellows or attendings want addressed. Section IV 3 B. Department of Pediatrics Grand Rounds: Grand Rounds at Egleston occur weekly on Wednesday mornings at 7:30 am in the B-52 Auditorium. Conferences cover a wide range of topics including both general and subspecialty pediatrics. Lecturers include attendings and staff of the hospital and the department of pediatrics including those from the division of emergency medicine. Frequently, guest lecturers from outside the institutions lead these sessions. This forum brings together attendings, community physicians, and trainees for continuing medical education. Sessions are taped and available for review in the hospital library. For the listing of upcoming Grand Rounds go to: http://www.choa.org/default.aspx?id=3040 Grand rounds at Hughes Spalding are sponsored by the Grady Healthcare System and the Department of Pediatrics and Emory University. The meetings occur weekly on Thursday mornings at 8:00 at in the Steiner Auditorum. Conferences are set up as case presentations with active participation of attendees in coming up with a broad differential diagnosis. Cases are often generated from those presenting to the emergency center at Hughes Spalding. Attendings and trainees, including those from the division of Pediatric Emergency Medicine, often provide wrap-up discussions on the case. C. Department Pediatrics Fellows’ Conference: The Departmental Fellows’ Conference, sponsored by the Department of Pediatrics, meets weekly on Tuesday afternoons during the latter part of the academic year. The conference provides a forum for fellows in all divisions to present their research. Research is presented in various stages of development, and the conference provides valuable feedback to subspecialty residents from attendings and other residents from the training program. Fellows from all levels of training benefit from this forum. The final conference in the series consists of a Department Research Competition for fellows. There are also sessions dedicated to teaching, evaluation of presentations, and even a teaching competition for fellows of the Department of Pediatrics. D. Department of Pediatrics Fellows’ Research Course: An introduction to research methodology and design. It includes discussions on experimental design, research techniques, data collection and analysis, grant writing, ethics in research, and abstract and manuscript preparation. This course is meant to lay a common foundation in research for all subspecialty residents in the Department of Pediatrics. Presentations occur by faculty members or administrators of the Department of Pediatrics, the Rollins School of Public Health, and other members of Emory University. E. Adult Emergency Medicine Resident Conference: This weekly conference is held on Tuesday mornings at 8:00 in the Steiner Auditorium on the Grady campus. Topics cover all aspects of emergency medicine. The Pediatric Emergency Medicine residents participate in topic discussions, case presentation discussions, and question/answer board review sessions. Once a month a pediatric session is held and presented by the division of Pediatric Emergency Medicine. The Pediatric Emergency Medicine residents participate in presenting pediatric topics to the Adult medicine residents. Section IV 4 F. Division of Pediatric Emergency Medicine Administrative Meeting: This meeting is held on the second Wednesday of every month at 9:30 am in the conference room at Tullie. Discussions include clinical care, research, leadership, peer review and topics relating to fellowship. Fellows are encouraged to participate in order to learn the administrative aspects of running the emergency centers. Each fellow is required to attend the meeting unless unavailable due to outside rotation conflict. The meeting is also a forum in which interesting cases, radiographs, quality assurance issues and chart reviews are discussed. The subspecialty residents, as well as nursing staff and other hospital administrators, participate in this open forum. G. Department of Pediatrics Resident Noon Conference: These conferences are held several times each week at both Children’s Healthcare of Atlanta at Egleston and Hughes Spalding Children’s Hospitals. Various topics from the faculty are presented and discussed. Pediatric Emergency Medicine residents periodically present lectures in order to teach the Pediatric residents in a formal didactic session. H. Pediatric Surgery/Trauma Conference: The division of Pediatric Surgery holds a weekly conference at 7:30 am Friday mornings in the B52-Auditorium at Egleston. Surgery residents and attendings present and review common pediatric surgical and trauma related issues. This meeting occurs as part of the Children’s Healthcare of Atlanta trauma committee meeting and is open for participation by Pediatric Emergency Medicine residents. J. Response to non-attendance and/or late arrival to the above meetings Attendance at the weekly PEM fellows’ conference and the Department of Pediatrics fellows’ conferences are mandatory unless you are on a clinical rotation that creates a conflict with scheduling. The other conferences should be attended whenever possible. While some conferences are not mandatory, attendance and participation, whenever possible, will greatly enhance your fellowship experience. For a complete daily schedule of lectures, committee meetings and events at Egleston go to: http://www.choa.org/default.aspx?id=3044 For a complete daily schedule of lectures, committee meetings and events at Grady go to: http://r25web.cc.emory.edu/MedGR_servlet/urd/run/wv_event.DayList?evdt=20070604,evfilter=10886 8,ebdviewmode=grid Section IV 5 FELLOWS LECTURE SERIES – CURRICULUM OVERVIEW Lecture: Airway Management Procedure: Intubation/Cricothyroidotomy Article Review: Airway Management Lecture: Shock Procedure: Intraoseous line/femoral central line Article Review: Shock Management Lecture: Neonatal Resuscitation Procedure: Umbilical Vessel Catheterization Article Review: Lecture: Sedation & Analgesia in the ED Procedure: Nerve Blocks Article Review: Conscious Sedation Lecture: C-Spine Evaluation/Trauma Procedure: C-Collar Removal Article Review: C-Spine Evaluation Lecture: Prehospital care and transport medicine for pediatrics Procedure: Nerve Blocks Article Review: Prehospital Care Lecture: Major Pediatric Trauma Procedure: ATLS surveys Article Review: Lecture: Asthma Management of the ED Procedure: Article Review: Asthma Related Lecture: Syncope Procedure: ECG Reading Exercise Article Review: Prolonged QT Syndrome Lecture: Dehydration Procedure: Subclavian central line placement Article Review: Dehydration Management Lecture: Seizures – Status and Febrile Procedure: Article Review: Status Management Section IV 6 Lecture: Meningitis Procedure: Lumbar Puncture Article Review: Meningitis Lecture: Detoxification Methods Procedure: NG/OG Placement Article Review: Whole Bowel Irrigation in Children Lecture: Cardiac Emergencies – Arrhythmias Procedure: Vagal Maneuvers/Defibrillation Article Review: Verapamil/Adenosine in Pediatrics Lecture: GI Bleeding in Pediatrics Procedure: Guiac, Rectal Exam Article Review: Lecture: Oncologic Emergencies Procedure: Central Line Access Article Review: Lecture: Toxicology – Summer Poisonings Procedure: Article Review: Toxicology Lecture: Otitis Media Procedure: Tympanocentecis Article Review: Otitis Media Management Lecture: Cardiac Emergencies – CHD/transplant Procedure: Article Review: Lecture: Seizures – Pediatric Burns Procedure: Burn Cleaning Article Review: Lecture: Seizures – Hematologic Emergencies (except SCD) Procedure: Article Review: Lecture: Seizures – Surgical Abdomen Procedure: Article Review: Lecture: Seizures – Household Poisonings Procedure: Article Review: Section IV 7 Lecture: Seizures – Tylenol/ASA Poisoning Procedure: Article Review: Mucomyst with Charcoal Lecture: ENT Emergencies Procedure: Article Review: Peritonsilar Abscess Management Lecture: Rashes Procedure: Article Review: Lecture: Urologic Emergencies Procedure: Hernia Reduction Article Review: Lecture: Ophthalmologic Emergencies Procedure: Fundoscopy, Slit Lamp Exam Article Review: Lecture: VOP in SCD Procedure: Article Review: Lecture: STD’s Procedure: Pelvic Exam Article Review: Outpatient PID Management Lecture: Limp Procedure: Arthrocentecis Article Review: Lecture: Wound Care/Bites Procedure: Wound Irrigation/Sutures/Dermabond Article Review: Lecture: Dental Emergencies Procedure: Avulsed Tooth Article Review: Lecture: Hypertension in the ED Procedure: Article Review: Lecture: Vaginal Bleeding Procedure: PAP Test Article Review: Section IV 8 Lecture: Headache Procedure: Article Review: Lecture: HIV in the ED Procedure: Article Review: Lecture: SCD Complications: Sepsis and Strokes Procedure: Article Review: Lecture: Hematuria Procedure: Article Review: Lecture: Cystic Fibrosis Procedure: Suctioning Article Review: Lecture: Malfunctioning Ventricular Shunt Procedure: Shunt Tap Article Review: Lecture: PID Procedure: Wet Mount Article Review: PID Complications Lecture: Dizziness/Ataxia Procedure: Article Review: Lecture: Toxicology- Alcohols Procedure: Article Review: Lecture: Endocrinologic Emergencies except DKA Procedure: Article Review: Lecture: Rape Evaluation Procedure: Georgia Rape Kit Article Review: Lecture: Nephrotic Syn/HUS/HSP Procedure: Paracentecis Article Review: Section IV 9 Lecture: Neck Masses Procedure: Abscess ID Article Review: Lecture: Back Pain Procedure: Article Review: Lecture: Biologic Terrorism Procedure: Article Review: Lecture: Business of Emergency Medicine (Flow) Procedure: Article Review: Lecture: Radiation Injury Procedure: Article Review: Lecture: Psychiatric Emergencies Procedure: Article Review: Lecture: Child Abuse and Neglect Procedure: Article Review: Lecture: Barotrauma/Altitude Sickness Procedure: Article Review: Lecture: Drowning Procedure: Article Review: Lecture: Business of Emergency Medicine (Customer Satisfaction) Procedure: Article Review: Lecture: Electrolyte Disorders Procedure: Article Review: Lecture: Toxicology – Antihistimine/Antihypertensives/INH) Procedure: Article Review: Section IV 10 Lecture: Looking for a Job in a PED Procedure: Article Review: Lecture: Rheumatologic Emergencies (SLE, JRA, Kawasaki) Procedure: Article Review: Lecture: Business of Emergency Medicine Procedure: Article Review: Lecture: Chemical Warfare Procedure: Article Review: Lecture: Anaphylaxis Procedure: Article Review: Lecture: Pancreatitis Procedure: Article Review: Lecture: Drowning/Immersion Injuries Procedure: Article Review: Lecture: Smoke Inhalation/Co Poisoning Procedure: Article Review: Lecture: Inflammatory Bowel Disease Procedure: Article Review: Lecture: Toxicology- Grieving Process in the ED Procedure: Article Review: Lecture: Upper Extremity Fractures Procedure: Upper Extremity Splints Article Review: Lecture: Inborn Errors of Metabolism in the ED Procedure: Article Review: Section IV 11 Lecture: GU Trauma Procedure: Article Review: Lecture: ENT Trauma Procedure: Article Review: Lecture: Compartment Syndromes Procedure: Article Review: Lecture: Pelvic/Spine Fractures Procedure: Article Review: Lecture: Billing Procedure: Article Review: Lecture: Abdominal Trauma Procedure: DPL Article Review: Lecture: Conference Presentations Procedure: Article Review: Lecture: Sleep deprivation and Work Life balance Procedure: Article Review: Section IV 12 VI. OTHER RESPONSIBILITIES Research Responsibilities Research is an integral component of this fellowship. While every effort will be made to provide you with a worthwhile research experience; it is your responsibility to translate this opportunity into concrete results. Current specialty board criteria require a fellow demonstrate “competence” in research to become board eligible. We will define research competence as the completion of at least one “research quality” manuscript accepted for publication in a peer reviewed journal. It is expected that you will complete at least one project as the primary author during your fellowship. It is also expected that you will be involved in other projects as a contributing author. Administrative Responsibilities Fellows are an important part of the division for three years. We encourage you to become involved and contribute to clinical, administrative and social activities. We expect active participation in committees, meetings and administrative tasks throughout your fellowship. You will also be expected to participate actively during the fellowship candidate interview season (from late August through October). Your input is vital in choosing and ranking candidates for the following year. During your first year you may be asked to join candidates for lunch or take them on tours of the hospitals. During subsequent years you may be asked to interview candidates one on one. This is good practice in building interview skills. All current fellows are required to participate during the candidate ranking meeting and provide feedback on candidates that they have met with. Teaching Responsibilities If one accepts the notion that fellows should be at the peak of their academic involvement, then it makes sense that they will have much to offer other health care providers. Moreover, it is important to develop the ability to communicate to groups of various sizes and backgrounds. Lecturing and teaching will be a vital part of your fellowship experience. Section IV 13 VII. GENERAL INFORMATION A. Payroll, Benefits, and Income Tax Forms Please refer to your Emory Orientation packets or contact Human Resources: Emory Human Resources – 404-727-7611 http://emory.hr.edu/forms.nsf/(title)/Residency+Training+Program+Forms+&+Brochures B. Identification Badges & Numbers Identification badges will be issued at the beginning of the year. They should be worn at all times when on CHOA and/or hospital properties. Visit the security office on the ground floor of Children’s Healthcare of Atlanta at Egleston Hospital (404-785-0428) to obtain your CHOA/Egleston ID badge. Make certain the first line of the badge states your name as Dr. (your last name) and the second line states your whole name (first name, last name, MD). Your title is Fellow, Pediatric Emergency Medicine. To have this badge activated for access to the 1645 Tullie Circle building, please go to Security in the CHOA office park (1680 Tullie). At the badge office on the ground floor of the alumni center next to Emory University Hospital, you will be able to receive your Emory ID. Contact 404-727-5658 if you have any questions. C. Parking Facilities Fellows are assigned parking spaces in the main Children’s Healthcare of Atlanta at Egleston garage. A key card is required for entrance to the parking deck. Parking is provided free of charge. The card can be obtained from the Children’s Healthcare of Atlanta at Egleston security office. Be sure to ask for a parking spot in the Children’s Healthcare of Atlanta at Egleston Deck, not on the Michael Street Deck. Parking is available at Hughes Spalding as well. There is an $18.00 per month fee that is deducted directly from your paycheck. Visit the parking office which is behind the hospital to obtain your parking tag. The one-time cost for the card is $10.00 (cash only). D. Mailboxes Mailboxes are located in the 1645 office. Outgoing mail can be dropped in the basket on the counter across from the copy machine. Mail to you should be addressed to either: Division of Pediatric Emergency Medicine, Children’s Healthcare of Atlanta at Egleston, 1405 Clifton Road, NE, Atlanta, Georgia 30322 OR 1645 Tullie Circle, Atlanta, GA 30329 Section IV 14 E. Email: Email accounts will be set up for you for both Emory and CHOA. Nearly all divisional mail will be sent via the Emory account. Please check your email often as we consider it a primary communication source and important information is shared between on a constant basis. F. Pager Fellows receive their own pager and keep it for the duration of the fellowship. Fellows are responsible for their pagers and there is a fee to replace lost pagers. Visit the office of Graduate Medical Education to get your pager. This office is located on the ground floor of the Woodruff Science Bldg. across from Egleston Hospital. Replacement batteries for pagers can be obtained from Donna at the PEM office at Tullie. G. Medical License All residents must have a Temporary Postgraduate Training Permit or a Medical License from the State of Georgia to participate in the Emory University School of Medicine Residency Training Program. A copy of the current GA Training Permit or Medical License must in the GME office before your program begins. Residents are not permitted to provide clinical care unless they have their permit or license. Residents/Fellows (PGY1-PGY7) will be reimbursed by the GME office up to $100.00 to obtain a Temporary Postgraduate Training Permit to practice as a resident in facilities associated with Emory University School of Medicine Residency Training Program. You will be reimbursed $50.00 to RENEW your training permits. You WILL NOT be reimbursed the cost to issue a new training permit if you allow the permit to lapse. If you (PGY1-PGY7) elect to obtain a Georgia Medical License instead of a Postgraduate Training Permit, you will be reimbursed up to $100.00 toward the cost. If you have a Georgia Postgraduate Training Permit and elect to obtain a Georgia Medical License, there will be no additional reimbursement. The GME office will NOT reimburse residents who obtain a Georgia Medical License in order to moonlight. To receive reimbursement for a permit when processed directly, residents must provide the GME office with a photocopy (both sides) of the personal check used to obtain a Georgia Training Permit and a photocopy of the permit. Once a permit is obtained you must maintain its validity throughout your training period in order to participate in the Emory University School of Medicine Training Program. Failure to do so will result in disciplinary action up to and including termination from the training program. Section IV 15 For information on obtaining permits and licensure contact the Composite State Board of Medicine Examiners: www.medicalboard.state.ga.us If you have any questions concerning your license, contact Dr. Lanski, Donna Stringfellow or Jeanette Carter in the GME office at (404) 727-5658. H. Documents Necessary For Your File: Upon beginning your fellowship, you will need to provide Donna with a copy of your GA. medical license or training permit, current DEA, any board certificates, and your most recent PALS card, as well as ATLS and ACLS if you have them, as soon as possible. I. Malpractice Insurance Coverage is provided for activities that are officially part of your fellowship training. J. Physical Exam GME must be provided with documentation indicating vaccinations or serologic data showing immunity to the following: MMR (rubeola, mumps, rubella) – 2 doses if born after 1957 Diphtheria – Tetanus – with the past 10 years Hepatitis B (3-dose series) Chickenpox This information must come from the student health service at the medical school you attended, from your personal physician or from a county health department. Residents MUST have a PPD skin test completed within 12 weeks prior to the start of training at Emory, and must provide proof of such a skin test to GME. K. Copying Facilities There is a copy machine available at the Tullie office for use for fellowship related duties. L. Library Facilities The Emory University School of Medicine library is the main library serving the entire medical center. Library cards may be obtained there with your identification card. The library is located on Clifton Road near the Rollins Research Building. Copy cards are available at the library. Section IV 16 Computer access to all Emory on-line resources is available at the Health Science Library at www.emory.edu/WHSCL/ Emory on-line software for free internet access is available through the division or the Health Science Center. Children’s Healthcare contains a relatively complete pediatric library on the ground floor of the hospital. It provides online searches and an Interlibrary Loan service for books, journal articles or audiovisual materials not available in the libraries. You are welcome to copy materials in the library at no charge (50-page limit). Requests for searches or information can be called in to 404-785-6438 or faxed to 404-785-6463. http://careforce/cms/default.aspx?id=441 http://ejournals.emory.edu/ http://pubs.ama-assn.org/ http://www.emory.edu/libraries.cfm http://www.healthlibrary.emory.edu/ http://gateway.ovid.com/ M. Vacation Postdoctoral fellows are allotted 3 weeks vacation per academic year. General vacation time cannot be taken during the dedicated during PICU, Trauma or Adult Emergency Medicine months. Unused vacation time does not transfer to the following year. N. Meetings Fellows may receive funding to attend academic meetings at which they present abstracts. Suggested meetings include the ACEP and AAP fall or spring meetings, the SPR/APS/APA and SAEM meetings or specific scientific meetings germane to your area of research. One of the meetings should include the Fall AAP or the spring SPR/APS/APA to allow for networking and meeting with potential employers. You may attend other meetings at which you do not make presentations (with divisional approval and in the absence of scheduling conflicts) at your own expense. In order to procure divisional funds to support your attendance at a meeting, the following must occur: Obtain printed meeting information including dates and costs. Discuss selected meeting with your designated mentor to assure appropriateness and benefit of the meeting for either your research or clinical needs. Obtain scheduling approval from Dr. Lanski. Submit a copy of meeting information to the fellowship director, Dr. Lanski for final approval at least two months (60 days) prior to the meeting. Meetings will be subject to final approval by the Division Director. Children’s Healthcare of Atlanta maintains a travel service for reimbursable trips. Contact Debra Busby for travel arrangements and reimbursements. Section IV 17 O. Book Money A stipend of $150.00 is provided to each fellow for purchase of appropriate critical care or research related textbooks or reference material. Receipts must be obtained and provided to Debra Busby for reimbursement with fellowship director approval. In addition, an up to date library with most major pediatric emergency medicine journals, and emergency medicine text books are available in the administrative offices of the division of emergency medicine. P. Long Distance Phone Calls An authorization code for long distance phone calls and faxes is required. Please see Donna or Debra to receive your code. Q. Presentation Making Making a good presentation is a necessary skill during fellowship. Donna will be happy to help you create, find and scan pictures for, and computerize your presentations. We currently have the equipment (scanner, LCD projector) to create completely computerized presentations. VIII. SUMMARY While demanding, the fellowship should be one of the most rewarding experiences of your career. You will develop all of the necessary skills for the care of ill and injured children, and you will develop the clinical, teaching, research and administrative skills necessary to become an outstanding Pediatric Emergency Medicine Physician. It is the goal of the program and all of us in the PEM Division to assist and guide you through the process. Section IV 18