Constriction Ring Syndrome
advertisement
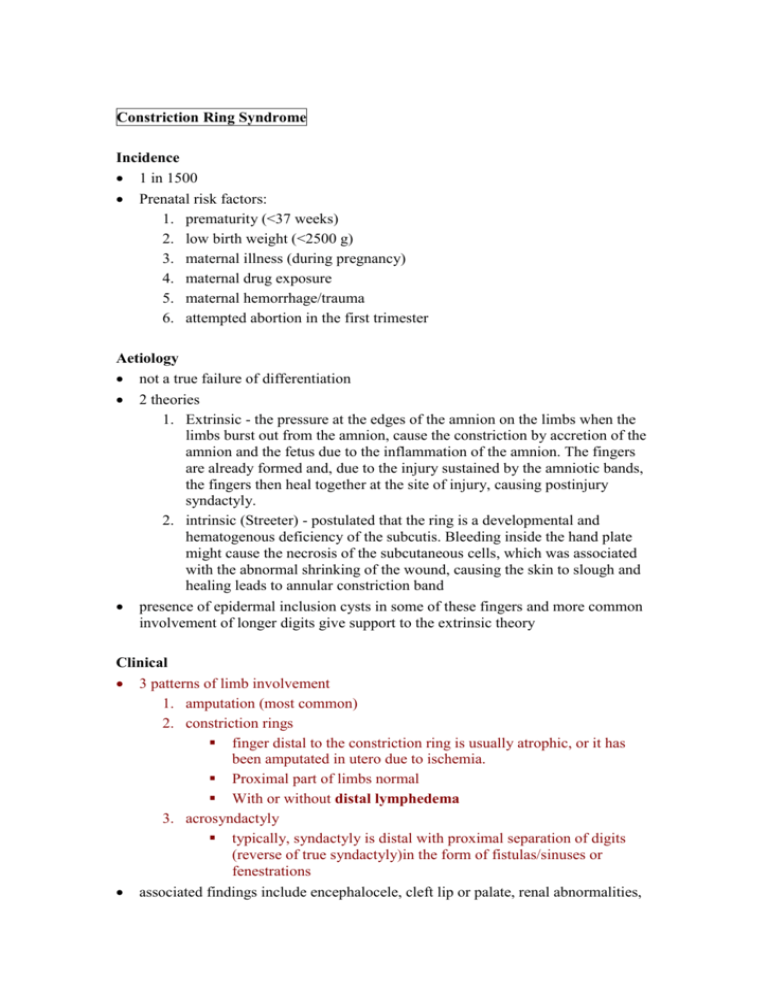
Constriction Ring Syndrome Incidence 1 in 1500 Prenatal risk factors: 1. prematurity (<37 weeks) 2. low birth weight (<2500 g) 3. maternal illness (during pregnancy) 4. maternal drug exposure 5. maternal hemorrhage/trauma 6. attempted abortion in the first trimester Aetiology not a true failure of differentiation 2 theories 1. Extrinsic - the pressure at the edges of the amnion on the limbs when the limbs burst out from the amnion, cause the constriction by accretion of the amnion and the fetus due to the inflammation of the amnion. The fingers are already formed and, due to the injury sustained by the amniotic bands, the fingers then heal together at the site of injury, causing postinjury syndactyly. 2. intrinsic (Streeter) - postulated that the ring is a developmental and hematogenous deficiency of the subcutis. Bleeding inside the hand plate might cause the necrosis of the subcutaneous cells, which was associated with the abnormal shrinking of the wound, causing the skin to slough and healing leads to annular constriction band presence of epidermal inclusion cysts in some of these fingers and more common involvement of longer digits give support to the extrinsic theory Clinical 3 patterns of limb involvement 1. amputation (most common) 2. constriction rings finger distal to the constriction ring is usually atrophic, or it has been amputated in utero due to ischemia. Proximal part of limbs normal With or without distal lymphedema 3. acrosyndactyly typically, syndactyly is distal with proximal separation of digits (reverse of true syndactyly)in the form of fistulas/sinuses or fenestrations associated findings include encephalocele, cleft lip or palate, renal abnormalities, cardiac defects, hemihypertrophy, anterolateral bowing of the tibia, tibial pseudarthrosis, and leg-length discrepancy. Hands affected in 90% of cases Clubfoot seen in 25% - 2 causes 1. transient oligohydramnios with sac rupture 2. constricting band around peroneal nerve (50%) Management Early management required for deep constriction bands 1. distal ischaemia 2. rapid increase in oedema 3. neurologic involvement Later management: 1. Constriction ring band excision - best to do ½ of the circumference at a time Z plasty – taking deeper perifascial fat layer in one limb and more superficial fat on the other limb V-Y plasty or W-plasty for tighter bands Upton describes advancing subcutaneous fat and fascial flaps to prevent recurrent contour deformities 2. Acrosyndactyly release similar to true syndactyly more skin graft generally required epithelialised tracks must be excised 3. Amputation type web deepening on-top plasties – transposing one digit on top of another skeletal lengthening (distraction) free toe transfers (all proximal structures normal)