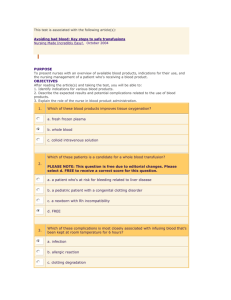
transfusion services (blood bank)
advertisement

TRANSFUSION SERVICES (BLOOD BANK) Introduction The Christiana Care Health Services maintains a Blood Bank and Transfusion Service. This section on Transfusion Therapy is designed to inform the Christiana Care Health Services staff of services provided by the Blood Bank Department and provide guidelines for transfusion. The "Circular of Information for the Use of Human Blood & Blood Components" and "Blood Transfusion Therapy -A Physician's Handbook" are available in the Blood Bank and should also be consulted for additional information. Indications for Transfusion Therapy Transfusion therapy with red blood cells (RBCs) is indicated for restoration of oxygen carrying capacity and correction of anemia. Most patients are not significantly symptomatic until the hemoglobin level is less than 7-8 grams/dl, however factors such as cause for the anemia and comorbid illnesses are considered in each transfusion decision. Platelets are indicated for correction of significant thrombocytopenia with bleeding, for prophylaxis in profound thrombocytopenia (usually less than 10,000), or for patients with thrombopathies. FFP and cryoprecipitate may be indicated for correction of coagulation defects in certain circumstances. All transfusion decisions involve integration of the clinical information and laboratory data and reflect both the benefit and risks of the therapy. Definitions and Explanation of Terms Blood Bank - A laboratory which is responsible for the collection, processing, manufacture, and storage of human blood and its components. Transfusion Service - A laboratory which is responsible for testing patient samples, storage of blood products, and issuing products for transfusion. Transfusion Therapy - The infusion of blood or one of its components for therapeutic purposes. Order - Formal written instructions from a physician which appear on a patient chart or on a prescription form requesting services and/or products. Request - The act of asking to supply products or services as a result of the physician's order. Transfusionist - A physician or registered nurse specially trained in transfusion practices who performs the phlebotomy and/or starts to transfuse the blood or blood component. Only the transfusionist may break the seal of the unit. Transfusion Reaction - Any untoward effect resulting from a transfusion. All suspected reactions must be reported to the patient's physician and the Transfusion Service Lab (Blood Bank) and/or IV nurses at the time it is noted. Unit Label - The non-removable label on the front of the blood or blood component containing information regarding the contents of that unit. Requisitions All Transfusion Service Laboratory (TSL) tests can be ordered by using a manual Transfusion Service Laboratory Requisition (the red and white form #18821 S) or by the Clinical Care System (CCS). All manual requisitions must be stamped with an addressograph plate or the information normally found on the plate must be legibly handwritten. The physician's order must be transcribed in the space provided on the requisition for requesting blood and blood components. Both types of requisitions (manual and CCS) have a space for the signature of the phlebotomist. Each specimen sent to the Blood Bank must be accompanied by one of the requisitions. The only exception to this would be immunology tests ordered through the CCS. No testing will be performed unless the specimen and a properly signed slip have been received and all patient identification information match. Services Provided by the Transfusion Service Lab Diagnostic Hepatitis Markers - tests for infectivity and/or evidence of prior exposure to the viruses (viral antibodies) HBsAg and confirmation - used to detect the presence of the Hepatitis B surface protein in the serum. Anti-HBc - detects the antibody to the Hepatitis B core antigen which is present in nearly all chronic HBsAg carriers. Anti-HBs - detects the antibody to HBsAg and usually indicates immunity to Hepatitis B virus. Anti-HCV - detects the antibody to the Hepatitis C virus previously called non-A, non-B hepatitis. Anti-HAV(IgM) - used to detect the IgM class antibody to Hepatitis A that appears during the acute phase of infection and persists through early convalescence. Anti-HBc(IgM) - used to detect the IgM class antibody to the Hepatitis B core antigen. It is a reliable marker for acute disease and can be valuable for diagnosing post-transfusion Hepatitis B. Immunologic Tests Anti-HIV I/II - detects antibodies to human immunodeficiency viruses type 1 and/or type 2 which cause Acquired Immunodeficiency Syndrome (AIDS). Rapid HIV – detects antibody to HIV 1 only. Limited to needlestick/exposures through Employee Health and untested mothers in L&D. Anti-HTLV-I/II - detects antibodies to the human T-lymphotropic virus type I/II which has been associated with Adult T-cell leukemia. CMV - semi-quantitative measurement of IgG antibodies to cytomegalovirus in serum to indicate past or current infection. Rubella - quantitative measurement of IgG antibodies to the Rubella Virus in serum to aid in the determination of immune status. Toxoplasma - quantitative measurement of IgG antibodies to Toxoplasma gondii in serum to aid in the determination of immune status. Send Out Tests - tests sent to facilities outside the hospital. HAV - antibody to Hepatitis A virus. This combination test detects IgM and IgG antibodies. HDV - antibody to Hepatitis Delta virus. HBeAg - detects Hepatitis B envelope antigen. Anti-HBe - antibody to HBeAg HCV PCR - Hepatitis C by polymerase chain reaction method, qualitative test. HCV RIBA - Hepatitis C by radio-immunoblot assay HCV RNA - Hepatitis C ribonucleic acid, quantitative test. HIV I and HIV II Western Blots - confirmatory test for HIV I and HIV II that detects viral gene proteins. HTLV I/II Western Blot - confirmatory test for HTLV I/II Rubella IgM - measurement of IgM antibody CMV IgM - measurement of IgM antibody Toxo IgM - measurement of IgM antibody Antibody Titer Titration is a semi-quantitative measurement of the amount of antibody contained in a serum; the higher the titer, the more antibody present. The serum is diluted serially until the antibody can no longer be detected and the titer is reported as the reciprocal of the highest reactive dilution. Both autoantibodies and allo-antibodies may be titered. Cold (auto) agglutinin titer may be elevated in the serum of patients with certain diseases; for example, an elevated titer (greater than 32) in a patient with respiratory symptoms may be indicative of mycoplasma infection. Serial titers of autoantibodies may be employed to assess response to therapy. Allo-antibodies such as the naturally occurring isoagglutinins anti-A and anti-B are sometimes titered in assessing immune competence. Cold antibodies are usually complete (IgM) antibodies with a blood specificity of Anti-I. Titers less than or equal to 32 are of no significance. In patients with acquired hemolytic anemia associated with a cold antibody, the titer is usually in the thousands. Elevated cold agglutinin titers are also seen in primary atypical pneumonia. The most frequent use of the antibody titer is to follow serially the response of each alloantibody to a red blood cell antigen found in the mother's serum during pregnancy. If the antibody is of IgG structure and directed against a red cell antigen inherited by the baby from its father, the possibility for Hemolytic Disease of the Newborn (HDN) exists. Rh HDN is the most common. Antigen-positive red cells from the baby will usually stimulate the mother to produce more antibody, producing a rising titer. Special Collection for Cold Agglutinin Blood should be collected in a prewarmed (37o C) purple top vacutainer tube immediately placed in a cup of warm (37o C) water and taken directly to the Blood Bank. Direct Antiglobulin Test (DAT) The DAT is used to detect globulins immunologically bound to the patient's red cells in vivo. The test is used in the diagnosis of hemolytic disease of the newborn, autoimmune hemolytic anemia, investigation of transfusion reactions, and diagnosis of drug-induced red cell sensitization reactions. A cell eluate may be performed when the DAT is positive in order to determine the identity of the antibody coating the cell. An eluate is the solution recovered after attempting to remove antibodies from red blood cells. Several techniques are available and the technique used will depend on the circumstances in each case. After an eluate is prepared, it is tested in the same manner as serum to detect antibodies. Occasionally a cell eluate may demonstrate the presence of an antibody coating the cell which cannot be detected by performing a routine antibody screen. The test is also used in investigation of transfusion reactions if the DAT becomes positive after the patient has been transfused. Antigen Profile The profile consists of typing the patient's cells for common antigens in the ABO, Rh, Kell, Kidd, Duffy, MNS, Lewis and P blood group systems for which antisera are available. Patients whose cells lack antigen in any of these systems have the potential to produce antibodies against those antigens if the patient receives blood possessing those antigens. When the DAT is positive, the extent of typing in the profile is reduced. An antigen profile is suggested for anyone expected to receive serial transfusions over a long period of time such as patients with renal disease, malignancies, chronic anemia, or other blood dyscrasia. Transfusion Reaction Evaluation Any symptoms suggestive of a transfusion reaction during or after a transfusion must be reported to the physician and the Transfusion Service Lab for investigation. Post transfusion samples must be drawn immediately. The investigation is a stat work-up consisting of 1) a clerical check for errors, 2) inspection of plasma for hemolysis, 3) a DAT, and 4) visual inspection of a post transfusion urine specimen. Any indication of a hemolytic reaction will result in additional tests being performed. Please refer to Adverse Reactions to Transfusions. Platelet Antibody Studies The Blood Bank sends testing for post-transfusion purpura (PTP) and Neonatal Alloimmune Thrombocytopenia (NAIT) to the Red Cross. The majority of PTP cases are associated with anti- PLA1 antibodies, although other specificities do occur. Antibodies are detected during the acute phase of thrombocytopenia, and platelet antigen typing is completed when the patient's platelet count recovers. NAIT is caused by passive transfer of maternal antibody to the newborn. The mother's serum is tested against the platelets of the father and a panel of known, typed platelets. Specificity is often found to be anti-PLA1, but specificities with Bak, Yuk, Br, and HLA are reported. HLA ABC and DR typing and HLA Cytotoxic Antibody Testing HLA ABC and DR typing is usually performed on potential bone marrow transplant candidates. HLA ABC and HLA cytotoxic antibody testing is usually performed on patients about to undergo chemotherapy for possible HLA matched platelet pheresis support in the event the patient becomes refractory to platelet transfusions. Testing requires a calculation of the number of tubes to be drawn based on the patient white count. Advance scheduling is also required. It is therefore necessary to contact the blood bank prior to ordering testing. Pretransfusion Neonatal Typing Tests performed include ABO, Rh, and DAT. Neonatal Typing should be ordered when sending cord bloods or other specimens for testing of neonates or infants less than four months of age. Type and Screen This is not an order to perform compatibility testing, but to perform all testing required (ABO, Rh, and antibody screen) prior to compatibility testing. Compatibility tests will only be performed when there is a physician's order for transfusion. Type and Crossmatch This test includes ABO, Rh, antibody screen, and crossmatch of blood for transfusion. The physician's order to transfuse or crossmatch blood for the patient must be written as it appears on the chart. Rh Immune Globulin (RhIg) Evaluation Antepartum, amniocentesis, or termination of pregnancy - This work-up is performed to evaluate the need for giving Rh Immune Globulin (RhIg) and consists of an ABO and Rh and antibody screen. All pregnant Rh negative women should be evaluated as candidates to receive RhIg. Postpartum - After delivery, the newborn's blood type will be determined. If the baby is Rh negative, the mother does not need a RhIg Evaluation. If the baby's type is Rh positive or cannot be determined, the mother is a RhIg candidate and a postpartum sample must be collected. This sample will determine if the mother should receive more than one dose of RhIg. Therapeutic Products See "Circular of Information for the Use of Human Blood and Blood Components" (prepared by AABB and ARC) or specific product circulars for commercially prepared products. The last ten products in this section (12-21) are commercially prepared. Red Blood Cells (Leukopoor) The red cells from a unit of whole blood that have been filtered to remove >99% of leukocytes. Leukocyte-poor RBC's are used routinely for all RBC transfusions. Storage may be up to 42 days at 4oC depending on the coagulant used when drawing the unit. Red Blood Cells (Washed) The red cells from a unit of whole blood that have been washed and resuspended in normal saline. Washed cells contain little or no serum proteins. After a unit has been washed, it can be stored for only 24 hours at 4 oC. This product may only be ordered after consultation with the Blood Bank Medical Director. Red Blood Cells (Deglycerolized) The red cells from a unit of whole blood that have been glycerolized and stored frozen up to ten years. Prior to transfusion, the unit is thawed, deglycerolized, and washed. Deglycerolized cells contain reduced numbers of leukocytes and little or no serum proteins. After deglycerolization, the unit can be stored for only 24 hours at 4oC. This product may only be ordered after consultation with the Blood Bank Medical Director. Autologous Blood Autologous transfusion refers to the transfusion of blood or blood components to the same person who donated the blood. Patients wishing to donate autologous blood are referred to the Blood Bank of Delaware. (A physician order is required.) The donor center then delivers autologous units to the appropriate hospital. These units are kept in inventory until they expire. Each unit donated for autologous use shall have a special tag permanently attached to the unit. A tag with the heading, "Autologous Unit – For Autologous Use Only" indicates that the unit is not acceptable for allogeneic transfusion. Designated Donation Designated donations are units drawn for transfusion to a specific patient, usually from family members or friends of the patient. A tag with the heading, "Designated Donation" and the patient's name and date of birth will be attached to the bag. Designated donors are tested for infectious disease markers, therefore 72 hours is required before blood is available to allow for testing. A husband is not recommended as a directed donor for his wife of child bearing age. If the wife receives this blood, she may produce antibodies that may affect future babies and cause hemolytic disease of the newborn. Designated donors are not collected at Christiana Care. These donors are referred to the Blood Bank of Delaware. Platelets (Apheresis, HLA-matched, Random Donor Pools) Platelets for transfusion are obtained by donor platelet pheresis. Rarely, and only with the approval of the Blood Bank Medical Director, pools of six random donor platelets prepared from individual units of donated whole blood may be provided. For adults, ABO-compatible platelets are preferred, but are not essential. Platelets are not routinely crossmatched, however, crossmatching is required if the platelet product contains more than 5 ml of red cells. Platelets can be stored for up to five days after collection. Platelet pheresis products are now tested for bacterial contamination before being delivered from the Blood Bank of Delaware. Testing is initiated before the products are sent, but results may not be available before the platelets are transfused. Should a pheresis product test positive for bacteria, the blood center will notify our Blood Bank. Our Blood Bank will quarantine the product, as well as notify the physician if the product has been transfused. Platelet pheresis is an effective way to harvest a therapeutic adult dose of platelets from one individual donor. Platelet pheresis should contain 3x1011 platelets, and the plasma volume will vary between 200 and 500 ml. If approved by the Blood Bank Medical Director, six random donor platelet concentrates may be pooled for transfusion. Each individual platelet contains not less than 5.5x1010 platelets in 50-70 ml of plasma. The pool of six platelet concentrates should, therefore, contain no less than 3x1011 platelets suspended in 300-420 ml of plasma. Once the pool is prepared, this product expires in four (4) hours. The platelet concentrates in each pool are tested for bacterial contamination before being issued. If the plasma volume of the platelets is considered excessive the product may be centrifuged to permit removal of the undesirable plasma. Following this centrifugation, the platelets must rest for 1 hour without agitation, then be gently agitated for 1 hour to assure the resuspension necessary for optimum function and survival before they can be transfused. This two-hour delay must be considered by the physician when requesting reduced volume platelet transfusions. HLA matched platelet pheresis may be requested from the blood bank for patients who demonstrate refractoriness to platelet transfusion. The products are obtained by the blood bank from Penn Jersey American Red Cross and require scheduling of product and preliminary HLA A,B, and C typing, and tests for HLA cytotoxic antibodies. A one (1) hour post-transfusion platelet count is recommended after each platelet transfusion. This count should be used to determine the correct platelet increment for the patient, and helps determine how the patient responded to the platelet transfusion. When Rh positive platelets are transfused to Rh negative females of childbearing age (<50 y/o), Rh Immune Globulin prophylaxis is required to prevent Rh immunization which could occur due to the small amount of red cells in the product. Granulocytes This product is obtained by leukocytapheresis of a donor in which granulocytes are removed. The product contains not less than 1 x 1010 granulocytes in 50-100ml of plasma and hydroxyethyl starch (HES). The product can be stored for only 24 hours, however transfusion as soon as possible after collection is recommended. Pretransfusion compatibility testing is performed the same as for red cell transfusion. Reduction of plasma volume of this product is undesirable unless the patient clearly presents a problem of volume overload. Fresh Frozen Plasma The plasma removed from a unit of whole blood and frozen within six (6) hours from the time of collection. This product can be stored up to one year at -18oC from the date of collection. Once thawed, FFP can be stored for 24 hours at 1-6oC. This product is not intended for use as a plasma volume expander. Major indication for use is to supply plasma clotting factors. Cryoprecipitated AHF A blood component obtained from a unit of whole blood. This product is prepared by thawing Fresh Frozen Plasma at 4oC and separating the plasma cryoprecipitate from the thawed plasma. This product can be stored up to one year at -18oC from the date of collection. Once thawed, cryo can be stored up to 6 hours at room temperature unless pooled. A pooled cryo product can be stored for only 4 hours at room temperature. Individual bags are not assayed, however, each bag should contain more than 80 units of Factor VIII in a volume of approximately 30 ml. Each unit also contains approximately 150 mg or more of fibrinogen. NOTE: The next five products are not issued without approval of the Transfusion Service's Medical Director or his designate. Factor VIII (Dried) Pooled concentrate of human Factor VIII commercially freeze dried and stored in the Blood Bank. This product is used for patients with Hemophilia A. Both monoclonal and recombinant Factor VIII products are available. Factor IX (Dried) Pooled concentrate of human Factor IX commercially freeze dried and stored in the Blood Bank. This product is used for patients with Hemophilia B. Both monoclonal and recombinant Factor IX products are available. Factor IX Complex (Factors II, VII, IX, and X, Dried) This product is prepared from pooled human plasma and then freeze dried. Each vial is assayed and labeled for Factor IX. More information regarding this product should be obtained from the package insert. This product is used for patients with Hemophilia A with inhibitors to Factor VIII. Anti-Inhibitor Coagulant Complex, Dried This product is prepared from pools of human plasma and then freeze dried. This product is assayed in arbitrary "inhibitor-bypassing units", which are roughly equivalent to its content of prothrombin complex protein. Use of this product is restricted to patients with inhibitors to Factor VIII. More information regarding this product should be obtained from the package insert. Anti-thrombin III (AT-III) This product is a sterile, lyophilized preparation of purified human anti-thrombin III. It is indicated for the treatment of patients with hereditary AT-III deficiency in connection with surgical or obstetrical procedures or when they suffer from thromboembolism. Rh Immune Globulin (RhIG) Rh Immune Globulin is a solution containing anti-D fractionated from carefully screened human plasma by a cold alcohol method. This product is filtered to remove possible viral contaminates. It is used to prevent the formation of anti-D antibodies by suppressing the antibody response to the foreign Rh positive fetal cells in the Rh negative mother. RhIG should be administered as soon as possible to Rh negative, non-immunized mothers (within 72 hours) after birth, amniocentesis, spontaneous passage, or surgical removal of the fetus. If RhIG is not given within the 72 hours, later administration (up to 30 days) should not be withheld. As of January 1984, the American College of Obstetrics and Gynecology recommends that antepartum RhIG be given at 28 weeks gestation to all Rh negative women. When Rh positive red cells or granulocytes are given to an Rh negative patient, the patient should receive RhIG to protect against possible immunization due to red cells in these products. When Rh positive platelets are given to a Rh negative female <50 years of age, the patient should receive RhIg to protect against possible immunization due to red cell contamination in the product. Immune Globulin Intravenous Immune Globin Intravenous is a sterile solution of human IgG protein. It is indicated for the maintenance treatment of patients who are unable to produce sufficient amounts of IgG antibodies. Use of Intravenous IgG may be preferred to that of intramuscular immunoglobulin preparations especially in patients with bleeding tendencies in whom intramuscular injections are contraindicated. It may be used in disease states such as congenital agammaglobulinemia, common variable hypogammaglobulinemia, linked immunodeficiency with hyper-IgM, and combined immunodeficiency. Intravenous IgG is also used in the treatment of ITP, particularly in young adults and children. Intravenous IgG should not be used in individuals who are known to have had an anaphylactic or severe systemic response to Immune serum globulin (Human). Individuals with selective IgG deficiencies should not receive intravenous or any immune globulin preparation. See product circular for indications, contraindications, and dosage and administration. Cytomegalovirus Immune Globulin CytoGam is a sterile lyophilized powder of Ig G. The purified immunoglobulin is derived from pooled adult human plasma selected for high titers of antibody for CMV. CytoGam is indicated for the attenuation of primary CMV disease associated with transplantation. The product is indicated for transplant recipients who are seronegative for CMV and receive marrow or stem cells from a CMV seropositive donor. WinRho SD WinRho SD is a sterile, freeze dried gamma globulin fraction containing antibodies to Rho (D). WinRho SD is prepared from human plasma and is subjected to solvent detergent treatment to inactivate enveloped viruses including Hepatitis B, Hepatitis C and HIV. WinRho may be administered either intramuscularly or intravenously to prevent Rh isoimmunization or to function as an IVIG. The product is routinely used intravenously when the patient would otherwise require multiple doses of Rh immune globulin to cover a large fetal-maternal bleed or an Rh negative patient receiving Rh positive red cells. WinRho also functions as an intravenous immune globulin, but this product only works as an IVIG in Rh positive patients. Requesting Products from the Transfusion Service Lab Transferring Orders to Requisition Promptly after the physician has written an order for tests and/or transfusion, the order is transferred to a Transfusion Service requisition or ordered through CCS and checked by the proper nursing personnel. Notify the Phlebotomy Team if they are to collect the specimen. Every attempt should be made to have the specimens collected as soon as possible and still minimize the number of venipunctures performed on the patient. Once the specimen has been collected, the specimen should be delivered to the Transfusion Service Lab without undue delay. Red Blood Cell Products - Red Blood Cells (leukocyte poor), Red Blood Cells (Washed), Red Blood Cells (Deglycerolized), Autologous Blood and Designated Donor Blood. These products are requested on a manual Transfusion Service requisition by transcribing the physician's order from the chart in the area labeled "physician's order" or are ordered through CCS. Immediately beneath the physician's order indicate when the product is needed for surgery or transfusion and the urgency of the request. The requisition must accompany the patient's specimen (one 10 ml EDTA purple top tube) when sent to the Transfusion Service Lab. Specimens will not be accepted without a proper requisition. Type & Screen and Compatibility tests will be performed prior to issuing the products for transfusion. If a patient's requisitions and specimens are received in the Transfusion Service Lab and additional units are requested, a requisition with the physician's order must be sent or an order placed in CCS. Additional samples may not be necessary, however, the Transfusion Service Lab should be called to see if new specimens are needed. The technologist in the Transfusion Service Lab will advise on the need for specimens and requisitions. Cancellation of orders should be transmitted to the Transfusion Service Lab immediately including cancellation due to death of the patient. Red Blood Cell products will be held for 3 days after the compatibility tests have been completed. Blood units are automatically released 72 hours later and returned to inventory in order to have blood available for other patients. If a patient is being transfused over a period of days, a new sample must be collected every 3 days. In cases of dire emergency when the patient's condition does not warrant waiting for completion of compatibility testing, uncrossmatched blood may be issued. In such cases, an emergency release form must be signed by the physician or by a nurse for the physician. The physician's name must be printed on the form to ensure legibility. This form is supplied by the Transfusion Service Lab and filed with the patient's records in the Blood Bank. Recommended guidelines for ordering red blood cell products: Pre-Operative Orders - Specimens and requests for products on patients scheduled for surgery should be delivered as soon as possible to the Transfusion Service Lab prior to surgery. The Transfusion Service Lab should be given additional advance notice if the patient may require large amounts of blood. Blood can be made available for most problem cases and patients with rare blood types when sufficient notice is given. However, the presence of antibodies may require longer time to have compatible products available. All surgical blood orders should comply with the Maximum Surgical Blood Order Schedule (MSBOS). Routine Orders - Orders should be checked "routine" when the patient is being electively transfused or does not need urgent transfusion. ASAP Orders - Orders should be checked "ASAP" only when the patient may need an urgent transfusion due to risk of bleeding or unscheduled surgery. Specimens and requests will be processed so the products will be ready 1 - 2 hours after receiving the specimens and requests in the Transfusion Service Lab. STAT Orders - Orders should be checked "STAT" only when the product is needed for Stat Transfusion. All requests from the Emergency Department are considered STAT. In most instances, products will be ready in less than one hour, however, products may be issued prior to completion of compatibility testing (see Issue of Uncrossmatched Blood). Issue of Uncrossmatched Blood - When a patient is in need of a Stat transfusion and the situation does not warrant waiting for completion of the Stat procedures, O negative blood will be issued to the physician upon obtaining a signed "Release for Emergency Issue of Blood Products" form. A blood specimen from the patient must be available in the Transfusion Service Lab. Patients presenting problems in finding compatible products often require extended testing which will take additional time no matter how the blood is ordered. Platelets This product is requested on a Transfusion Service requisition by transcribing the physician's order from the chart in the area labeled for the physician's order or ordered in the CCS. Immediately beneath the physician's order, indicate when the product is needed. Once the patient has been Typed by the CCHS Transfusion Service Lab, specimens do not need to be drawn unless requested by the Transfusion Service Lab. Compatibility tests are not routinely performed. By order of the physician, the volume of plasma can be reduced when the patient cannot tolerate excess fluids. Granulocytes The physician should call the Transfusion Service Medical Director to determine the efficacy of this product for the patient and to set up a transfusion schedule for the patient. This product is requested on a Transfusion Service requisition by transcribing the physician's order from the chart in the area labeled for the physician's order or ordered through CCS. Immediately beneath the physician's order, indicate when the product is needed. The requisition must accompany the patient's specimen (one 10 ml EDTA purple top tube) when sent to the Transfusion Service Lab. Type & Screen and Compatibility tests will be routinely performed prior to issuing the product for transfusion. Reduction of plasma volume of this product is undesirable unless the patient already presents a problem of volume overload. Follow recommended Protocol attached to each bag for transfusion instructions. Plasma Products - Fresh Frozen Plasma and Cryoprecipitate These products are requested on a Transfusion Service requisition by transcribing the physician's order from the chart in the area labeled for the physician's order or ordered through CCS. Immediately beneath the physician's order, indicate when the product is needed. Once the patient has been Typed by the CCHS Transfusion Service Lab, specimens do not need to be drawn unless requested by the Transfusion Service Lab. Compatibility tests are not performed. Commercial Plasma Products-Factor VIII, Factor IX, Prothrombin Complex (Factor IX),Anti-inhibitor Coagulation Complex and Antithrombin III These products are requested on a requisition by transcribing the physician's order from the chart in the area labeled for the physician's order or ordered in CCS. These products must be approved by the Transfusion Services Medical Director or his designate. Compatibility tests are not performed. Immune Globulin Products - RhIG, Immune Globulin Intravenous, Cytomegalovirus Immunoglobulin and WinRho SD These products are requested on Transfusion Service requisition by transcribing the physician's order from the chart in the area labeled for the physician's order or ordered through CCS. Compatibility tests are not performed. Guidelines for Antepartum use of RhIG. Antepartum RhIG is given to Rh Negative women at 28 weeks gestation. Patient must be sent to the Medical Arts Pavilion Outpatient Laboratory or Clinic with a written order for an antibody screening and the administration of RhIG The RhIG will be administered prior to the screening test being completed. This spares the patient having to wait while the tests are completed. Only in a rare instance is a patient likely to receive the RhIG unnecessarily. If the patient's insurance coverage requires that the type and screen be performed at another laboratory, it is the responsibility of the ordering physician to confirm that the patient is a RhIg candidate. For these patients, written order to administer the RhIg is necessary. Guidelines for use of RhIG following Diagnostic Amniocentesis All Rh negative women undergoing amniocentesis should be evaluated as RhIG candidates. Transfusion Service Lab records must confirm patient is Rh negative. Patients not having records in the lab to confirm their type should have a RhIG Evaluation performed. Guidelines for use of RhIG following Aborted Pregnancy. All Rh negative women aborting should be evaluated as RhIG candidates. A RhIg Evaluation should be done prior to releasing the product on the day of the abortion. Guidelines for Post Partum use of RhIG Labor and Delivery (L&D) will notify the Transfusion Service Lab of all Rh negative women admitted to their department. L&D will send cord blood specimens from every neonate delivered by an Rh negative female to the Transfusion Service Lab for type and DAT. After testing of the cord blood has been completed, the Transfusion Service Lab will inform the nursing station of the results. Those postpartum mothers who need to be administered RhIg will have a blood sample drawn and sent to the Transfusion Service Lab. Candidates who should receive RhIG will be issued the standard dose of RhIG (300 ug of anti-D). Any evidence of a large fetomaternal bleed during the RhIG Evaluation will result in calculation of the proper dose in the Transfusion Service Lab and additional vials will be issued for the patient. After the RhIG has been injected, the chart copy of the Transfusion tag must be placed on the patient's chart and the Transfusion Service Lab copy returned to the Transfusion Service Lab. Collection of Specimens Good transfusion therapy relies on proper patient identification and specimen collection. The following guidelines were designed to ensure positive identification of the patient and reduce the possibility of errors occurring. These guidelines apply to all specimens collected for use in the Blood Bank Department. Prior to collection of any specimens, the proper requisitions for ordering tests must be stamped with the addressograph plate or handwritten with the proper patient information. CCS requisitions have the patient information already printed on them. Minimum identification on all specimens and requisitions is: Patient's full name Medical Record, Emergency Department or Social Security number Date and time of collection. Signature of phlebotomist (label on specimen must be initialed). Specimens submitted to the Transfusion Service Lab may be collected by a physician, staff nurse, member of the IV Team or member of the Phlebotomy Team. The patient must have an identification bracelet on their wrist or ankle prior to collection of specimens. This applies to all in-patients and to those out-patients having specimens drawn for transfusion. Out-patients having diagnostic tests performed (non-transfusion specimens) do not need identification bracelets. Specimens for use in the Blood Bank must not be collected if the patient does not have an identification bracelet on. If a bracelet is removed for any reason, the person removing the bracelet or a person who observed its removal must place it on or affix it to the patient. This is of utmost importance since a physician must take complete responsibility for transfusion of a patient who does not have an identification bracelet attached to them. If the physician does not want to take the responsibility, a new identification bracelet must be attached to the patient, new specimens drawn, and submitted for repeat testing. The repeat testing will be charged to the patient's account. Identification information on the bracelet must be identical with the information on the requisition and the specimen tube. Any discrepancies must be corrected prior to drawing the specimen(s). The phlebotomist must confirm the patient identifying information on the identification bracelet, requisition, and specimen labels prior to drawing the specimen, and must sign his/her name on the requisition to document the identification procedure. Deliver the specimens without delay to the Transfusion Service Lab. All specimens for compatibility testing must be accompanied by a requisition ordering the test(s). Specimens for compatibility testing are used for 3 days. Check with the Transfusion Service Lab if there is any question about specimens for compatibility testing. Transferring Patients The Transfusion Service Lab should be notified if a patient who has blood products being prepared or held for transfusion or surgery is transferred to another Hospital. In order to assure continuity of care, prevent undue delays in providing blood products, and prevent duplicate testing and charging for the patient, the following guidelines are recommended: From the Emergency Department Any patient transferred from the Emergency Department to another unit or Hospital must keep their Emergency Department identification bracelet on for 3 days, otherwise, products that are available must be retested with a new specimen. The Emergency Department should notify the Transfusion Service Lab when a patient is being transferred and to which Hospital the patient is going. The Transfusion Service Lab will arrange to have available blood products transported independently or with the patient. Products transported with the patient must be immediately sent to the Transfusion Service Lab upon arrival. (See Note). The unit receiving the patient should contact the Transfusion Service Lab to inform them that the patient has arrived and confirm that the blood products ordered in the Emergency Department are available. Between CCHS Hospitals A unit clerk or other personnel from the nursing station should notify the Transfusion Service Lab when a patient is being transferred. The Transfusion Service Lab will arrange to have available blood products transported independently or with the patient. Products transported with the patient must be immediately sent to the Transfusion Service Lab (See Note). The unit receiving the patient should contact the Transfusion Service Lab to inform them that the patient has arrived and confirm that the blood products ordered at the other Hospital are available. NOTE: The Transfusion Service Lab may also be sending the patient's specimens with the blood products and it is of the utmost importance that the entire package be delivered to the Transfusion Service Lab without delay. Equipment needed for Transfusing Therapeutic Products A. B. C. Obtain the following from the Nursing Department 1. I.V. pole 2. Tourniquet 3. Adhesive tape 4. 70% alcohol prep and/or iodine tincture 2% sterile Sepps 5. Dry Sterile 2” x 2” sponges 6. Proper needle or plastic catheter 7. Covered arm board All products for IV use must be filtered prior to infusion. Obtain one of the following recipient sets from Central Service. 1. Blood Recipient Set (170 micron) - used for Red Blood Cell products; may be used for plasma when a red cell product is also transfused. 2. Blood Component Recipient Set (170 microns) - used for plasma, platelets, granulocytes and cryoprecipitates given by I.V. drip. 3. Blood Component Infusion Set (170 microns) – used when transfusing via I.V. push small volumes of Factor VIII, cryoprecipitate, platelets, etc. (Stocked in Transfusion Service Lab Only). 4. Microaggregate Filter (20 micron without integral tubing) a. Central Supply stocks the Alaris 20 Micron High Capacity depth filter and the 20 Micron Pediatric depth filter. b. The 20 Micron Pediatric filter is used routinely for infant transfusions. (see 5 below). c. The 20 Micron High Capacity filter is used in adults and children for fast, massive transfusions. It is used during surgery and in the Emergency Department for trauma patients. An IV tubing set or a blood recipient set must be attached to the 20 Micron High Capacity filter for utilization. d. These filters must not be used to transfuse granulocytes. e. Commercial microaggregate filters are available in 20 to 40 microns with or without integral tubing. The types of filters available are either depth, screen or a combination of depth and screen. 5. Neonatal syringe set (with 150 micron filter) – Recently there has been manufacturing delays with the 20 micron pediatric filter (see 4 b. above). When supplies are jeopardized, Christiana Care also provides the chartermed neonatal syringe set. This device includes a 150 micron filter attached to a syringe and is designed for removal and filtration of red blood cells into the syringe for administration to infants. This device is also available in central supply. Leukoreduction filters 1. If leukopoor red cells are not available from the Blood Bank, a red blood cell leukocyte reduction Y-administration set will be issued from the Blood Bank with the rbc. These are intended for the leukocyte reduction of red cell products by direct 2. in-line filtration during transfusions. Some platelet products will be issued from the Blood Bank with a platelet leukocyte reduction Y-administration set. These are intended for the leukocyte reduction of platelet products by direct in-line filtration during transfusion. Most single donor platelet pheresis products are leukoreduced during processing and will not require filters during the infusion process. Preparing for the Transfusion A. B. C. IV Solutions 1. Isotonic Saline, Normal Saline - 0.9% NaC1 for IV use only, is the only IV solution which may be used in a blood recipient set before, during, or after transfusion of a blood product. 50 ml of normal saline may be added to RBC to reduce viscosity. 2. Solutions containing dextrose may not be used as they cause hemolysis of red blood cells. 3. Lactated Ringers (with or without dextrose) may not be used because of the Ca content which also causes red blood cells to clump. 4. Any solution may proceed or follow a blood transfusion provided that the blood recipient set used in transfusing the blood product is not used. Special Precautions 1. All products given intravenously must be administered through a blood set containing a filter. 2. Do not store blood products in an un-monitored refrigerator or at room temperature in any department. If there is any delay in starting the transfusion, return the unit immediately to the Transfusion Service Lab. Any blood product not returned to the Transfusion Service Lab within 30 minutes of issuing cannot be re-issued nor can the unit be released to another patient. Blood stored in monitored refrigerators or packed in wet ice by the Transfusion Service Lab are not subject to the 30 minute limit from time of issue, however, if the blood is removed for transfusion, the 30 minute limit will apply from the time it is removed. 3. Absolutely no drugs are to be added to a unit of blood or a blood component. 4. Before obtaining the unit from the Transfusion Service Lab, check and verify the following items in the patient's chart. a. Verify the physician's order. b. Check for a signed and witnessed consent for transfusion. The permit must be signed prior to starting the transfusion. In emergency situations, a written order must be obtained from the physician assuming responsibility for the transfusion if consent from patient or relative cannot be obtained. c. Check the chart for any previous Blood Bank reports. d. Note if previous records confirm the patient's blood type. Obtaining Products from the Transfusion Service Lab 1. Blood products should be obtained from the Transfusion Service Lab after all other supplies are available in the patient’s room. 2. D. The IV nurse will be responsible for obtaining products(s) from the Transfusion Service Lab only if she is starting the transfusion. Staff members who are starting transfusions are responsible for obtaining the product from the Transfusion Service Lab. Only nurses who have received additional training in transfusion therapy from the IV Team are permitted to start transfusions. 3. Upon completion of pre-transfusion testing, the Transfusion Service Lab will call the floor. a. The floor in turn will call the IV nurse, if she will be starting the transfusion. i. The IV nurse will call the Transfusion Service Lab with the patient's full name, medical record number and type of product to be administered. The Transfusion Service Lab will then dispense the product(s). ii. If two (2) patients with established IV lines acceptable for transfusion are to receive red cell products, the IV nurse may take the product for both patients out of the Transfusion Service Lab at the same time. iii. For those patients who must have an IV started in order to administer the blood, only one (1) unit at a time may be taken out of the Transfusion Service Lab. iv. The IV nurse may continue to take a plasma component and red cell product out of the Transfusion Service Lab on two(2) different patients, whether an IV line must be established or not, however, the red cell product must be started first. v. IV nurses only may take one type of component to a third patient in any of the situations above. b. If the floor nurse will be starting the transfusion, she will send another nurse, a unit clerk, or a service assistant to pick up the blood or product(s). Blood can be sent through the tube system if it is available. If received via the tube system, the transporter must sign the transfusion tag indicating that the unit received is identified for the intended recipient. It is necessary to call the blood bank with the patient's name, medical record number and products requested. i. The person picking up the product(s) must present an addressograph label of the patient who will be transfused to the clerk or tech in the Transfusion Service Lab. ii. The type of product requested must be written on the label to confirm the type of product ordered by the patient's physician. iii. "Transport" personnel may pick up red cell products for two different patients at one time. However, they must be taking the products to patients on the same or adjoining nursing units. iv. Red cells for one patient and one type of component (platelets, FFP, or cryo) may be issued for another patient, or one type of component may be issued for two different patients. v. If the patient is on dialysis, 2 red cell units for the same patient may be dispensed at one time. Confirmation of Patient Identity Prior to Transfusion At the patient's bedside the transfusionist and one other licensed staff member must verify and confirm the patient's identity. The following steps are the minimum required for identifying the patient. It is the responsibility of the transfusionist for making any additional checks deemed necessary. 1. The transfusionist should obtain verbal identification from the patient when possible, i.e., "What is your name?" 2. The staff member assisting in the identification must be another licensed CCHS professional. He/she should confirm the identity of the patient by visual recognition and by inspection of the patient's identification bracelet affixed to the patient. (NOTE: Patients should not be transfused unless the identification bracelet is affixed to the patient). 3. The transfusionist (RN) checks the following with the identifying assistant (another licensed CCHS professional): Blood bag vs. Transfusion Tag.: Check the unit number, blood product, compatibility of ABO and Rh, and expiration date. The ID assistant should read this information aloud to the transfusionist, then repeat by having the transfusionist read the information back to the ID assistant. At bedside, Transfusion tag vs. the patient identification armband: Check the patient’s medical record number, newborn ID, or ED number, and the patient’s full name. The ID assistant should read this information aloud to the transfusionist, then repeat by having the transfusionist read the information back to the ID assistant. 4. Any discrepancies must be immediately resolved or the unit must be returned to the Transfusion Service Lab without delay. 5. Performance of this procedure must be documented on the Transfusion tag. The transfusionist's signature must appear beneath the verification statement on the Transfusion tag. The staff member assisting in the identification must sign their name beneath the transfusionist's signature. 6. The Transfusion tag must not be detached from the unit while the product is being transfused. Exception: For patients in isolation, leave the entire tag on the outside of the door after confirming the patient's identity. Starting the Transfusion A. Using a Straight Recipient Set 1. Transfusionist must gently mix the unit. 2. The blood recipient set should be inserted into the unit by performing the following steps: a. Close all clamps. b. Push coupler cover of transfusion tubing toward flange and twist to break seal. Do Not Remove. c. Pull apart tabs to expose one of the ports in the unit (outside port preferred). d. Remove coupler cover and insert coupler using a twisting motion. Insert the coupler as far as possible maintaining sterility of the system. e. To prevent puncturing the unit with the coupler of the recipient set, the following has been recommended: i. Hang the unit from an IV pole. 3. 4. 5. 6. 7. ii. Grasp port with tabs open. Hold coupler immediately beneath flange. Insert coupler of recipient set as far as possible with a twisting motion until firmly seated. Do not grasp filter, twisting the filter may cause the seal to break between the filter and coupler. Use of this technique causes pressure to be exerted by the blood or plasma against the sides of the unit resulting in a clear entrance of the coupler into the unit. CAUTION MUST BE USED. Ambient air should never enter the bag. Fill the filter chamber completely using one of the following methods: a. Remove unit from pole b. Squeeze and hold unit upright, open clamp to fill chamber completely. c. Close clamp and hang unit back on IV pole. Or a. After inserting coupler into the unit, squeeze filter chamber. b. Release filter chamber to permit partial filling of chamber. c. Squeeze and release filter chamber until completely filled. Fill the drip chamber 1/4 to 1/2 full by squeezing and releasing the drip chamber. If drip chamber should overfill, then invert unit, squeeze both filter and drip chamber. Flow clamp should remain closed. Rehang unit and check that filter and drip chamber are properly filled. Drip chamber visibility will return in approximately one minute. Never remove recipient set from the bag. Remove protector cap from needle adapter. Release clamp and expel all air from tubing. Close clamp and keep needle adapter sterile. Apply a tourniquet and select a vein. Release tourniquet. After selection of the vein most suitable for venipuncture, the site should be prepared by using venipuncture site preparation for donors (See BB Procedure Manual) or by using the following procedure: a. Scrub the venipuncture site with a sterile alcohol swab-isopropyl alcohol, 70%. Use enough pressure to raise a redness in an area 1 1/2 to 2 inches in diameter. Dry with a sterile 2 x 2 gauze sponge. b. Using a sterile iodine tincture, 2% with alcohol 47% "Sepps", start at the site of the intended venipuncture and apply the solution in concentric circles to cover an area of at least 1 1/2 inches in all directions. Always apply at the outside of the circle, never go back to an inner circle. Allow solution to air dry. (The minimum drying time in emergencies is 30 seconds). c. Using a sterile alcohol swab-isopropyl alcohol 70%, remove the iodine tincture. Start at the site of the intended venipuncture and work out in concentric circles as in the preceding step. Several alcohol swabs may be needed. d. Dry area with a sterile 2 x 2 gauze sponge, being careful not to contaminate venipuncture site. e. Keep venipuncture site covered with a sterile 2 x 2 gauze sponge until ready to insert the intravascular device. The prepared skin should not be touched until after the device has been inserted beneath the skin. Apply tourniquet, perform venipuncture, check for return flow, and release tourniquet. If a catheter was inserted, remove the style at this time. Attach the needle adapter of the recipient set to the needle or catheter. 9. Secure needle or catheter in place with tape. Cover venipuncture site with a doubled dry sterile 2 x 2 gauze sponge and tape in place. 10 The rate of infusion of a blood product depends on the clinical status of the patient. The rate should be no slower than four hours per unit and the flow rates serve only as guidelines. See Transfusion Rates. Adjust flow rate to 1 ml/min (15 drops per minute). This flow rate should be maintained for the first five to twenty minutes. Flow rates for neonates and infants are slower, see suggested flow rates under Transfusion Rates. During this time, remain with the patient and observe for signs of a transfusion reaction. Most hemolytic reactions will occur within the first thirty minutes. 11 Increase the flow rate after the first five to twenty minutes to a flow rate of 3 ml/min or to a rate prescribed by the physician. Before leaving, make the patient comfortable. Report the patient's condition to the nurses responsible for monitoring the patient. The nurse should check on the patient every fifteen to thirty minutes while the patient is being transfused. B. Using a Y-type Recipient Set 1. Obtain the necessary equipment for starting an IV including a Y-type recipient set and a 250 ml bag of normal saline. (NOTE: 50 ml of normal saline can be added to RBC to reduce viscosity). 2. Close all clamps on the recipient set 3. Insert one lead of the Y-type recipient set into the saline bag. 4. Prime the filter and tubing with saline. 5. Apply a tourniquet and select a vein. Release tourniquet. 6. Prepare the venipuncture site as described in step 7 in the section on using a straight recipient set. 7. Apply tourniquet, perform venipuncture, check for return flow and release tourniquet. 8. Secure needle or catheter in place with tape. Apply a 2 x 2 dressing and tape. 9. Open clamp from saline bag and clamp beneath filter, establish a very slow drip rate. 10. Obtain product from the Transfusion Service Lab. 11. Perform patient identification by following the procedure for "Confirmation of Patient Identity Prior to Transfusion" 12. Gently mix the unit. 13. Attach unit to the recipient set following steps 2b. thru 2e. in the section on using a straight recipient set. 14. Prime lead from the product by opening and closing clamp beneath product. 15. Close clamp under saline bag and open clamp under product. 16. Regulate rate of infusion by adjusting clamp beneath the filter. 17. Adjust flow rates as described in steps 10 and 11 in the section on using a straight recipient set. C. Use of Fenwal - Blood Warming System 1. Attach the blood warmer to an IV stand by means of the brackets on the back of the warmer. Plug the warmer into a 110-120V outlet. 2. Newer models have on-off switches; turn switches on. 3. Wait approximately two minutes for temperature indicator to reach the green operating range area. 4. Check alarm and breaker systems as directed on the back of the warmer. Record on Q.C. record. If any problems, warmer should not be used. 5. Close roller clamp of blood warming bag and attach warming bag to offset pins on inner panel of the Blood Warmer. Close and lock door of warmer. DO NOT OPEN DURING USE. 6. Prepare the unit for transfusion. Follow steps 1-4 when using a straight set, steps 1-3 when using a Y-type recipient set. 7. Attach recipient set adapter to bottom part of Fenwal Blood Warming Bag. A pressure infuser may be used if necessary. NOTE: Temperature gauge must be in operating range before transfusion. 8. Open clamp on tubing of blood warming bag. Allow blood to flow into bag by opening clamp on the recipient set. Squeeze and keep outlet chamber flattened until blood appears in outlet tubing of warming bag. When blood appears in outlet tubing, close clamp of blood warming bag and release chamber. Fill chamber with blood to or above the index line located on the side of the warmer. If a Y-type recipient set is used, prime recipient set and blood warming bag with saline. 9. Open clamp of warming bag to expel air from tubing. 10. Proceed with venipuncture and transfusion as directed in steps 6-11 when using a straight recipient set, steps 5-17 when using a Y-recipient set. NOTE: If the temperature indicator goes beyond the green area into the red area, either turn power switch off or unplug unit from electrical outlet immediately. Any problems which cannot be corrected should be reported to an IV nurse. D. Use of Fenwal - Pressure Infuser - Two sizes of pressure infusers are manufactured, 600 ml and 1000 ml capacity. Only the 600 ml capacity should be used with blood product units. 1. Confirm connection of bulb hand pump and tubing assembly. Close air valve. 2. Insert plastic non-vented blood container with primed recipient set attached. Insert through lower opening of mesh panel. The label on the unit should face away from the mesh panel. 3. Insert unit until its hanger slot is past the mesh panel. Thread the fabric suspensions trap through the unit hanger slot and the Fenwal tab on infuser. Suspend infuser and unit by fabric strap. DO NOT SUSPEND BY HANGER SLOT OF UNIT. 4. Open flow clamp wide open and observe drip rate. Slow or negligible drip rates may indicate: a. unit not gently mixed prior to priming the recipient set b. small fibrin clots blocking the port in the unit c. an occlusion in the tubing (mechanical or physical) d. improperly positioned intravascular device 5. For pressure infusion, inflate to desired pressure as indicated on gauge. (NOTE: The pressure gauge is an approximate indicator only. The product is not designed for use in monitoring arterial or venous pressure). Do not exceed 300 mm of HG on gauge. Over inflation may damage the infuser. 6. Infusion flow rate may be adjusted by using the recipient set clamp. Pressure infusion may be maintained by squeezing bulb pump as the product is infused. 7. To remove empty unit, open air valve to rapidly deflate infuser. E. Use of Tycos - Pressure Infuser – Primary usage in Emergency Dept 1. 2. 3. 4. 5. 6. 7. Turn pressure infuser crank handle clockwise to open position. Insert plastic, non-vented blood container with primed recipient set attached. Insert unit through lower opening and attach to metal hook. The label on the unit should face away from the clear plastic. Turn crank handle counterclockwise until it will no longer turn. Infuser is now loaded and ready for use. No further adjustments need be made. Use metal loop in top handle for attachment to IV stand. Open flow clamp wide open and observe drip rate. Slow or negligible drip rates may indicate: a. unit not gently mixed prior to priming the recipient set b. small fibrin clots blocking the port in the unit c. an occlusion in the tubing (mechanical or physical) d. improperly positioned intravascular device. To remove the empty bag, turn pressure infuser crank handle clockwise to the open position and remove bag. Transfusion Rates 1. The rate of infusion depends upon the clinical condition of the patient being transfused. The flow rates listed in the table will normally result in complete transfusion of the unit as indicated by the transfusion time. Product Red Blood Cells Granulocytes RBC (Deglycerolized) Fresh Frozen Plasma Platelets: Apheresis Random Concentrate Factor VIII/Factor IX Factor VIII (Continuous) Intravenous Immunoglobulin Quantity (unit) 1 1 1 1 1 Pool of 6-10 50 ml 1 vial Specified by M.D. 1 vial Rate ml/min 3 Transfusion Time 3 10 1-2 hours 50-60 minutes 1 - 2 hours 15-25 minutes 5-6 10 10 See package insert Specified by M.D. 30-45 minutes 30-45 minutes 5-10 minutes I.V. push in most instances See #2 below See package insert As ordered (usually 12 hours) 1 - 1 1/2 2. 3. 4 Continuous infusion of Factor VIII - continuous infusion of Factor VIII must be performed using a volume control device, such as the Alaris Pump. The diluent must be Normal Saline. No dextrose solutions may be used as the diluent. The order should specify the number of units (IU) of Factor VIII to be infused and the volume of diluent desired. The infusion should be monitored at least hourly, and the rate adjusted as needed to maintain a steady even flow through the specified infusion period as ordered by the physician. A major side effect that may be seen with this type of infusion is localized phlebitis. Nursing personnel should carefully monitor the patient for this symptom. If localized phlebitis occurs, the I.V. site must be changed and the ordering physician should be notified. Continuous infusion must not be used with Factor IX or Cryoprecipitate unless specifically ordered by the Medical Director or his designate. Flow rates should be slower than those suggested and times of completion of the transfusion will be longer in the following cases: a. Infants and children b. Adults over age 60 c. Cardiac and Pulmonary disease patients d. Chronic anemia patients In these cases, the flow rate should be designated by the physician. If not written on the chart, request information from the physician. The following flow rates are suggested for neonates and infants, based on the weight of the child: Weight of Child Flow Rate Less than 1.5 Kg 0.5 ml/min 1.5 Kg or greater 1.5 ml/min Monitoring Patients During Transfusion A. Red Cell and Granulocyte Transfusion 1. Gently mix blood as often as necessary. 2. Remain with the patient for the initial 20 minutes of transfusion to assess suspected reaction. 3. Check patient at least every 30 minutes for any untoward effects, discomfort, infiltration at needle site and for signs of reaction. 4. Check patient's temperature, pulse, respiration, and the flow rate of the transfusion at 15 minutes and 30 minutes, then every hour during the transfusion and one hour post transfusion. Transfusion should be completed within four hours. If vital signs remain in the normal range, then vital signs are taken as per routine. Record the values on the appropriate sheet on the patient's chart. Record hourly flow rate. 5. Visually inspect and record all voiding at the start and during the transfusion as to time, amount, and color. This should be continued for at least 12 hours posttransfusion. This is a very important clinical notation if an investigation for a hemolytic transfusion reaction is required. 6. B. Any portion of blood not administered to the patient MUST be returned to the Transfusion Service Lab immediately. Reasons for not completing the transfusion must be written on the copy of the Transfusion tag returned with the unit. DO NOT REMOVE the recipient set from the unit if the transfusion is stopped prior to completion. The unit must be kept sterile, including the recipient filter set by placing a covered sterile needle on the end of the tubing. If for some reason, the recipient set has been contaminated, please note on the copy of the Transfusion requisition returned to the Transfusion Service Lab with the unit. 7. Patients who are being transfused should be accompanied by a qualified nurse when transported to another area or between hospitals. This is especially important when the patient is going to an area where a qualified nurse is not present to monitor the transfusion. Plasma, Platelets, and Pharmaceutical Products 1. Remain with the patient for the initial 20 minutes of infusion. 2. Check the patient for any untoward effects, discomforts, or infiltration at needle site. Observe the patient frequently throughout the transfusion. 3. Any portion of a component not administered to the patient MUST be returned to the Transfusion Service Lab immediately. Reasons for not completing the transfusion must be written on the copy of the Transfusion tag returned with the product. 4. If clinical lab tests were ordered to be performed following transfusion, notify phlebotomist or appropriate staff member for collection of samples. 5. Whenever possible, a qualified nurse should accompany the patient if transported to another area or hospital while being transfused. "Add Ons" and Discontinuing the Transfusion 1. 2. When an additional unit of blood or a plasma component is to be transfused immediately upon completion of the first unit, the following steps should be followed: a. The recipient set from the first unit may be used. If fibrin clots appear to clog or fill the filter, a new recipient set should be used. The recipient set should be disconnected at the needle hub when starting the next unit through a new set. Maintain the sterility of the set being replaced by placing a covered sterile needle on the needle adapter. b. When reusing the recipient set, hang the unit on the IV pole. Grasp the tabs protecting the port, pull them apart, and fold back to expose the sterile port. Do not contaminate the sterile port. c. Close the clamp on the recipient set from the completed unit and remove the unit from the IV pole. d. Remove the recipient set from the empty pack, being sure to maintain sterility, insert the coupler taken from the transfused unit into the port of the unit on the IV pole. Insert the coupler with a twisting motion until it is firmly seated. NOTE: Every additional unit must be checked vs. the patient ID band by the transfusionist and an identifying assistant, just like the first unit. Discontinue the transfusion by performing one of the following: a. Add any IV solution after changing the recipient set Or b. Remove the needle from the patient's arm and apply pressure with a dry sterile gauze. Place a pressure dressing on the patient's arm after all bleeding has stopped. If a patient in an isolation area has a transfusion reaction, the unit and attached recipient set must be sent to the Transfusion Service Lab. The unit and attached tubing must be placed in a clear plastic bag and sealed. Return the unit and the lab copy of the Transfusion tag to the Transfusion Service Lab. Charting the Transfusion 1. 2. The transfusionist must chart the following information on the transfusion requisition and Water Balance Sheet (or ICU Flow Sheet) after starting the transfusion: a. On the transfusion tag: i. Transfusionist signature certifying proper identification of the patient, the product, and information on the tag attached to the product. ii. Signature of licensed staff member assisting with the identification at the patient's bedside. iii. Date and time started b. .On the Water Balance Sheet (or ICU Flow Sheet) at the patient's bedside i. Date and Time unit was started ii. Product and amount iii. CCHS number from unit iv. Type of intravascular device used and where it was inserted v. Signature and title of transfusionist when venipuncture is performed c. The Medication Administration Record (M.A.R.) should be used to chart infusion of Factor VIII, Factor IX complex, and Immunoglobulin. If volumes are 50 ml or greater, they must also be charted on the Water Balance Sheet. Upon completed infusion of the product or if the transfusion was stopped prior to complete infusion, i.e. a transfusion reaction, the nurse who discontinues the transfusion must chart the following on the transfusion tag and on the Ancillary and Nursing Patient Progress Report. a. On the transfusion tag: i. Indicate whether or not the entire unit was transfused. If "no" is checked, also indicate the approximate volume transfused. ii. Indicate whether or not a transfusion reaction was noted. iii. Enter the date and time the transfusion ended or was stopped. iv. Place the chart copy of the transfusion tag on the "Laboratory Results" form in the patient's chart. b. On the Ancillary and Nursing Patient Progress Report (may be charted by the nurse responsible for the patient at the end of the transfusion): i. Patient's general condition at the end of the transfusion ii. Patient's 1 and 24 hour post-transfusion TPR c. If the transfusion was stopped to investigate a reaction, also include on the Ancillary and Nursing Patient Progress Report: i. Time reaction occurred ii. Time product discontinued iii. iv. v. vi. vii. d. Patient's symptoms (be specific) Type of IV solution and time administered Time IV nurse or Transfusion Service notified Time post-transfusion specimens were collected Time physician was notified, name of physician, and whether or not orders were received. viii. Include BP with post-transfusion TPR ix. Amount, results of visual inspection, and time of all voiding. (NOTE: Technologist may request specimen be sent for urinalysis as part of reaction workup). Any additional pertinent data relating to the transfusion or reaction investigation. Adverse Reactions to Transfusions Any untoward symptoms noted by the patient or attendant during any transfusion constitutes a Transfusion Reaction. This must be evaluated STAT by the patient's physician. The I.V. nurse or transfusionist and the Transfusion Service Lab should also be notified STAT so the Transfusion Reaction work-up can assist the physician's evaluation. The following are definitions/descriptions of the recognized types of transfusion reactions: A. Hemolytic Reactions 1. Acute Hemolytic Reactions – Acute hemolytic reactions are the result of transfusing incompatible or abnormal red cells and are characterized by their prompt destruction. Symptoms may include chills, a burning sensation along the course of the vein being used for the infusion, flushing of the face, fever and headache, pain in the lower back, and often an oppressive feeling in the chest. Shock may be a prominent feature. Severe reactions without clinical symptoms may occur in patients under anesthesia, often seen as abnormal oozing of blood, hemoglobinuria, and a drop in blood pressure. Hemolysis may be primarily intramuscular with hemoglobinemia/uria or extravascular producing icterus. Severe hemolytic reactions usually cause renal damage. 2. Delayed Hemolytic Reaction - Delayed hemolytic reactions are the result of transfusing incompatible blood which caused an amnestic immune response to either a previous transfusion or pregnancy. The amount of antibody in the patient's plasma is too low to be detected in pre-transfusion serological testing. The antibody may not be detected until 2-20 days after the transfusion when a rapid increase in the antibody concentration occurs followed by rapid destruction of the donor red cells. Typically, there are no clinical symptoms at the time of transfusion. Several days after the transfusion, the following clinical pathology may appear: 1) a positive DAT, 2) spherocytosis noted in blood films, 3) a fall in the hemoglobin concentration, 4) jaundice, and/or hemoglobinemia/uria. Clinical symptoms may accompany this reaction if the hemolysis is sufficiently rapid. B. Non-Hemolytic Reactions 1. Febrile Reaction - May be caused by leukocyte incompatibility, leukocyte cytokines, or by bacterial pyrogens. Reactions are characterized by chills and varying degrees of fever during transfusion. The fever is usually self-limited and rarely biphasic. Symptoms often do not develop for 60-90 minutes or later following the start of the transfusion. Flushing may develop within five (5) minutes if the patient has a potent leukocyte antibody. Fever may be accompanied by headache, flushing, tachycardia, etc., and discomfort may persist for as long as 8-10 hours. 2. Anaphylactic and Allergic Reactions - When platelets or plasma are transfused, the recipient receives many different plasma proteins and alloimmunization to a certain plasma protein may cause a reaction. Reactions may be severe, characterized by flushing, dyspnea, and hypotension; much more common are mild reactions characterized by urticaria (hives). Allergic reactions are relatively frequent and are seldom serious, but must be noted and treated. Chills, fever and edema may accompany eruption. 3. Graft-Versus-Host (GVH) - GVH may develop in immunocompetent or immunodeficient patients when transfused viable T-lymphocytes present in cellular blood components engraft, proliferate and react against host tissues. GVH as a result of blood transfusion may be fatal. Symptoms include fever, skin rash, liver dysfunction, severe diarrhea, bone marrow suppression and infection. GVH can be prevented by irradiating all lymphocyte containing blood components prior to transfusion. 4. Circulatory Overload - Overloading produces a rise in central venous pressure, an increase in the amount of blood in the pulmonary blood vessels, and a diminution in lung compliance. Circulatory overload is characterized by headache, tightness in the chest, and dyspnea, dry cough, and frothy sputum. Circulatory overload during transfusion must be treated as a grave matter and a very close watch of the patient should be kept during the next 12 hours 5. Alloimmunization - Immunization to cellular, protein, or other alloantigens is an unavoidable risk from transfusion of blood products. Patients may become sensitized and produce antibodies to any antigen which they lack, and which is present in the transfusion product. The risk of sensitization can be estimated to be approximately 1% for each unit of blood transfused. Following antibody formation, future transfusions may be more difficult since it will be necessary to select blood products lacking the corresponding antigen. 6. TRALI – Transfusion related acute lung injury may occur if leukocyte antibodies are present in the donor plasma. Such antibodies may cause leukocyte aggregation in the lungs of the recipient and subsequent fluid collection. C. Disease Transmission 1. Post-Transfusion Hepatitis (PTH) - Transmission of hepatitis is the most frequent serious complication of blood transfusion, constituting a hazard to the health and life of the recipient. Clinical symptoms range from very mild subclinical hepatitis to severe fatal liver necrosis. All blood products carry a risk of transmitting hepatitis except those which are exposed to high temperatures, filtration or solvent detergent treatment during their manufacture (such as albumin, gamma globulin, and plasma protein fraction). The degree of risk depends on the number of donor exposures the patient has. Of the several viruses known to cause hepatitis, hepatitis C is the most prevalent cause of PTH followed by hepatitis B virus. Investigation of PTH involves the patient's clinical symptoms, incubation period and serological study of hepatitis markers. 2. Transfusion Associated Cytomegalovirus (CMV) - Newborns, especially preemies may be at high risk for CMV infections associated with transfusion of blood products. CMV infections may result in serious after effects or death in the newborn. Adults, except those that are immuno-compromised, are at lower risk since most have had silent CMV infections at some time in their lives and have produced antibodies to the virus. Since the virus is carried in leukocytes, it is possible that infection would be less likely if blood components that are leukocyte-poor are used. 3. Bacterial Contamination - The clinical syndrome of a reaction due to the infusion of contaminated blood is dramatic and its detection is important. The reaction is characterized by shaking, vomiting, and bloody diarrhea. As a rule, the patient goes into profound shock. The shock syndrome is peculiar in that it is accompanied by dry flushed skin and fever ("red shock"). Symptoms appear after a latent period of about 30 minutes and follow infusion of as little as 50 ml of blood. 4. Acquired Immunodeficiency Syndrome (AIDS) - The disease caused by a retrovirus called human immunodeficiency virus (HIV). This virus can be transmitted through transfusion of blood and blood products, however, immunoglobulin, albumin, RhIg, and Hepatitis B vaccine have not been implicated in AIDS transmission. The virus infects T-helper (T4) lymphocytes which causes loss of immune function and regulation. The long-term prognosis for most persons infected with HIV is unknown, but the mortality of full-blown AIDS is very high. D. Temperature Guidelines - All elevated temperatures are of importance in reporting any untoward effects resulting from transfusion. 1. If the patient's temperature prior to transfusion of a unit is 37.2oC (99oF) or below, a temperature rise to 38oC or above must be reported to the Transfusion Service Lab and/or I.V. nurse as a suspected reaction by the nursing personnel responsible for the patient and the monitoring of the transfusion. 2. If the patient's temperature prior to transfusion of a unit is above 37.2oC (99oF), any temperature rise of 1.0oC must be reported to the Transfusion Service Lab and/or I.V. nurse as a suspected reaction by the nursing personnel responsible for the patient and the monitoring of the transfusion. 3. Orders to “transfuse despite temperature” are not required. Either “1” or “2” above must be applied when evaluating temperature increases. 4. The temperature taken prior to starting the first unit should be used as a base temperature for "add on" units. E. Suspected Reactions and Reaction Workup - If a nurse notes any symptoms suggesting a reaction, she must follow the protocol below: 1. Allergic urticarial reactions, (i.e., local erythema, hives, and itching when not accompanied by fever or any other adverse effects) are the only type of transfusion reaction for which it is not necessary to discontinue transfusion. The infusion should be interrupted and an antihistamine administered. After relief of symptoms, the transfusion is continued slowly. The Blood Bank must be notified that the patient has had an urticarial reaction, but a reaction workup is not necessary. 2. For any other type of Transfusion Reaction - STOP THE TRANSFUSION IMMEDIATELY. If using a straight recipient set, close the clamp on the recipient set. DO NOT REMOVE RECIPIENT SET FROM BAG. Remove tubing from needle hub maintaining sterility of tubing and unit and attach a covered sterile needle. DO NOT REMOVE IV NEEDLE FROM ARM. Keep vein open by adding IV normal saline (0.9% NaCl) using a new set. Any pre-ordered IV solution may also be used. If a "Y" type recipient set is being used, clamp off the blood line and open the clamp on the saline to K.V.O. rate. Recheck transfusion tag and blood label on patient ID band for any errors. 3. Immediately notify the attending physician or resident for evaluation. Also notify the Transfusion Service Lab. A post-transfusion blood sample (1 purple top tube) must be drawn. The specimen, a Blood Bank requisition, the unit and attached tubing and saline must be sent to the Transfusion Service Lab for performance of a STAT investigation. After the transfusion is discontinued, K.V.O. with pre-ordered IV solution or saline. NOTE: The post transfusion blood sample is evaluated to determine if a clerical error, ABO incompatibility, or other antigen- antibody mismatches have occurred with RBC transfusions. If reactions are suspected with platelet transfusions, the product must be stopped, the physician and Blood Bank must be notified, and the transfusion tag must be completed appropriately to document the reaction, but a blood sample need not be drawn because RBC hemolysis is not involved. 4. An accurate account of the reaction must be recorded in the patient's chart. The following must be charted on the "Ancillary and Nursing Patient Progress Report": a. Patient symptoms and/or complaints b. Time reaction occurred and blood product discontinued c. Time and type of IV solution administered d. Time I.V. nurse or Transfusion Service Lab notified and post-transfusion specimens were collected e. Time physician notified, name of physician, and whether orders were received. f. Amount, results of visual inspection, and time of all voiding (NOTE: Technologist may request specimens be sent for routine urinalysis as part of reaction workup). 5. Upon completion of the Stat Investigation; the technologist will call the floor nurse to check on the patient's condition, obtain results of visual inspection of urine, and report the remainder of the results of the Stat Investigation. 6. If there is no evidence of a hemolytic transfusion reaction or bacterial contamination, no further work will be performed. The results of the Stat Investigation will be reviewed by the Medical Director of the Transfusion Service Lab and a written summary report will be placed on the patient's chart. 7. If there is any evidence of a hemolytic transfusion reaction or bacterial contamination, the technologist will request that the unit nurse initiate baseline studies for either hemolytic reactions, bacterial reactions or both. 8. Criteria upon which the technologist will base this request are: a. Evidence of a clerical error that results in a hemolytic reaction b. Positive direct antiglobulin test on a post-transfusion specimen and subsequent recovery of an antibody when none was present in the pre-transfusion sample. c. Evidence of hemolysis in the plasma and serum of post transfusion specimens d. Any symptoms suggestive of a hemolytic reaction such as pain in the flank or back, burning sensation along vein in which blood is infused, or excessive oozing in patients under anesthesia. If any of the above criteria are noted, consult a physician and administer 40 mg of Lasix IV Stat. 9. Directions for all forms used in ordering baseline studies are: a. All tests must be ordered STAT. b. When using a manual requisition, the following must be written above the patient's name: "Transfusion Reaction Evaluation" -- This will clearly identify results as part of the baseline study so tests will not be charged to the patient. c. The transfusion reaction work-up may also be ordered directly through CCS. d. All tests must be drawn Stat and may be collected by a member of the Phlebotomy Team. e. All forms and specimens must be sent to the labs in which the tests are performed. 10. Directions for initiating the baseline studies for a hemolytic reaction are as follows: a. Blood Bank Studies - Order STAT, a Type and Screen using a Requisition by checking the box marked Transfusion Reaction Evaluation. One EDTA (purple top) tube must be sent to the Transfusion Service Lab. This specimen is for additional testing not performed during the STAT Investigation. b. Chemistry Studies - The following chemistry tests should be drawn STAT: i. Bilirubin (a second sample must be collected 5-7 hours after the transfusion). ii. BUN (urea nitrogen) iii. Creatinine iv. Serum Haptoglobin v. Plasma Hemoglobin A routine Chemistry form may be used to order the bilirubin, BUN, and Creatinine. A Special Chemistry form may be used to order the plasma hemoglobin and serum haptoglobin, or orders you placed through CCS. c. Coagulation Studies - Order a STAT DIC workup using a Routine Coag form or CCS orders. Two citrate (blue top) tubes, an EDTA (purple top) tube, and an FSP tube should be sent to the Coag Lab. d. Urinalysis - Collect the first voided post-transfusion urine and send to Chemistry for a STAT Urinalysis. When ordering, request a routine urinalysis including microscopic examination. 11. The standing order for baseline studies of a bacterial reaction consists of a STAT Blood Culture on the patient. 12. Directions for initiating the baseline studies for a bacterial reaction are as follows: Order a Blood Culture to be drawn STAT. Use the Microbiology form, check the box for blood specimen, and write on the line - Transfusion Reaction, or enter through CCS. 13. Results of any baseline study will be charted on the patient's chart. After all tests have been completed, the results will be reviewed by the Medical Director of the Transfusion Service Lab and interpretation of the results will be placed on the patient's chart. Outpatient Transfusion 1. 2. 3. 4. 5. 6. 7. Outpatient transfusions will be performed in the Ambulatory Infusion Center (AIC) during normal operating hours, Monday through Friday. If the AIC is unavailable or if a patient's condition requires, the patient may be admitted to an out-patient bed for transfusion. These patients are not to be admitted or held overnight unless a transfusion reaction occurs and the physician in charge orders the admission. The staff nurse will notify admitting after receiving the physician's admission order. Outpatient transfusions in the AIC will be scheduled after the AIC nurse receives the physician's order. Transfusions in the AIC are performed following AIC procedures. Outpatient transfusions that require a hospital bed must be ordered by the physician or physician's office through the admitting office. Admitting will prepare the outpatient registration and chart, and will also notify the patient when to arrive at the admitting office. Patients in a hospital bed will be transfused following procedure found in the Nursing Procedure Manual for Blood/Blood Products.