Principles of delay
advertisement
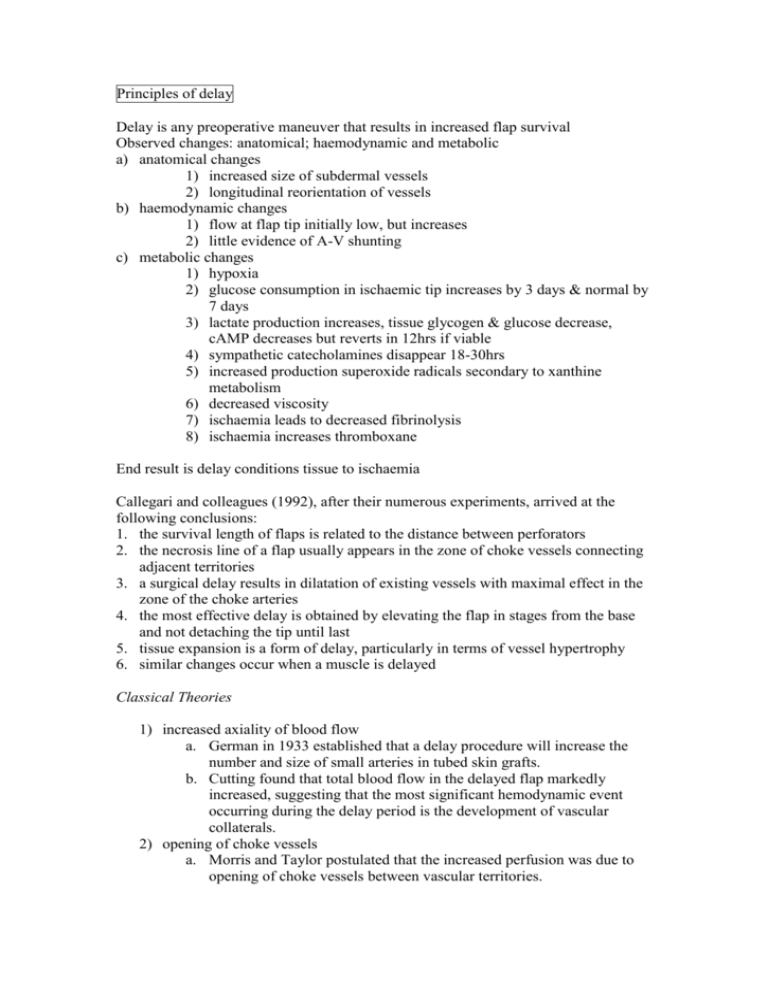
Principles of delay Delay is any preoperative maneuver that results in increased flap survival Observed changes: anatomical; haemodynamic and metabolic a) anatomical changes 1) increased size of subdermal vessels 2) longitudinal reorientation of vessels b) haemodynamic changes 1) flow at flap tip initially low, but increases 2) little evidence of A-V shunting c) metabolic changes 1) hypoxia 2) glucose consumption in ischaemic tip increases by 3 days & normal by 7 days 3) lactate production increases, tissue glycogen & glucose decrease, cAMP decreases but reverts in 12hrs if viable 4) sympathetic catecholamines disappear 18-30hrs 5) increased production superoxide radicals secondary to xanthine metabolism 6) decreased viscosity 7) ischaemia leads to decreased fibrinolysis 8) ischaemia increases thromboxane End result is delay conditions tissue to ischaemia Callegari and colleagues (1992), after their numerous experiments, arrived at the following conclusions: 1. the survival length of flaps is related to the distance between perforators 2. the necrosis line of a flap usually appears in the zone of choke vessels connecting adjacent territories 3. a surgical delay results in dilatation of existing vessels with maximal effect in the zone of the choke arteries 4. the most effective delay is obtained by elevating the flap in stages from the base and not detaching the tip until last 5. tissue expansion is a form of delay, particularly in terms of vessel hypertrophy 6. similar changes occur when a muscle is delayed Classical Theories 1) increased axiality of blood flow a. German in 1933 established that a delay procedure will increase the number and size of small arteries in tubed skin grafts. b. Cutting found that total blood flow in the delayed flap markedly increased, suggesting that the most significant hemodynamic event occurring during the delay period is the development of vascular collaterals. 2) opening of choke vessels a. Morris and Taylor postulated that the increased perfusion was due to opening of choke vessels between vascular territories. 3) 4) 5) 6) 7) b. They found that the maximal effect of this perfusion change occurred between 48 and 72 hours after surgical delay. c. histologic analysis revealed an increase in the diameter of the vessels and a decrease in vessel wall thickness compared with the control vessels. d. Stages i. Vessel spasms for 3 hours ii. Increased caliber of choke vessels with wall thinning (24-72 hours) iii. Dilation and thickening of wall (72hrs-1 week) iv. Choke vessels open permanently Tolerance to ischaemia a. In 1965, McFarlane stated that the delay procedure conditions flaps to survive on diminished nutrient blood flow, resulting in increased flap survival. b. In 1972, Myers theorized that the improvement in flap circulation was dependent on the degree of ischemia produced by the initial delay procedure. c. Now known to be mediated by heat shock proteins Sympathectomy vasodilatation theory a. Divided sympathetics at the borders of the flap b. Does not explain why maximal effect is delayed and why delay requires weeks. Interflap shunting hypothesis a. Sympathectomy dilates the AVAs more than precapillary sphincters resulting in increased blood bypass b. Delay results in less sympathetic fibers cut and therefore less of a reduction in non-nutritive flow Hyperadrenergic state a. Surgery results in rise in local and systemic vasoconstrictive substances (Adrenaline and noradrenaline) b. As the effect of these chemicals gradually diminishes (4 to 12 hours), vessels in the flap begin to dilate. Over the next 24 to 72 hours, an active process further dilates the vessels. Unifying theory (Pearl 1981) a. elevation of flap produces a hyperadrenergic state lasting 18-30 hrs. b. This results in vasoconstriction. c. Recovery from hyperadrenergic state follows over next few days as the flap is exhausted of noradrenaline. Thus when flap finally elevated, adverse vasoconstriction is avoided. Current Theory Induction of Heat Shock Proteins Supraphysiologic stress induces a heat shock response, which may exert protection against ischemic necrosis. Delay preconditions the tissue at risk prior to surgery to induce heat shock proteins (HSPs) by exposure to physical or pharmacologic stressor Experimentally, the heat shock response has been demonstrated to have a positive effect on flap survival by protecting tissue from ischemia or ischemia–reperfusion injury. HSPs are a superfamily of highly conserved intracellular proteins that protect cells and whole organisms from various stresses. Mechanism of action 1) Tolerance to ischaemia a. act as molecular chaperones, escorting proteins targeted for other cellular compartments b. prevent misfolding of newly synthesized proteins 2) improving microcirculatory blood flow on an arteriolar and capillary level a. vasodilatory action of carbon monoxide Of interest are heat-shock protein (HSP) 70 and HSP-32 [haem oxygenase 1] HSP-32 has been identified as heme oxygenase (HO)-1, the rate-limiting enzyme in the catabolism of heme to biliverdin, free iron, and carbon monoxide. HSP-32 is the main endogenous source of carbon monoxide In mouse studies, induction of HSP-32 after repetitive local heat preconditioning of the skin significantly preserves endangered myocutaneous ischemic tissue from apoptotic and necrotic cell death. This protection from ischemic tissue loss seems to be the result of the HSP-32mediated vasoactive action of carbon monoxide, improving microcirculatory blood flow on an arteriolar and capillary level rather than increasing ischemic tolerance of the tissue. Delay may be 1) Surgical a. Dividing margins of flap b. Classically, lateral borders are divided and flap totally undermined (bipedicled flap) 2) Vascular a. Dividing perforators/axial vessels 3) Laser 4) Chemical a. Alpha-adrenoreceptor blocker i. Phenoxybenzamine ii. Phentolamine iii. Daxozocin b. Adrenergic neuron blocking i. Guanethidine c. Noradrenaline depletion i. Reserpine d. Free radical scavengers i. Superoxide dismutase ii. Allupurinol e. Cytokines i. VEGF 1. preoperative intramuscular injection of VEGF increases skin paddle survival (rat model) alone or in conjunction with surgical delay