Carpal Tunnel Syndrome
advertisement

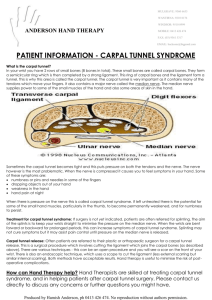
CARPAL TUNNEL SYNDROME clinical syndrome manifested by characteristic signs and symptoms resulting from an entrapment neuropathy of the median nerve at the wrist most common compression neuropathy in the upper extremity. Anatomy Space enclosed by the concavity of the carpus and the overlying flexor retinaculum Flexor retinaculum has 3 components deep forearm fascia (deep to FCR and FCU) transverse carpal ligament distal aponeurosis between thenar and hypothenar muscles Mean width 25mm at proximal end 20mm at the narrowest region at the level of the hook of hamate 26mm at the distal end Mean widening of the transverse carpal arch after carpal tunnel release is 10.4% or 2.7 mm Volume measure 5ml. Generally smaller in females Contents 4 tendons of flexor digitorum superficialis (FDS) 4 tendons of flexor digitorum profundus (FDP) All 8 share a common synovial sheath – Ulnar bursa. The sheath does not invest them completely but is reflected/open from the radial side. Arteries gain access to the tendons at these points 1 tendon of flexor pollicis longus, median nerve Other structures Palmaris profundus arises from the interosseus membrane in the forearm and passes through the carpal tunnel to insert onto the dorsal surface of the palmar aponeurosis. Rare finding. Reported in 1:1600 dissections Lumbricals usually originate form FDP tendons distal to the tunnel, but when fingers are flexed they may be pulled back into the tunnel Small persistent median artery – dominant blood supply to median nerve in 30% and may significantly contribute to blood supply of index and middle fingers Anomalous palmar cutaneous branch MRI distal cross section Transverse Carpal ligament Medial – pisiform and hamate ( hook and radial surface) Lateral – scaphoid tuberosity and medial surface/ridge of trapezium. Integrity of the TCL is not a major factor in the maintenance of the carpal arch. Palmar cutaneous nerve From radiopalmar aspect of nerve, 5cm proximal to wrist crease Separates from main nerve after 2cm and travels underneath antebrachial fascia between PL and FCR Emerges through fascia 0.8cm proximal to wrist crease and divides into radial and ulnar branches Median Nerve Enters the canal in the middle or slightly to the radial side of midline, directly under or dorso-radial to the palmaris longus tendon Enclosed by a parietal and visceral layers of loose connective tissue. This allows it to shift as the hand changes position. Shape of the nerve varies as is passes through the tunnel. It starts out oval and then flattens out. With the wrist in a neutral position, the median nerve is seen anterior to the flexor digitorum superficialis tendon of the index finger or posterolaterally between the flexor digitorum tendon of the index finger and flexor pollicis longus tendon. May move as much as 20mm in flexion-extension The nerve can sometimes be split by an accessory lumbrical or the median artery. The division may be equal or unequal. Sometimes they rejoin distally. Motor fascicles are generally on the radial side. 78% of cases motor fascicles occupy radiopalmar position in the nerve, 22% in central palmar portion Divides into 6 branches distally – recurrent, 2 common and 3 proper 1st lumbrical supplied by radial side proper digital nerve to IF, 2nd lumbrical supplied by common digital nerve to 2nd cleft In 56%, the thenar branch travels in a separate fascial tunnel. The thenar branch commonly comes off distal to the TCL(extraligamentous). Sometimes it branches off within the tunnel (subligamentous) and sometimes it perforates the TCL in its own tunnel (transligamentous). A – Extraligamentous and recurrent (most common 45-90%) B – Subligamentous (31%) C – Transligamentous (23%) D – Originate from ulnar border of median nerve E – Lie on top of TCL Topographical landmarks 1. Distal wrist crease is the proximal origin of the transverse carpal ligament (TCL). The proximal wrist crease corresponds to the radiocarpal joint. 2. Kaplan’s cardinal line – line drawn parallel to the ulnar side of the abducted thumb and the hypothenar space. 3. The distal end of TCL is at the intersection of the cardinal line and the line of the ring finger axis. 4. Superficial palmar arch lies 5mm distal to the above point. 5. Hook of hamate is 1cm distal and radial to the pisiform. 6. Kaplan’s landmark is the intersection of the cardinal line and a line drawn from index/middle finger interspace. This point identifies the motor branch of the median nerve. History 1854 - Sir James Paget first reported median nerve compression at the wrist following a distal radius fracture 1913 - Pierre Marie and Charles Foix described the pathology of median nerve compression underneath the transverse carpal ligament 1924- Galloway and Mackinnon in Winnipeg, Canada, did the first TCL release in a patient with a posttraumatic neuropathy. Complicated by neuroma of PCN 1933 - Sir James Learmonth reported TCL release to treat median nerve compression at the wrist. 1951 – Phalen advocated transverse incision at the distal wrist crease, with proximal and distal extension as needed 1970 – Taleisnik popularised vertical incision in line with 4th ray Epidemiology Prevalence 1-5% of general population prevalence among working individuals is somewhat lower, about 0.5% - suggests that the majority of cases occur in the non-working population 50% bilateral F>M 3-5:1 o relationships between CTS and women (OC use, menstrual disorders, and obesity) may be related to pressure on the median nerve due to fat or edema near the carpal tunnel. Most common 4th to 6th decades of life Risk factors 1. female sex 2. obesity (BMI>30) 3. age 41-60 4. diabetus mellitus 5. square (width=height) wrists (as opposed to rectangular) Smoking is not strongly associated Males tend to have worse disease Diabetus mellitus is a significant risk factor for bilateral lesions. American Society for Surgery of the Hand has issued a statement that the current literature does not support a causal relationship between specific work activities and the development of diseases such as CTS. Aetiology Approximately one-third of patients with carpal tunnel symptoms have associated medical conditions such as inflammatory arthritis, diabetes, pregnancy, amyloidosis, hypothyroidism and acromegaly (NEJM 1993) Local and Systemic factors o Systemic factors act to directly or indirectly affect microcirculation, pressure thresholds for nerve conduction, nerve cell body synthesis, and axon transport or interstitial fluid pressures. Acute vs Chronic Trauma-related structural changes 1. Distal radius fracture 2. Lunate dislocation 3. Posttraumatic arthritis/osteophytes 4. Edema 5. Hemorrhage 6. Burns Systemic diseases 1. Rheumatoid arthritis 2. Diabetes mellitus a. Reduces threshold for developing symptoms 3. Thyroid imbalance (especially hypothyroidism) a. Consider this if recurrent presentation after surgery b. Causal relationship not clear 4. Amyloidosis 5. scleroderma 6. Hemophilia 7. Alcoholism 8. Raynaud's phenomenon 9. Paget's disease 10. Gout 11. Chronic renal failure/hemodialysis 12. Glycogen storage diseases in children Anomalous anatomic structures 1. Aberrant muscles (eg, reversed palmaris, palmaris profundus) 2. Unusually extensive lumbricals or FDS/FDP bellies 3. Median artery thrombosis 4. Enlarged persistent median artery Hormonal changes 1. Pregnancy a. up to 17% of pregnant women, mostly in third trimester b. weight gain increases risk c. most resolve spontaneously after delivery d. 11% of women reported CTS six months after delivery and 4.3% still had the condition a year afterward 2. Menstrual disorders 3. Menopause 4. Oral contraceptive pill 5. Acromegaly Infections 1. TB Tumors/neoplasms 1. Lipoma 2. Ganglion 3. Fibroma 4. Aneurysm of median artery Mechanical overuse 1. Vibrating machinery Differential Diagnosis 1. 2. 3. 4. 5. 6. Cervical radiculopathy (double crush syndrome) Thoracic outlet syndrome Pronator teres syndrome De Quervain’s syndrome RSD Tenosynovitis Pathophysiology Compression leads to 1. swelling of tenosynovium 2. thickening of transverse carpal ligament 3. focal demyelination of median nerve. 4. Axonal loss in more severe cases initial insult is a reduction in epineural blood flow and venous congestion, which occurs with 20 to 30 mm Hg compression. Intracarpal canal pressures in patients with CTS routinely measure at least 33 mm Hg and often up to 110 mm Hg with wrist extension. Continued or increased pressure eventually causes edema in the epineurium and endoneurium. If applied for 2 hours, pressure of 50 mm Hg will cause epineural edema, and if applied for 8 hours, it will increase endoneural fluid pressure fourfold and block axonal transport. As further injury occurs to the capillary endothelium, more protein leaks out into the tissues, which become more edematous, and a vicious cycle ensues. The effects are most pronounced within the endoneurium, since more exudate and edema accumulate there, unable to diffuse across the perineurium. The perineurium resists pressure changes because of its higher tensile strength and acts as a diffusion barrier creating in effect a "compartment syndrome" within the nerve. Histopathology Path of flexor tenosynovium shows inflammation in only 10%, but oedema and vascular sclerosis in 98% Diagnosis History most common symptom is paresthesias in the distribution of the median nerve – middle and index most common Other symptoms include feelings of clumsiness and weakness in the affected hand, often made worse with activity. Proximal radiation of pain or paresthesias to the elbow or even the shoulder is not uncommon Night pain is a consistent symptom. Theories: o Phalen postulated that when the hand and wrist are at rest during sleep, engorgement and relative venostasis occur in the small vessels within the flexor synovialis, producing swelling, more nerve compression within the tunnel, and worse pain. Active motion of the fingers and wrist decreases venous engorgement and relieves pain, a phenomenon consistent with many patients' histories and their need to shake or exercise their hands to relieve night pain. It is an interesting theory that emphasizes the vascular etiology of the disorder, but there is no published evidence to prove the hypothesis. o Patients hold their wrists flexed while sleeping, thus increasing the pressure on the median nerve and causing pain. Therefore, preventing wrist flexion would be expected to decrease symptoms, and may be why many patients find it beneficial to wear neutral-position wrist splints at night. Examination thorough physical examination of the neck and upper extremity should be performed Sensory findings (threshold tests best): 1. Semmes-Weinstein pressure monofilaments: Values greater than 2.83 may be indicative of CTS. 2. Vibratory sensibility: A vibrating 256-cycle per second tuning fork is placed against the patient's fingertips. The median and ulnar fingers of both hands are tested. The test is considered positive if decreased sensation is perceived. 3. Static and moving 2-point discrimination: Failure to discriminate more than 6 mm (static) or 5 mm (moving) is a positive finding – this is a late finding as can remain normal until nearly all sensory conduction has ceased. Thenar atrophy is a sign of advanced CTS of long-standing duration. Provocation tests 1. Tinel’s a. Sensitivity - 25 to 79% b. Specificity – 60-95% c. One study showed Tinels to be the most specific (84 percent), but the least sensitive (32 percent) of all the provocation tests 2. Phalens (wrist flexion) a. patient's elbows are placed on a table, the forearms are perpendicular to the table, and the wrists are flexed for 60 seconds. The test is positive if numbness or paresthesias develop in radialsided digits b. Sensitivity - 42 to 85% c. Specificity – 54-98% 3. reverse Phalen's (wrist extension) 4. carpal compression 5. vibration testing 6. Durkan’s pressure test a. Applies a known standard pressure (150mmHg) over the TCL b. 10% false positive rate No one test is diagnostic Investigations Investigations for systemic diseases – hypothyroidism, diabetes Nerve conduction studies most appropriate role for electrodiagnostic testing is as an adjunct to the clinical assessment in instances where the diagnosis is not clear Distal motor latencies of 4.5 millisecs and sensory latencies of 3.5millisecs abnormal Difference between hands of 1 ms (motor) or 0.5 ms (sensory) abnormal Electromyography of thenar helpful for signs of denervation There is no relationship between the nature or duration of pre-operative symptoms and the severity of the electrophysiological impairment. There is no relationship between pre-operative nerve conduction impairment and either successful outcome of surgery (defined as complete symptom relief) or time to resolution of symptoms after surgery Imaging studies Xray wrist – arthropathy, post trauma deformities US and MRI not routinely performed unless masses suspected MRI may be useful to assess recurrent symptoms post repair o following adequate carpal tunnel release, MRI may demonstrate an increase in carpal tunnel volume of up to 24%, often accompanied by a change in shape from oval to circular, resulting in increased anteroposterior and mediolateral diameters. o incomplete surgical release of the flexor retinaculum can occur and be detected by a residual increase in T2 signal of the median nerve within the carpal tunnel and by direct visualization of the still-connected fibers of the retinaculum. o Other changes include excessive fat within the carpal tunnel, neuromas, scarring, and persistent neuritis. Management Nonoperative 1. splinting in neutral o initial trial of full-time splinting for 3 to 4 weeks followed by part-time night splinting is recommended. 2. NSAIDs 3. diuretics to reduce oedema o little evidence to support effectiveness 4. treat underlying disease o often resolves symptoms in hypothyroidism 5. Vit B6 was thought to be good but doesn’t modify disease 6. Steroids – 80% relief (transient), 22% symptom free at 1 year o Most likely to benefit are those with symptoms <1yr; diffuse and intermittent numbness; normal 2 point discrimination; no weakness or atrophy; <1-2ms prolongation in latency for M and S o 40% of this group symptom free for >12 months o Injection method 22 or 25g needle 1cm prox to distal wrist crease ulnar to PL at angle of 45 degrees (distal and dorsal) Recent BJPS article suggest safer to go radial to FCR advance until hit floor then withdraw 0.5cm 1ml of betamethasone (Celestone 5.7mg/ml water soluble) or triamcinolone (Kenacort A10 10mg/ml) + 2ml of Xylocaine 1% withdraw if median n paraesthesias splint wrist continuously for 3 weeks o good response to injection is correlated with an excellent response to subsequent surgery. Conservative management unlikely to work if 1. Older than 50 years. 2. Symptoms lasting 10 months or longer. 3. Continual numbness. 4. The thenar muscles have begun to atrophy 5. Symptoms occur within 30 seconds during a Phalen's test. If none of above present, conservative management will work in 2/3rd of cases 40% if one present and 20% if 2 present and nearly none if >2 present Operative Indications 1. Failure of conservative management 2. acute CTS 3. severe chronic CTS – thenar atrophy, reduced 2 point discrimination 4. secondary to mass compression Open technique tournique, local or regional block Taleisnik advocates incision placement ulnar to axis of flexed ring finger at level of wrist crease (avoids PCN) 1. Or stay ulnar to PL at distal wrist crease 2. Or 5mm ulnar to interthenar depression and extend distally in line with 3rd web space (MacKinnon) – PCN lies 5mm radial to this 3. Avoid too ulnar placement – risk palmar cutaneous branch of ulnar nerve, nerve of Henle (nerve of ulnar artery) and entry into Guyon’s canal Kaplan’s cardinal line – apex of thumb-index web toward hook of hamate, parallel to prox palmar crease 1. Intersection of line with middle finger flexed into palm = recurrent br 2. Deep palmar arch lies deep to cardinal line 3. Superficial palmar arch between cardinal line and prox palmar crease Curvilinear incision beginning prox to Kaplans line, 2-3mm ulnar to thenar crease (remain ulnar to PL or flexed ring finger at distal wrist crease) Blunt dissection transversely => visualise TCL Antebrachial fascia penetrated with fine artery – median n identified Blunt dissection to separate median nerve and TCL Sharp division of TCL on ulnar border Distal median n and recurrent branch visualised Residual fibres divided Antebrachial fascia release in prox part of wound Tourniquet down – haemostasis Skin closure Outcomes 96% patient satisfaction with 84% return to work grip strength return to pre-op at 3months and pinch strength at 6 weeks TCL repair Theory 1. to prevent bowstringing: MRI evidence of an increased volume of the carpal canal and volar migration of the median nerve and flexor tendons after release 2. to improve excursion of flexor tendons: D Netscher PRS 1997 Postoperative grip and pinch strength values for the transposition flap repair group surpassed those of the other two groups at 12 weeks 3. reduce pillar pain, tranverse arch widening Best indicated for RA, during concomitant tendon repairs, and CTS release in conjunction with trigger release/Dupuytren’s has been associated with reformation of the carpal tunnel and the subsequent recurrence of symptoms. no benefit demonstrated from neurolysis or epineurotomy Release of Guyons not recommended as Guyons canal opens up with release of TCL on MRI synovectomy not indicated as increases post op haematoma formation + produce adhesions but indicated for proliferative or invasive tenosynovitis – eg. in gout, inflammatory arthritis or infection (TB) Bowers Limited incision Endoscopic 30 degree scope used 1. Chow 2 portal technique o Entry portal – line 1-1.5cm radial to pisiform prox pole + line 0.5cm prox to end of first line o 1cm transverse cut from end of 2nd line – thru fascia o curved dissector/obturator passed to touch hook of hamate o exit portal – fingers hyperextended, 0.5cm long cut made 1cm prox along line that bisects angle drawn between distal border of fully abducted thumb and third web space o probe knife inserted – cutting distal TCL (distal to prox) o triangle knife cuts midsection o retrograde knife pushed from prox to distal to join cuts o then endoscope inserted distally and process repeated but prox to distal 2. Seiler’s modification of Chow 2 portal technique o Prox port made just ulnar to PL and distally based fascial flap created to improve visualisation o Distal port made before trocar insertion to identify palmar arch o Trocar inserted along axis of ring finger o Limited wrist extension (30 deg) 3. Agee single portal endoscopic technique (Agee 3M system) o 2-3cm transverse cut between FCR and FCU in wrist crease that separates glabrous palmar skin and wrist skin o spreading technique until fascia identified o U shaped distally based forearm fascial flap raised o probe passed along line of base of 4th finger radial to hook of hamate o blade assembly inserted with viewing window up against deep surface of TCL o palpate and visualise distal border – blade extended and camera withdrawn – cuts distal 2/3rds o blade assembly re-inserted and TCL inspected and more cuts to release remaining fascia Post op – splinting for 2 weeks may be detrimental – increase in wound pain in first month post op o Not routine but if splint, use for only one week o Home physio programme of separate finger and wrist exercises Open vs Endoscopic Early studies showed endoscopy had no special benefit in terms of outcome, and with a substantially increased risk. It was associated with 1. a substantial risk of significant complications including injuries to the median and ulnar nerves, lacerations of the flexor tendons 2. incomplete release of the carpal tunnel. o More likely to miss other compressive pathologies – ie synovitis (risk of recurrence highest in those with bilateral CTS) These complications were especially likely to occur where the procedure was only carried out occasionally. Schmelzer PRS Jan 2006 – 753 hands treated with endoscope. 100% symptom improvement. Complications included one transient median nerve neurapraxia, six complaints of residual pain, and one complaint of hypersensitivity. 3 prospective, randomized clinical trials comparing the endoscopic and open methods 1. Agee (J Hand Surg Am. 1992) a. higher complications noted with endoscopic 2. Brown et al.( J Bone Joint Surg Am. 1993) a. independent randomized trial of the two-portal technique, with an 84 day follow-up b. Authors expressed concern that the endoscopic technique may have a higher rate of complication 3. Trumble ( J Bone Joint Surg Am. 2002) a. independent randomized trial of the 1-port technique of 192 hands in 147 patients, with a 1 year follow-up b. During the first three months after surgery, the patients treated with the endoscopic method had better Carpal Tunnel Syndrome Symptom Severity Scores, better Carpal Tunnel Syndrome Functional Status Scores, and better subjective satisfaction scores. c. During the first three months after surgery, they also had significantly (p < 0.05) greater grip strength, pinch strength, and hand dexterity. After that, both returned to preoperative levels d. The open technique resulted in greater scar tenderness during the first three months after surgery as well as a longer time until the patients could return to work (median, 38 days compared with 18 days after the endoscopic release). e. No technical problems with respect to nerve, tendon, or artery injuries were noted in either group. f. There was no significant difference in the rate of complications or the cost of surgery between the two group Metanalysis (PRS 2004) a. endoscopic carpal tunnel release is favored over the open carpal tunnel release in terms of a reduction in scar tenderness and increase in grip and pinch strength at a 12-week follow-up. b. With regard to symptom relief and return to work, the data are inconclusive. c. Irreversible nerve damage is uncommon in either technique; however, there is an increased susceptibility to reversible nerve injury that is three times as likely to occur with endoscopic carpal tunnel release than with open carpal tunnel release. Complications 3-19% Postoperative complications may be classified into the general areas of neurological, vascular, tendon, and wrist complaints. Early 1. Hematoma a. May cause skin necrosis requiring flap coverage b. Long term increase risk of scarring 2. Nerve damage a. PCN most common 3. 4. 5. 6. b. Recurrent branch c. Main trunk d. Ulnar nerve tendon damage superficial arch damage a. pseudoaneurysm Stiffness Infection Late 1. Recurrent symptoms a. Incomplete division of TCL b. Extensive scarring – adhesive neuritis c. Untreated systemic conditions 2. Pillar pain (pain in thenar and or hypothenar area) 3. carpal arch widening a. direct relationship exists between widening of the transverse carpal arch and loss of grip strength. b. Residual pain, forearm circumference, and wrist range of motion are not related to widening of the transverse carpal arch. 4. Pisotriquetral pain syndrome (J Hand Surg 1989) a. Hypothenar pain – reported in 1.1% b. Pain, discomfort, and loss of grip strength mostly during activities requiring full hand grip or activities associated with use of the heel of the hand, such as pushing up from a chair, or pushing open a door with the flat palm. c. pain from the piso-triquetral joint, possibly a result of intercarpal alignment change after carpal tunnel release. d. Pisiform excision curative, with complete relief of symptoms and return of strength and dexterity. 5. Scar pain 6. Scar 7. Persistent weakness 8. Tendon adhesions, triggering and bowstringing a. higher frequency of trigger finger noted after carpal tunnel surgery. b. A possible explanation is that the transverse carpal ligament may also normally function as the first tendon pulley. c. When this is released, greater forces are then transmitted to the first annular ligament, which is now the most proximal pulley and may contribute to triggering at this site. 9. complex regional pain syndrome Secondary Surgery From PRS CME 2001 (Mackinnon) Aetiology Persistent Symptoms - 7- 20% have persistent symptoms following carpal tunnel release. 1. Most often, the transverse carpal ligament (flexor retinaculum) is incompletely released, with the problem usually in the most distal portion of the ligament may also occur more proximally by inadequate release of the most distal portion of the antebrachial fascia 2. compression of the median nerve further proximally in the forearm or the neck. There is a well-established association between carpal tunnel syndrome and cervical disc disease 3. incorrect diagnosis of CTS Recurrent symptoms 1. Postoperative scarring (common findings at revision surgery) a. may involve the median nerve directly by forming around it and entrapping the nerve (adhesive median neuritis, epineural fibrous fixation, or neurodesis) b. results in diminished longitudinal excursion of the median nerve, which has been shown to be approximately 1.0 cm in normal wrists c. Contributory factors may include hematoma formation, prolonged postoperative immobilization, or inadequate range-of-motion exercises and therapy d. Excess scar tissue may also indirectly affect the nerve by leading to reformation of the transverse carpal ligament 2. Unmask a more proximal site of compression New Symptoms - Neurologic injury 1. PCN most commonly a. incision too radial. b. abnormal sensation in the territory of the nerve and a Tinel sign at the level of the injury. 2. 3. 4. 5. c. Primary entrapment neuropathy of the palmar cutaneous branch has been reported - Transection of the transverse carpal ligament may not release pressure on the palmar cutaneous branch because it may have its own distinct tunnel to the hand, and postoperative swelling and edema may lead to compression of this tunnel d. tender hypertrophic scar is likely to be the result of injury to small cutaneous branches Recurrent branch a. Weakness/atrophy of APB Median nerve a. portion of the median nerve to the third webspace is frequently injured - most superficial or anteriorly located fascicles of the median nerve b. bowstringing or anterior dislocation of the median nerve rare Ulnar nerve a. palmar cutaneous branch, and/or a communicating branch between the median and ulnar nerves Complex regional pain syndrome type I a. rare, but it may follow carpal tunnel surgery or, alternatively, may be caused or exacerbated by carpal tunnel syndrome. Multiple factors have been associated with poor results, including a. injury to the median nerve either from chronic compression or iatrogenic surgical injury, b. excessive scar formation preventing the nerve from gliding with wrist motion c. subcutaneous atrophy of the palm d. secondary gain factors (workers compensation) Clinical thorough clinical evaluation, including a complete neurological examination of the hand and upper extremity, provides an accurate assessment of the status of the median nerve distally and proximally Determine if persistent,recurrent or new symptoms Management results following reoperation have been significantly worse, with up to 95 percent residual symptoms and 40 percent poor results Secondary external or internal neurolysis internal neurolysis - the external and internal epineurium is opened until a normal fascicular appearance with visible perineurial markings (bands of Fontana) is seen. Opening the perineurium is avoided because it is an anatomical site of the blood-nerve barrier. Release of entrapment of recurrent branch Neuroma-in-continuity assessment, neuroma management, nerve grafting PCN neuroma is neurolysed proximally and buried into muscle injury to the main portion of the median nerve itself will usually require an interposition nerve graft o thorough preoperative evaluation is vital to provide a good understanding of the components of the nerve that are uninjured, those that are only partially injured, and those that are not functioning at all. o Managed as a Sutherland sixth-degree injury, dissecting and replacing only the affected portion of the nerve o Donor nerves 1. first choice - the anterior branch of the medial antebrachial cutaneous nerve. The landmark for finding the medial antebrachial cutaneous nerve is the adjacent basilic vein located along the medial border of the biceps muscle. The anterior branch supplies sensation to the ulnar volar aspect of the forearm 2. if only short nerve graft needed, the lateral antebrachial cutaneous nerve may be used instead. It lies adjacent to the cephalic vein along the medial border of the brachioradialis muscle in the proximal forearm, and the donor scar is therefore more visible. 3. terminal branch of the anterior interosseous nerve just proximal to the pronator quadratus muscle. Because it is an expendable motor nerve, there is no sensory loss. 4. use of the sural nerve for grafting should be reserved for cases in which long grafts or multiple cable grafting will be needed The pattern of nerve injury may vary along the length of the nerve and from fascicle to fascicle at a given level. This illustration of a cross-section of a nerve reveals a sixth-degree or mixed injury pattern. The fascicle at the 12 o'clock position is normal. Moving in a clockwise direction, the fascicle at 1 o'clock demonstrates a first-degree injury (I), or neurapraxia with segmental demyelination. At the 3 o'clock position, a second-degree injury (II), or axonotmesis, is shown. Injury to the axon, myelin, and endoneurium, or third-degree injury (III), is demonstrated by the two smaller fascicles, which are more centrally located. A fourth-degree injury (IV), as shown by the fascicle at the 9 o'clock position, has marked fibrosis across the nerve, with only the epineurium remaining intact. At the 5 o'clock position is a fifth-degree injury (V), which involves transection of the nerve and complete loss of continuity. The surgeon's role is to identify and reconstruct those fascicles with fourth- and fifth-degree injury patterns. Those with a first-, second-, or third-degree injury or a normal pattern should, at most, be neurolysed. Tissue interposition flaps aims to decrease scar adherence of the reoperated median nerve to enhance the development of new blood vessels, provide padding, and possibly serve as a bed for nerve regrowth. Options a. local pedicle muscle flaps pronator quadratus – difficult dissection but provides better coverage more proximally in the distal forearm abductor digiti minimi (favored by Mackinnon) 1st and 2nd lumbricals palmaris brevis - thin and somewhat variable in its size and thickness b. fascial flaps reverse radial artery fascial flap – provides little padding free thoracodorsal fascial flap c. fat flaps hypothenar fat pad flap (Strickland, J Hand Surg 1996) - limited in the proximal and distal extent of their coverage, are unable to cover the median nerve proximal to the wrist flexion crease, and cannot be placed circumferentially. d. autologous vein wrapping does not provide additional padding to the median nerve, nor does it enhance vascularity to the area. e. Regional flaps Radial forearm fasciocutaneous/fascial flaps f. Omental flap (PRS 2005) Omentum contains fibroblast growth factor, which has been shown to stimulate axon growth and nerve regeneration. Its major use in peripheral nerve surgery is for the treatment of post radiotherapy brachial plexitis. Fibroblast growth factor has also been shown to have significant angiogenic potential through its chemotactic and mitogenic activity in endothelial cells. Omentum has also been shown to be advantageous for preventing perineural fibrosis. Brunelli et al. compared omentum to muscle regarding its ability to prevent perineural fibrosis and found a five-fold increase in cicatrix following neurolysis associated with muscle coverage compared with omentum